Mesalamine is a common treatment for Crohn's disease, and can be rarely associated with myocarditis through a mechanism of drug hypersensitivity. We present the case of a 19-year-old male who developed chest pain two weeks after beginning mesalamine therapy. The electrocardiogram showed slight ST-segment elevation with upward concavity in the inferolateral leads; blood tests demonstrated elevated troponin I and the echocardiogram revealed moderately depressed left ventricular systolic function with global hypocontractility. Cardiac magnetic resonance imaging confirmed the diagnosis of myocarditis, revealing multiple areas of subepicardial fibrosis. The onset of symptoms after mesalamine, and improvement of chest pain, cardiac biomarkers and left ventricular systolic function after discontinuing the drug, suggest that our patient suffered from a rare drug-hypersensitivity reaction to mesalamine.
A mesalamina é um tratamento comum para a doença de Crohn, associando-se de forma rara à miocardite aguda, através de uma reação de hipersensibilidade ao fármaco. Os autores apresentam o caso clínico de um jovem de 19 anos com aparecimento de dor torácica duas semanas após ter iniciado tratamento com mesalamina para a doença de Crohn. O eletrocardiograma mostrou um discreto supradesnivelamento do segmento ST, de concavidade ascendente, nas derivações infero-laterais; as análises revelaram elevação da troponina I e o ecocardiograma exibiu uma depressão moderada da função sistólica do ventrículo esquerdo, por hipocontractilidade global. A ressonância magnética cardíaca confirmou o diagnóstico de miocardite, evidenciando múltiplas áreas de fibrose subepicárdica. O início dos sintomas após o começo da mesalamina e a melhoria da dor torácica, biomarcadores cardíacos e função sistólica ventricular esquerda após a suspensão do medicamento, sugerem que o nosso paciente teve uma reação rara de hipersensibilidade à mesalamina.
Mesalamine (5-aminosalicylic acid) is a well-known treatment for inflammatory bowel disease, often used as the first-line drug. Although rare, adverse cardiac reactions due to mesalamine have been described in the literature, and include pericarditis, myocarditis, coronary vasculitis and left ventricular dysfunction.1–4 We report a case of mesalamine-induced myocarditis in a patient with a recent diagnosis of Crohn's disease.
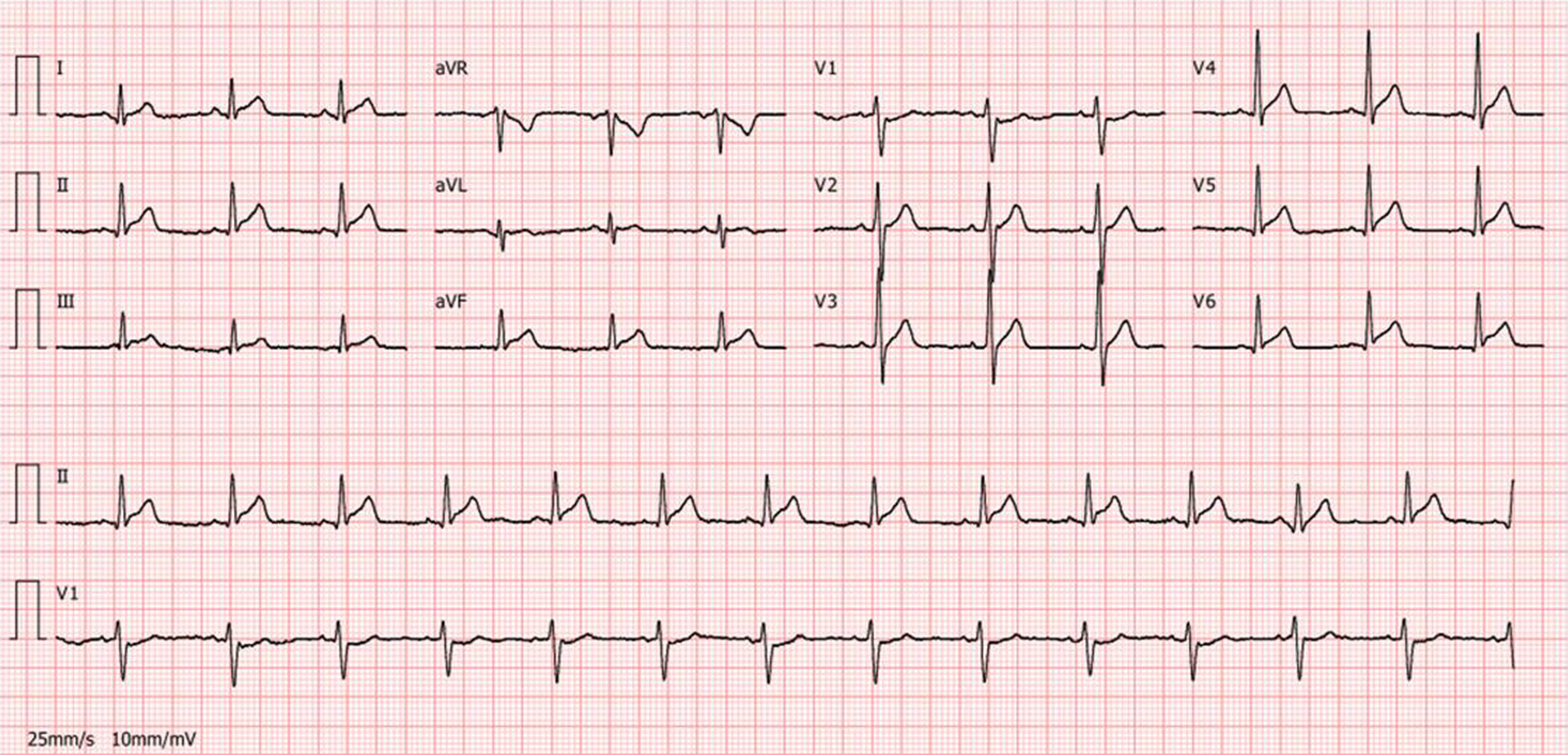
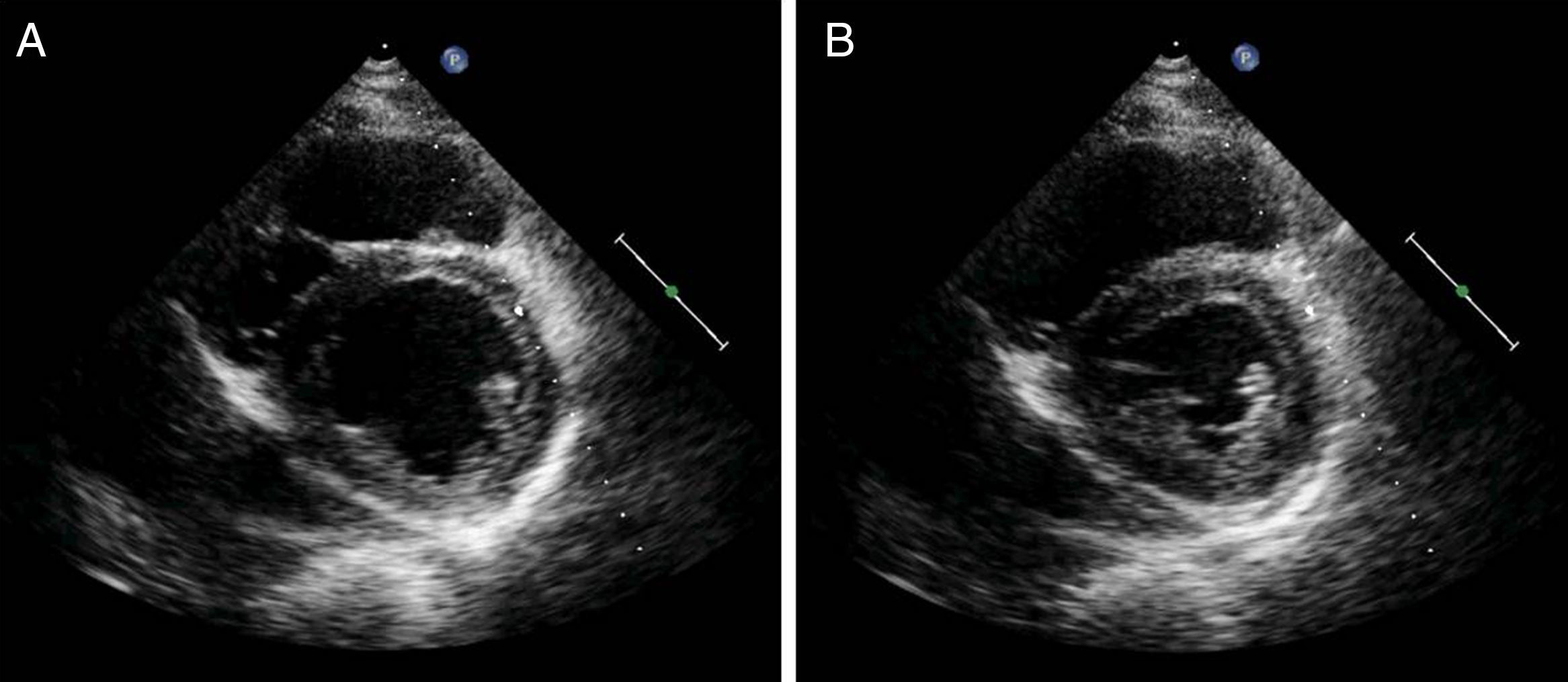
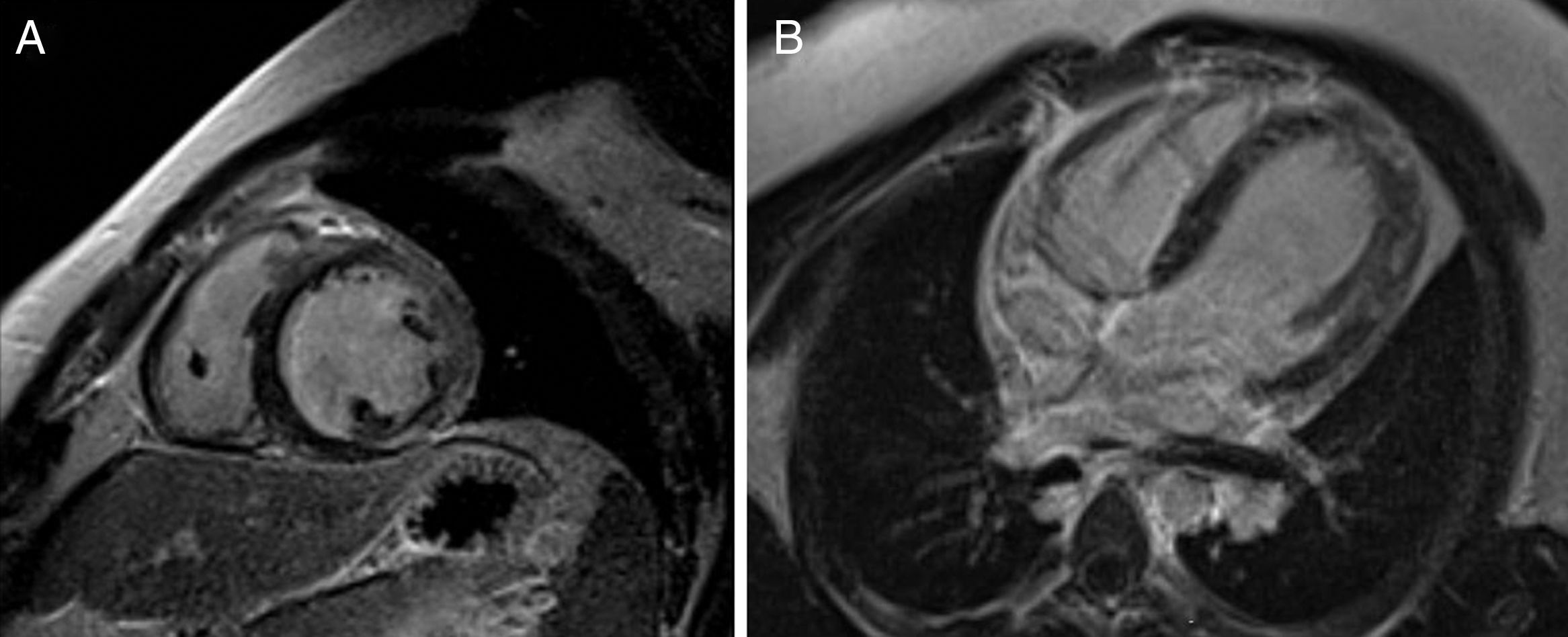
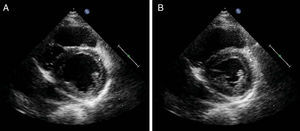
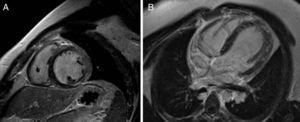
Case reportA 19-year-old male with no relevant medical history, besides having been diagnosed two weeks previously with Crohn's disease for which he was medicated with mesalamine 1500 mg twice a day and budesonide 9 mg daily, was admitted to the local hospital with retrosternal chest pain radiating to the left arm. He reported no accompanying symptoms and no relieving or aggravating factors were identified. The patient had no reported previous infection. The physical examination was unremarkable and there were no signs of hemodynamic instability or heart failure. The initial 12-lead electrocardiogram revealed sinus rhythm and slight ST-segment elevation with upward concavity in leads I, II, III, aVF and V3–V6 (Figure 1). As laboratory tests showed elevated cardiac necrosis biomarkers (troponin I 9.1 ng/ml), he was transferred to our hospital for cardiological evaluation. Following admission to the cardiac care unit, he mentioned some episodes of chest pain which improved after treatment with aspirin. Repeated blood tests demonstrated a further increase in cardiac biomarkers (peak troponin I 27.3 ng/ml and peak total CK 915 IU/l) accompanied by elevation of NT-proBNP (6413 pg/ml) and inflammatory parameters (C-reactive protein 130 mg/l, 15800 leukocytes). Remodeling therapy with ACE inhibitors and beta-blockers was also introduced, due to the moderately depressed left ventricular systolic function (ejection fraction of 38%) seen on the transthoracic echocardiogram, with global hypocontractility, although more noticeable in the posterior, inferior and lateral walls (Figure 2). Cardiac magnetic resonance imaging (MRI) with delayed gadolinium enhancement revealed multiple areas of myocardial fibrosis, mainly subepicardial, suggesting a non-ischemic pattern (Figure 3). There was no sign of myocardial infarction and the patient was therefore diagnosed with acute myocarditis.
In view of mesalamine's cardiovascular toxicity as described in the literature, this drug was discontinued shortly after admission. The patient remained asymptomatic thereafter and laboratory tests were favorable (NT-proBNP 905 pg/ml and troponin I 0.13 ng/ml at discharge). Electrocardiograms showed progressive resolution of ST-segment elevation and the echocardiogram was repeated one week later, demonstrating improvement in left ventricular systolic function (ejection fraction of 45%).
DiscussionClassic myocarditis refers to inflammation of the heart muscle as a result of exposure to either discrete external antigen triggers, such as viruses, bacteria, parasites or drugs, or to internal triggers such as autoimmune activation against self-antigens. Drugs can act as a direct toxic agent (anthracyclines and cocaine) or by a hypersensitivity reaction, as is thought to be the case with mesalamine and other medications (clozapine, sulfonamides, cephalosporins, penicillins and tricyclic antidepressants).5
Cardiac disease can be associated with Crohn's disease as an extraintestinal manifestation of inflammatory bowel disease or as a consequence of drug-induced side effects.1–4 Myocarditis associated with mesalamine is a rare but potentially serious phenomenon, generally occurring 2–4 weeks after the initial exposure to the drug, although presentation may be delayed over years, especially if steroids are used concomitantly.6 Mesalamine's mechanism of action is not fully understood, but it includes inhibition of the cyclooxygenase pathway, inducing an anti-inflammatory effect in the colon. The exact mechanism for mesalamine-induced myocardial inflammation is not clearly identified, but it is thought to be a hypersensitivity reaction rather than a cytotoxic effect.1,2 One proposed mechanism is humoral-mediated hypersensitivity, in which antibodies formed against mesalamine cross-react with cardiac tissue causing inflammation.6 The diagnosis of hypersensitivity myocarditis is supported by two facts: inflammation worsens if mesalamine is reintroduced during the acute phase,1 and resolution of symptoms occurs within one week after drug discontinuation, as has been described in all reported cases.1–4 Eosinophilic infiltration of the myocardium on endomyocardial biopsy has also been described,7 which seems to confirm the link between mesalamine and hypersensitivity myocarditis.
In our case, the onset and resolution of symptoms were similar to those reported in the literature. Soon after discontinuing mesalamine, our patient evolved well, with progressive falls in cardiac biomarkers and improvement in left ventricular systolic function. Considering this evolution and the fact that there was no previous infection, mesalamine-induced myocarditis was considered to be the most likely diagnosis.
ConclusionThis case illustrates the importance of eliciting a thorough medical history and being aware of the timing when new medications are started. It is imperative that any new onset of chest pain in the setting of inflammatory bowel disease treated with mesalamine should be evaluated via cardiac enzymes, electrocardiogram, echocardiogram and possibly cardiac MRI to rapidly diagnose any complication caused by either the inflammatory bowel disease itself or an adverse drug reaction.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflict of interestsThe authors have no conflict of interests to declare.