Primary cardiac and pericardial tumors are rare entities with an autopsy frequency of 0.001-0.03%. Metastases to the heart and pericardium are much more common than primary tumors. Malignant pericardial mesotheliomas account for up to 50% of primary pericardial tumors.
We report the case of a 75-year-old woman with hypertension, dyslipidemia and atrial fibrillation who went to the emergency department due to nonspecific thoracic discomfort of over six hours duration associated with syncope. Physical examination revealed a low-amplitude arrhythmic pulse, no heart murmurs and no signs of pulmonary congestion. The ECG revealed atrial fibrillation with ST-segment elevation in V2-V6, I and aVL. The patient was transferred for emergent coronary angiography, which revealed a long stenosis in the mid-distal portion of the left anterior descending artery. The echocardiogram showed a large pericardial effusion with diffuse thickening of the myocardium. Due to worsening hemodynamics, cardiac rupture was suspected and the patient underwent urgent sternotomy and pericardiotomy with drainage of a large quantity of hematic fluid. The surgeons then identified a large, unresectable tumor occupying the distal half of the anterior portion of the heart.
This is, to our knowledge, the first case report of primary pericardial mesothelioma presenting with suspected ST-elevation myocardial infarction. In this case, direct observation of the tumor led to biopsy and the final diagnosis. These are highly malignant tumors and when diagnosed are usually already at an advanced stage.
Os tumores primários do coração e pericárdio são entidades raras, com uma frequência estimada em autópsias de 0,001-0,03%. A metastização do coração e pericárdio é muito mais comum do que os tumores primários. O mesotelioma maligno do pericárdio pode atingir 50% dos casos de tumores primários do pericárdio.
Mulher de 75 anos, com hipertensão arterial, dislipidemia e fibrilhação auricular. Recorreu ao serviço de urgência por desconforto torácico inespecífico, com mais de seis horas de duração, associado a síncope. No exame objetivo foi detetado pulso arrítmico de baixa amplitude, ausência de sons cardíacos, sem sinais de congestão pulmonar. O ECG mostrou fibrilhação auricular e elevação do segmento ST em V2-V6, I e aVL. A doente foi transferida para angiografia coronária urgente, que mostrou estenose na porção médio-distal da artéria descendente anterior esquerda. O ecocardiograma revelou derrame pericárdico de grande volume com espessamento difuso do miocárdio. Devido a agravamento hemodinâmico, houve suspeita de rutura cardíaca e a doente foi submetida a esternotomia e pericardiotomia emergentes, com drenagem de grande quantidade de líquido hemático. Foi observada existência de volumoso tumor irressecável, ocupando a metade distal da face anterior do coração.
O nosso caso é o primeiro, de que temos conhecimento, que descreve um caso de mesotelioma do pericárdio primário que se apresenta como suspeita inicial de enfarte do miocárdio com supra-ST. Neste caso, a observação direta do tumor permitiu a realização de biopsia e o diagnóstico final. Estes tumores são altamente malignos e, quando diagnosticados, estão habitualmente num estádio avançado.
Primary cardiac and pericardial tumors are rare entities with an autopsy frequency of 0.001-0.03%.1 Metastases to the heart and pericardium are much more common (100-1000 times) than primary tumors, with the underlying malignant origin, in most cases, being carcinoma of the lung.2 Primary cardiac tumors present with one or more symptoms of the classic triad of cardiac symptoms and signs resulting from intracardiac obstruction, signs of systemic embolization, and systemic or constitutional symptoms.3 Unlike primary malignant cardiac tumors, which account for up to 25% of cases, malignant pericardial mesotheliomas account for up to 50% of primary pericardial tumors. The mean age of presentation is 46 years and they are twice as common in males than in females. We present the case of a patient with a primary pericardial mesothelioma presenting with ST-elevation myocardial infarction.
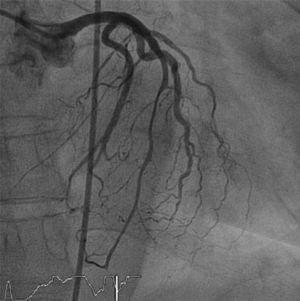
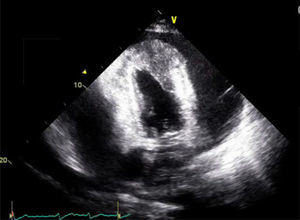
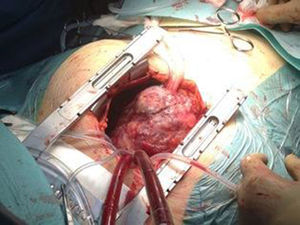
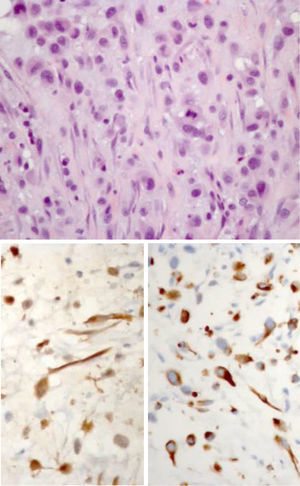
Case reportWe present the case of a 75-year-old Caucasian woman with a previous history of hypertension, dyslipidemia and a left total hip replacement. She was medicated with lisinopril-hydrochlorothiazide, bisoprolol and atorvastatin. Additionally, she was recently diagnosed with atrial fibrillation and was on warfarin. She had no previous symptoms of cardiac disease. She went to the emergency department of the local hospital due to nonspecific thoracic discomfort and malaise of over six hours duration associated with an episode of syncope. She also reported dyspnea on moderate exertion of two weeks duration. A complete blood count (CBC) and biochemistry revealed anemia and thrombocytopenia, with no other changes. The patient denied other signs or symptoms. Physical examination revealed a low-amplitude arrhythmic pulse, no heart murmurs and no signs of pulmonary congestion, blood pressure of 95/56 mmHg, heart rate of 101 beats per minute, and peripheral oxygen saturation of 85%. The CBC revealed anemia (Hg 8.9 g/dl) and thrombocytopenia (80 000 U/l). Biochemistry results revealed elevated serum cardiac troponin I (0.9 ng/ml; normal <0.04 ng/ml). A chest X-ray revealed a cardiothoracic index of >50% with widening of the mediastinum. The ECG revealed atrial fibrillation with ST-segment elevation in V2-V6, I and aVL. The patient was immediately transferred to a tertiary centre for emergent coronary angiography, which revealed a long stenosis of 50% in the mid-distal portion of the left anterior descending artery (with TIMI 3 flow) and a focal 30% stenosis in the mid segment of the right coronary artery (Figure 1). Left ventriculography revealed a hyperkinetic left ventricle and apical akinesia but otherwise normal systolic function. In the minutes after cardiac catheterization, the patient developed hypotension (systolic blood pressure of 85-90 mmHg) and slight chest discomfort persisted. An echocardiogram was performed and revealed a large pericardial effusion with diffuse thickening of the myocardium, mainly in the anterolateral wall and apex, which was assumed to be adherent fibrin (Figure 2). Due to worsening hemodynamic status and echocardiographic findings in a patient with chest pain, ST-elevation on the ECG and elevated cardiac troponin, cardiac rupture was suspected and the patient underwent urgent sternotomy and pericardiotomy with drainage of a large quantity of bloody fluid followed by hemodynamic recovery. The surgeons then identified a large unresectable tumor occupying the distal half of the anterior portion of the heart, which was biopsied (Figure 3). The patient was admitted to the cardiothoracic intensive care unit and was extubated on day 2 after surgery, and was then transferred to an intermediate care unit, with a favorable clinical status. A cervical-thoraco-abdominal-pelvic computed tomography (CT) scan was performed that identified myocardial tumor infiltration (measuring 6 cm×7 cm×11 cm) and pulmonary, cervical and abdominal wall metastases. The pathological study revealed a malignant mesothelioma. The immunohistochemical study documented diffuse expression of AE1/AE3, vimentin and MDM2 in tumor cells and focal expression of calretinin, EMA, podoplanin, desmin and p53 (Figure 4).
An oncological group meeting decided to start chemotherapy with pemetrexed and carboplatin on the eighth day of hospitalization. The patient was transferred to the medical oncology department after 14 days of hospitalization (sixth day of chemotherapy). She remained clinically stable but showed a gradual deterioration in her general condition, with anorexia and asthenia, and died suddenly on the 30th day of hospitalization.
DiscussionThis is, to our knowledge, the first case report of primary pericardial mesothelioma presenting with suspected ST-elevation myocardial infarction (STEMI).
Primary cardiac tumors are rare entities, with an estimated prevalence of 0.001-0.056%.1,4 Primary pericardial tumors are even rarer, with an estimated prevalence of 0.001-0.007%.5 These can be benign (teratoma, fibroma, angioma, lipoma) or malignant (mesothelioma, sarcoma). Pericardial mesothelioma is extremely rare, although it is the most common primary malignant pericardial tumor, accounting for 50% of primary pericardial tumors. Its incidence was 0.0022% among 500 000 cases in a large necropsy study.6 Metastatic tumors are much more common, arising mostly from the lung, breast, skin or blood (lymphoma or leukemia).2,6 Age at presentation ranges from 2 to 78 years and they are more frequent in men (2:1 male to female ratio).
Common clinical manifestations of pericardial mesothelioma include heart failure (due to cardiac tamponade, constrictive pericarditis and in some cases myocardial infiltration); pericardial effusion and ischemic cardiac pain (angina) may also be present due to coronary artery compression by the tumor. The onset of symptoms is usually insidious. Distant metastasis, conduction block due to myocardial infiltration and tumor embolism causing neurological deficits have also been reported.7,8
Pericardial mesotheliomas usually grow as a bulky mass that encircles the heart with few foci of myocardial infiltration. Magnetic resonance imaging (MRI) and CT are useful in showing the extent of involvement of contiguous structures and the degree of constriction.
In several case reports the most common mode of presentation of pericardial mesothelioma was the development of pericarditis that evolved to constrictive pericarditis,9–11 sometimes associated with a circumferential pericardial effusion for which diagnostic pericardiocentesis was not conclusive.12 In the case presented, the clinical presentation was sudden, mimicking an anterior wall STEMI. The suspicion of left ventricular rupture was founded on the observation of a pericardial effusion, with a suspected large quantity of fibrin adjacent to the myocardium, associated with hypotension, indicating cardiac tamponade. As previously described, the sensitivity of echocardiography in the identification of pericardial mesothelioma is low,13 and CT scanning and MRI are preferable since these techniques not only detect invasion of adjacent structures and the presence of metastases but also, in the case of MRI, can assess the presence of constriction and ventricular dysfunction.6
In this case, direct observation of the tumor led to biopsy and the final diagnosis. At the histological level, pericardial and pleural mesotheliomas are similar. The tumor cells can have three distinct patterns: (1) predominance of epithelioid cells; (2) predominance of fibrous (spindle) cells; and (3) mixed-type (which was the pattern observed in this case).14 Unlike pleural mesothelioma, which has a well-established association with previous exposure to asbestos, in pericardial mesothelioma this association is less strong, and our patient had no history of present or past contact with asbestos products.15
These are highly malignant tumors and when diagnosed are usually already at an advanced stage. Mesotheliomas respond poorly to radiotherapy and chemotherapy is usually employed to reduce tumor mass. Resection may be curative but only in small, localized tumors.16 Surgical intervention in pericardial mesothelioma is primarily for effusion control, for cytoreduction before multimodal therapy, or to deliver and monitor innovative intrapericardial therapies. Chemotherapy and pericardiotomy (for prevention of cardiac tamponade and relief of constriction) are the bases of palliative care. A pericardial window can be formed to introduce chemotherapeutic agents.
With regards to prognosis, survival is extremely low, between 3.5 and 6 months after diagnosis. The most common causes of death are cardiac tamponade and heart failure.17
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.