A single coronary artery is one of the most rarely seen coronary artery anomalies. In addition, the specific subtype (Lipton RII-A) that our patient presented is one of the least common, and its clinical presentation as myocardial infarction and cardiac arrest has not been described in the literature. The case shows that although it is essential to exclude a malignant interarterial course of the vessel, cardiac arrest is a possible clinical presentation produced by myocardial ischemia in the context of acute myocardial infarction and should be managed according to clinical practice guidelines.
Uma artéria coronária única é uma das anomalias mais raras das artérias coronárias. Além disso, o subtipo específico (Lipton R-IIA) presente no nosso doente é um dos menos frequentes e a sua apresentação clínica como enfarte do miocárdio e como paragem cardíaca não foi ainda descrita na literatura. O caso mostra que, embora o descarte de um percurso interarterial maligno do vaso seja essencial, a paragem cardíaca é uma apresentação clínica possível causada por isquemia do miocárdio no cenário de um enfarte agudo do miocárdio, que deverá ser tratada de acordo com as recomendações práticas clínicas.
We present a 51-year-old male with hypertension and dyslipidemia admitted to a regional hospital for chest pain at rest. The initial electrocardiogram showed a 1.5 mm ST-segment depression. Initial laboratory tests showed mild troponin elevation. Antithrombotic treatment with aspirin, clopidogrel and enoxaparin was administered and intravenous nitroglycerin achieved pain relief and normalization of the electrocardiogram. With a diagnosis of high-risk non-ST-elevation myocardial infarction, according to the recommendations of the clinical practice guidelines,1 an early invasive strategy was planned with coronary angiography within 24 hours of hospital admission. Suddenly, four hours after admission, the patient experienced cardiac arrest in ventricular fibrillation. Advanced cardiopulmonary resuscitation was performed and after five defibrillations, he recovered sinus rhythm with inferior ST elevation. The patient was transferred to our center for primary percutaneous coronary intervention.
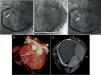
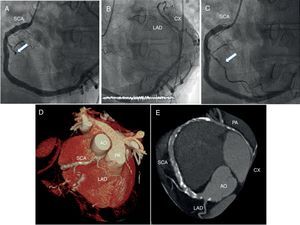
On coronary angiography, a single coronary artery (SCA) originating from the right coronary sinus was observed, which also supplied the territory of the left anterior descending (LAD) and circumflex (CX) arteries (Figure 1A and B; videos 1 and 2). An acute marginal branch had a thrombotic occlusion (Figure 1A; arrow). The acute occlusion was easily crossed with a Runthrough NS® floppy guidewire. Thromboaspiration was attempted but it was impossible to advance the aspiration catheter due to the diffuse disease of the vessel. Simple angioplasty with a semicompliant balloon (2 mm×15 mm) was therefore performed, with recovery of TIMI 3 distal flow (Figure 1C; arrow). We decided not to implant a stent because of diffuse disease and the small diameter of the vessel.
(A and B) Coronary angiography showing a single coronary artery (SCA) originating from the right coronary sinus, also supplying the territory of the left anterior descending (LAD) and circumflex (CX) arteries, and thrombotic occlusion of an acute marginal branch (A, arrow); (C) primary percutaneous coronary intervention recovering distal TIMI 3 flow in the culprit vessel (arrow); (D and E) multislice computed tomography reconstruction. After its origin, the main trunk of the SCA crosses the base of the heart to supply the contralateral coronary artery. Immediately after the origin of this main trunk, it also gives off a small vessel that reaches the anterior interventricular sulcus anteriorly to the aorta (AO) and pulmonary artery (PA) to supply the proximal LAD territory.
The patient evolved well and was promptly extubated. In order to confirm the origin and course of the SCA, multislice computed tomography (MSCT) was performed. It confirmed the existence of an SCA originating from the right sinus. Immediately after the origin of this main trunk, it gave off a small vessel that reached the anterior interventricular sulcus anteriorly to the aorta and pulmonary artery (proximal LAD territory) (Figure 1D). The single common trunk, 7 mm in diameter at its proximal segment, had numerous calcified plaques along its route without significant stenosis. A large left posterolateral branch followed the left atrioventricular groove supplying the nominal CX territory (Figure 1E). Finally, the SCA gave rise to a distal branch on the distal anterior wall of the left ventricle, completing the irrigation of the LAD territory. Given these findings, the SCA was classified as RII-A subtype according to Lipton's classification. Due to the non-malignant course of the SCA, the patient was discharged under medical therapy consisting of dual antiplatelet therapy (aspirin and clopidogrel) for 12 months, atorvastatin, metoprolol and enalapril. After one year of clinical follow-up, he remains asymptomatic, with no further adverse events.
DiscussionAn SCA, defined as an artery that arises from an arterial trunk of a coronary sinus and irrigates the entire myocardium, is one of the most rarely seen coronary artery anomalies (CAA), with an incidence of 0.05%.2,3 The prognosis of patients with SCA varies according to its anatomic distribution and associated coronary atherosclerosis. The majority of these anomalies are diagnosed as incidental findings on coronary angiography. However, 20% of cases are associated with life-threatening symptoms, such as arrhythmias, syncope, myocardial infarction, or sudden death (SD).2 SCAs were classified by Lipton et al.4 according to the site of origin (right or left coronary sinus of Valsalva), the anatomical distribution on the ventricular surface, and the relationship with the ascending aorta and the pulmonary artery. In patients with an SCA and an intra-arterial course, SD may occur when the SCA is compressed between the aorta and pulmonary artery during vigorous exercise.
Coronary angiography is the gold standard for the evaluation of coronary artery disease. However, in the case of CAA, further evaluation by MSCT is recommended to determine the course of the anomaly and prognosis.2,3
To the best of our knowledge this case is the first reported in the literature describing a patient with an RII-A subtype SCA presenting with ST-segment elevation myocardial infarction and cardiac arrest. It should be borne in mind that coronary atherosclerosis is common in CAA, and that its clinical presentation can be as stable coronary artery disease or acute coronary syndromes (ACS). Even after a malignant interarterial course of the SCA is excluded, cardiac arrest is a possible clinical presentation produced by myocardial ischemia in the context of an ACS and should be managed according to clinical practice guidelines.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.