Uhl's disease, also known as Uhl anomaly, is a rare disease secondary to selective but uncontrolled apoptosis of right ventricular myocytes during the perinatal period, after complete cardiac development, leading to the absence of right ventricular myocardium and the direct apposition of endocardium to epicardium without a myocardial layer in between, resulting in right ventricular failure.
The present paper describes a case of Uhl's disease with an uncommon presentation. A 28-year-old man was admitted with dyspnea and cyanosis. Transthoracic echocardiography showed severe dilation of the right chambers, impaired right ventricular systolic function and a large ostium secundum atrial septal defect (ASD). Cardiac catheterization revealed pulmonary hypertension, with increased pulmonary capillary wedge pressure (mean 19mmHg) and Qp:QS 0.88:1. At this point, the authors considered that a main diagnosis of ASD could not explain the clinical features and hemodynamic data. A primary disease of the right ventricle was the most likely hypothesis and cardiac magnetic resonance imaging was performed, which demonstrated an extremely thin-walled right ventricle, with almost complete absence of right ventricular free wall myocardium, compatible with Uhl's disease.
A anomalia de Ulh é uma doença rara, secundária à seletiva, contudo descontrolada apoptose dos miócitos do ventrículo direito durante o período perinatal, após o desenvolvimento cardíaco completo, o que explica a ausência de miocárdio do ventrículo direito e a direta aposição do endocárdio e epicárdio, resultando em falência do ventrículo direito. O presente artigo descreve um caso de doença de Uhl com apresentação incomum. Homem de 28 anos admitido por dispneia e cianose. O ecocardiograma transtorácico documentou dilatação grave das cavidades direitas, compromisso da função sistólica do ventrículo direito e uma grande comunicação interauricular ostium secundum. O cateterismo cardíaco revelou hipertensão pulmonar com aumento da pressão capilar (média 19mmHg); Qp:Qs 0,88:1. Neste momento, os autores consideraram que a comunicação interauricular como diagnóstico principal não explicava a apresentação clínica e os dados hemodinâmicos. Doença primária do ventrículo direito tornou-se a hipótese mais provável, pelo que se realizou uma ressonância magnética cardíaca que demonstrou um ventrículo direito com parede extremamente fina, com ausência praticamente total do miocárdio da parede livre, compatível com doença de Uhl.
Uhl's anomaly was first described by Osler in 1905. The exact incidence of this rare condition is unknown. In 1993, Gerlis et al. concluded that many cases of arrhythmogenic right ventricular dysplasia (ARVD) were incorrectly classified as Uhl's anomaly. In said paper, the authors discussed 84 real Uhl's disease cases, and since then fewer cases have been reported.1 Uhl's anomaly is a rare disease secondary to the selective but uncontrolled apoptosis of right ventricular myocytes during the perinatal period, following complete cardiac development. This explains the absence of the right ventricular myocardium and the direct apposition of endocardium to epicardium without a myocardial layer in between, resulting in right ventricular failure.2
Furthermore, some studies suggest that the overexpression of vascular endothelial growth factor may play a role in impairing the development of the right ventricular myocardium.3
In Uhl's disease, the absence of the right ventricular myocardium leads to a lack of contraction and, consequently, the chamber acts as a transition zone between the right atrium and pulmonary artery. Pulmonary circulation is maintained by the pumping action of the right atrium, whereas the right ventricle (RV) balloons aneurysmally in systole. The right atrium is enormous in size.4
In the past, diagnosis was performed during autopsy. However, nowadays, given the development of imaging techniques, diagnosis is carried out via echocardiography or more sensitive and specific cardiac magnetic resonance (CMR) imaging.4 Moreover, there are also published cases where diagnosis took place during prenatal screening.5
Case reportThe authors report the case of a 28-year-old man, with no known heart disease and an insignificant personal and family medical history. However, he did note that he had suffered cyanosis over the past three years, which was never investigated, and had no other symptoms. The patient was admitted to the hospital due to a respiratory infection, presenting with fever, dyspnea and hypoxemia (peripheral oxygen saturation of 55%).
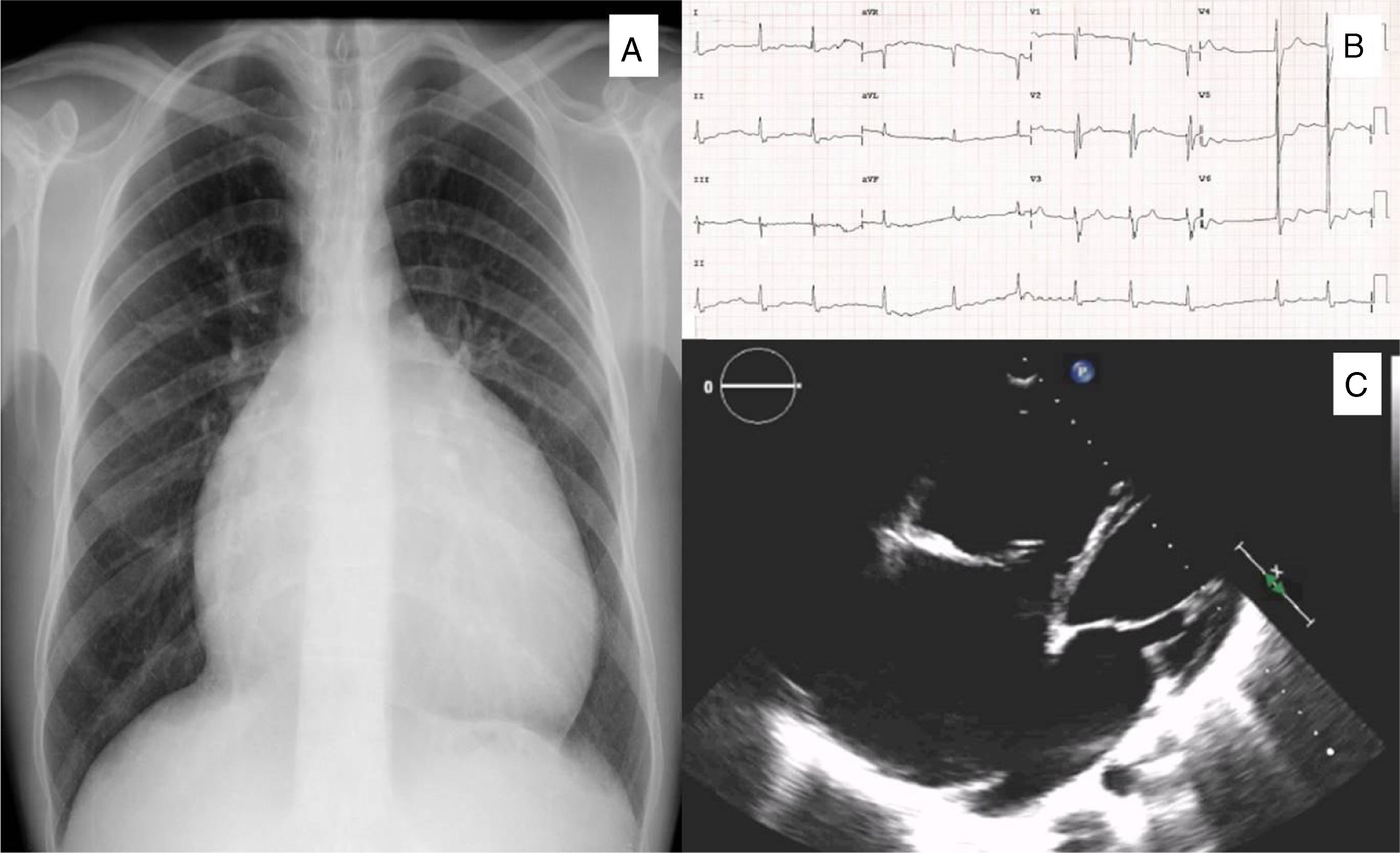
Electrocardiogram (ECG) showed atrial fibrillation (±77 bpm), right bundle branch block and a fragmented QRS complex – despite normal left ventricular activation, right ventricular depolarization was delayed and prolonged (Figure 1).
A: Chest X-ray revealing cardiomegaly with no pulmonary artery dilatation; B: Electrocardiogram showing atrial fibrillation and right bundle branch block. C: Transthoracic echocardiography showing severe right chambers dilation, particularly of the right atrium, and a large ostium secundum atrial septal defect.
A chest X-ray revealed cardiomegaly, with a narrow vascular pedicle (Figure 1). Computed tomography of the chest showed dilated right heart chambers, inferior vena cava and hepatic veins, with no dilatation of the pulmonary artery. Pulmonary ventilation/perfusion scintigraphy ruled out a pulmonary embolism and indicated a right-to-left shunt. Transthoracic echocardiography confirmed severe dilation of the right heart chambers and impaired right ventricular systolic function (Figure 1); a tricuspid valve with normal implantation and moderate regurgitation; an estimated pulmonary artery systolic pressure of 36 mmHg; a normal pulmonary artery diameter; and a large ostium secundum atrial septal defect (ASD) (38 mm), confirmed by transesophageal echocardiography.
Cardiac catheterization was performed, revealing an absence of gradient between the RV and pulmonary artery and post-capillary pulmonary hypertension (mean pulmonary artery pressure of 32 mmHg, with an elevated pulmonary capillary wedge pressure of 19 mmHg). A pulmonary blood flow:systemic blood flow ratio of 0.88:1 was also calculated.
At this point, the authors felt that ASD as the primary diagnosis could not explain the clinical features or hemodynamic data. On one hand, there was no anomalous venous return to justify the cyanosis and mild postcapillary pulmonary hypertension was not compatible with Eisenmenger's syndrome and the consequent right-to-left shunt. On the other hand, there was no evidence of a significant past or present left-to-right shunt, since the pulmonary artery was normal in size.
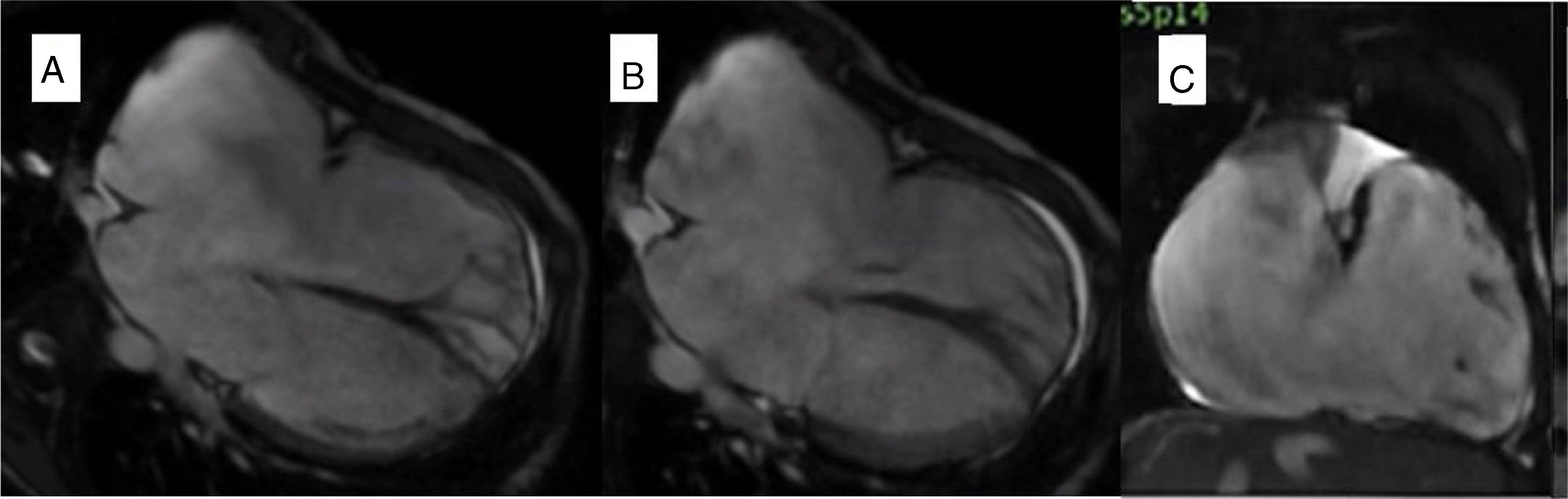
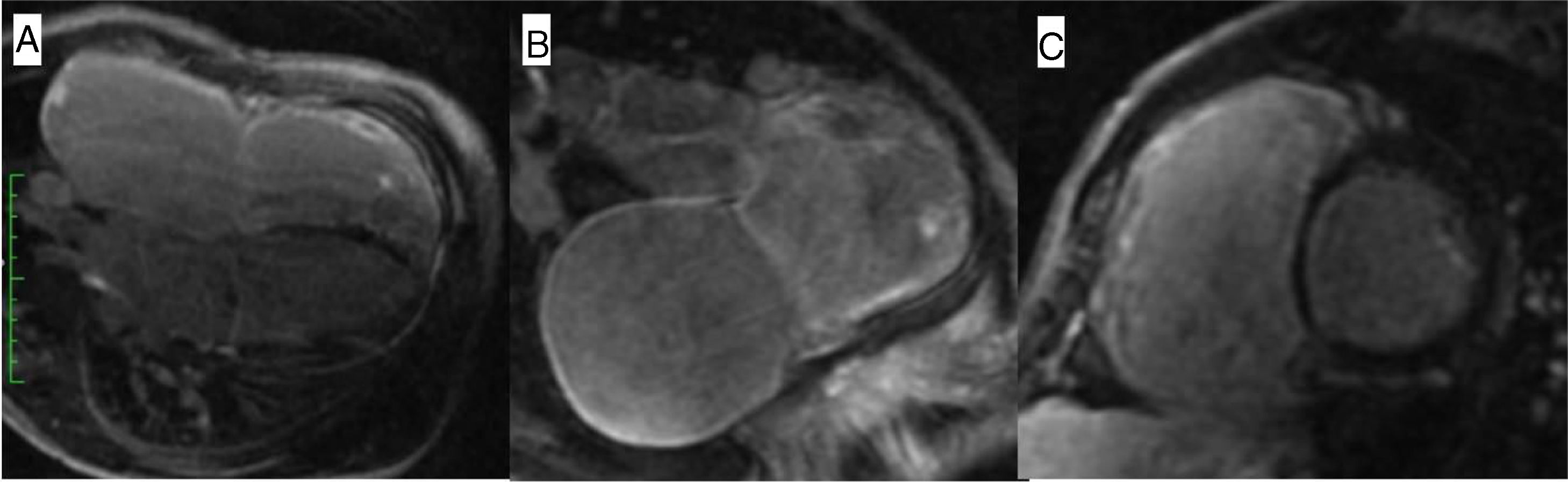
Primary right ventricular disease was the most likely hypothesis and CMR was performed, revealing severe dilation of the right atrium (91×72 mm) and right ventricle (end-diastolic volume 355 ml, 207.9 ml/m2), an extremely thin-walled RV with almost complete absence of the right ventricular free wall myocardium, a paucity of apical trabeculations and impaired systolic function (ejection fraction [EF] 25%) (Figure 2). The left ventricle was dilated with normal wall thickness and an EF of 41%. An ASD measuring over 30 mm was identified and late gadolinium enhancement was observed in the right ventricle and right atrium walls (Figure 3). These findings were compatible with Uhl's anomaly.
Cardiovascular magnetic resonance: Steady-state free precession imaging documenting severe dilation of the right atrium and right ventricle, an extremely thin-walled right ventricle with almost complete absence of the right ventricular free wall myocardium, with a paucity of apical trabeculations, in a four-chamber view in diastole (A) and systole (B), and coronal view (C). An atrial septal defect measuring over 30 mm was also identified.
Cardiopulmonary exercise testing showed a moderate exercise capacity with a peak oxygen uptake of 27.6 ml/kg/min (55% of the value predicted for the patient's gender and age) as well as an oxygen uptake at anaerobic threshold of 20.5 ml/kg/min and a minute ventilation-to-carbon dioxide output slope of 46.2.
The patient initiated anticoagulation therapy with warfarin and received a subcutaneous implantable cardioverter-defibrillator for primary prevention of sudden cardiac death, due to severe right ventricular dysfunction. The patient will be closely monitored and heart transplantation will be considered in the event his functional capacity deteriorates.
DiscussionUhl's disease is characterized by the absence of the RV myocardium and the direct apposition of endocardium to epicardium.2
Histological examination confirms cardiac muscle wastage and replacement by fibrous tissue.6 However, despite this anomaly in the RV myocardium, the septal and left ventricular myocardium is preserved.4,7
In severe forms, RV failure develops during childhood, with pulmonary circulation being dependent on the right atrium. Cyanosis is also present in the event of an atrial shunt.4
Prior to the advent of current imaging methods, diagnosis was performed during autopsy. Nowadays, CMR is the method of choice for diagnosis, as well as for morphologic and functional evaluation.4
The association of Uhl's disease with other congenital heart defects had rarely been reported, namely with tricuspid valve dysplasia or absence, Ebstein's anomaly, pulmonary atresia or regurgitation, patent ductus arteriosus, ASD and hypoplasia of the mitral valve and left ventricle.1,8–12
A differential diagnosis should be performed with ARVD. From a histological point of view, ARVD is characterized by fibrofatty infiltration of the right ventricular free wall which is absent in Uhl's disease, where fibrosis predominates.13 Unlike ARVD, the major clinical finding in Uhl's disease is heart failure, rather than arrhythmic events and sudden death.6,10 Family history is also more common in ARVD than in Uhl's disease.10
Regarding electrocardiographic studies, in ARVD, T-wave inversions in V1 and V2 are noted, along with Epsilon waves. Uhl's disease, on the other hand, presents a fragmented QRS complex.7,13 In CMR, Uhl's disease is characterized by an extremely dilated thin-walled RV with severe hypokinesis, a paucity of trabeculations and no fat signal in the RV wall, as seen in ARVD. In ARVD, focal wall motion abnormalities are more frequent, contrasting with the global hypokinesis seen in Uhl's disease.4,7,13
Ebstein's anomaly should also be considered in differential diagnosis. In Uhl's disease the tricuspid valve hinges normally and is not dysplastic.4
With regard to surgical treatment, a right heart bypass can be performed. However, this procedure carries a risk of clots forming in the right ventricle as well as embolization, particularly in the presence of a bidirectional Glenn shunt.14 Another option involves almost entirely resecting the RV free wall.15 Possible complications include recurrent ventricular dilatation and arrhythmias. In these cases, a residual RV free wall must be ruled out and a total cavopulmonary connection performed.16
If clinical deterioration persists, the treatment approach should be orthotopic cardiac transplantation.17
In our case, the association of RV myocardium disease with a large ASD explains the patient's unique clinical evolution.
Cyanosis in the presence of an ASD (with a “normal” RV) may occur in two circumstances that were not present in this case: severe pulmonary hypertension with Eisenmenger's syndrome and the consequent right-to-left shunt, or when an anomalous systemic venous return exists.
Furthermore, the lack of pulmonary artery dilation shows that, although the ASD is large, there was probably no significant left-to-right shunt. The inexistence of such a shunt is due to the fact that a shunt is dependent of the compliance of both ventricles in ASDs, and in this case only the RV was affected. Over the years, progressive RV dysfunction led to a right-to-left shunt and consequent cyanosis. Moreover, the defect acts as an escape, which has until now prevented the occurrence of overt right-sided heart failure.
The ECG is also notable, with a fragmented QRS complex, reflecting the delay and prolongation of right ventricular depolarization.
In conclusion, this case shows that clinical symptoms, hemodynamic data and imaging findings must be comprehensively and thoroughly reviewed in congenital heart disease in order to enable correct diagnosis. Primary RV disease should be considered when RV failure is present in the absence of valve disease and pulmonary hypertension. Uhl's anomaly is a rare disease that consists in the absence of the RV myocardium and progressive RV failure.
Conflicts of interestThe authors have no conflicts of interest to declare.