The present report concerns a 54-year-old man with refractory angina who was referred for lipoprotein(a) [Lp(a)] apheresis (LA) because of Lp(a)-hyperlipoproteinemia. At 18-month follow-up, myocardial perfusion, assessed with stress cardiac magnetic resonance, was shown to improve, with progressive amelioration of anginal symptoms.
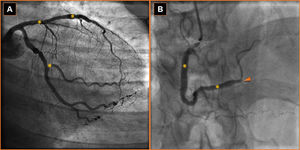
The patient began to suffer effort angina at the age of 53. In one year he had undergone multiple percutaneous coronary artery revascularizations, with chronic occlusion of the posterior descending artery (Figure 1). At his first admission to our lipid clinic, he was diagnosed with Lp(a)-hyperlipoproteinemia and polygenic hypercholesterolemia. He was receiving ranolazine 750 mg twice daily, aspirin 100 mg once daily, clopidogrel 75 mg once daily, and irbesartan 300 mg once daily. In the 6-min walk test angina appeared at 450 m; a baseline Seattle Angina Questionnaire (SAQ)1 was recorded. Carotid artery Doppler examination revealed intimal medial thickness <1 mm with 30% stenosis at the sinus bilaterally.
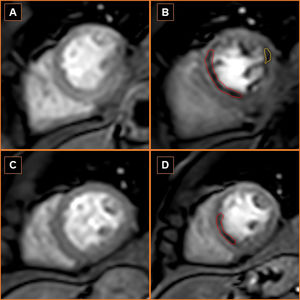
Considering the role of Lp(a)-hyperlipoproteinemia in the pathogenesis of refractory angina, LA was started2 and was repeated every two weeks, treating 5000 ml of plasma (about 2.0 times patient plasma volume) per session using dextran sulfate (Liposorber® LA systems; Kaneka) in addition to optimized lipid-lowering therapy (Table 1). Background pharmacological therapy was maintained unchanged. During 18 months of follow-up the patient presented progressive improvement in anginal symptoms: effort angina in the 6-min walk test regressed and an improvement in four of five domains of the SAQ was reported. The follow-up myocardial perfusion scan on stress cardiac magnetic resonance imaging showed improvement in the septal left ventricular wall perfusion defect and resolution of the lateral left ventricular wall perfusion defect (Figure 2).
Patient's lipid profile.
| TC (mg/dl) (120-200) | HDL (mg/dl) (>35) | TG (mg/dl) (<150) | LDL (mg/dl) (<160) | Non-HDL-C (mg/dl) (<130) | TC/HDL ratio (<4.5) | Lp(a) (mg/dl) (<50) | LLT | |
|---|---|---|---|---|---|---|---|---|
| Baseline | 153 | 33 | 167 | 87 | 120 | 4.6 | - | Atorvastatin 40 mg once daily |
| Before LA | 117 | 44 | 73 | 68 | 73 | 2.7 | 92 | Rosuvastatin 10 mg once dailyFenofibrate 145 mg once dailyAcipimox 500 mg once daily |
| After LA | 61 | 41 | 43 | 11 | NA | NA | 15 | Rosuvastatin 10 mg once dailyFenofibrate 145 mg once dailyAcipimox 500 mg once daily |
HDL: high-density lipoprotein; HDL-C: high-density lipoprotein cholesterol; LA: lipoprotein apheresis; LDL: low-density lipoprotein; LLT: lipid-lowering therapy; Lp(a): lipoprotein(a); NA: not applicable; TC: total cholesterol; TG: triglycerides.
Stress and rest perfusion cardiac magnetic resonance (CMR) sequences showing improved perfusion in the left ventricular septal wall perfusion defect (red area) and resolution of the left ventricular lateral wall perfusion defect (yellow area). (A) Baseline rest perfusion CMR; (B) baseline stress perfusion CMR; (C) 18-month follow-up rest perfusion CMR; (D) 18-month follow-up stress perfusion CMR.
Refractory angina is a growing problem worldwide due to improved survival after revascularization procedures.3,4 The case reported supports the hypothesis that Lp(a)-hyperlipoproteinemia is a contributing factor in refractory angina: the apolipoprotein(a) [apo(a)] component of Lp(a) exhibits structural homology with plasminogen, enhances thrombosis and impairs fibrinolysis. Reduction of Lp(a) by LA improves thrombotic and fibrinolytic parameters in patients with refractory angina,5 enables restoration of endothelial function,6 and reduces the incidence of cardiovascular events in patients with Lp(a)-hyperlipoproteinemia.7 In addition, a unified view of Lp(a) in cardiovascular medicine draws attention to the advantages of associating cascade screening with personalized therapy.8
Until apo(a) antisense therapy becomes available, LA may represent an effective long-term treatment for refractory angina in those with Lp(a)-hyperlipoproteinemia that may improve myocardial perfusion, angina symptoms and quality of life.
FundingNo financial support was received.
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors are grateful to Mascia Pianelli and Roberta Luciani for their excellent work in the apheresis unit.