We read with interest the paper by Brandão et al. entitled “Lipoprotein(a) as a key target in combined therapeutic approaches for cardiovascular disease”1 highlighting, in the era of new lipid-lowering drugs,2,3 the value of Lipoprotein(a) [Lp(a)] as a risk factor for atherosclerotic cardiovascular disease4 and the importance of its measurement in the cascade screening of familial hypercholesterolemia (FH).5,6 We were comforted by these results because we have been dosing Lp(a) at our Institute for this specific purpose for many years now. Indeed, already in the 1980s, the central role of Lp(a) in cardiovascular disease was demonstrated by various lines of research – epidemiology, biochemistry, pathophysiology7 and, unsurprisingly, measurement of Lp(a) has been strongly advocated in FH, as well as in other more frequent forms of dyslipidemia.8
Subsequent studies reinforced the importance of Lp(a), which should be assessed in all patients with premature coronary artery disease (CAD) in the absence of major coronary risk factors. Moreover, Lp(a) levels have been found to have a causal role in CAD and the relationship is so strong that, in some countries (such as Germany), Lp(a)-lowering therapy (i.e. lipoprotein apheresis) is reimbursed by the public health system.9
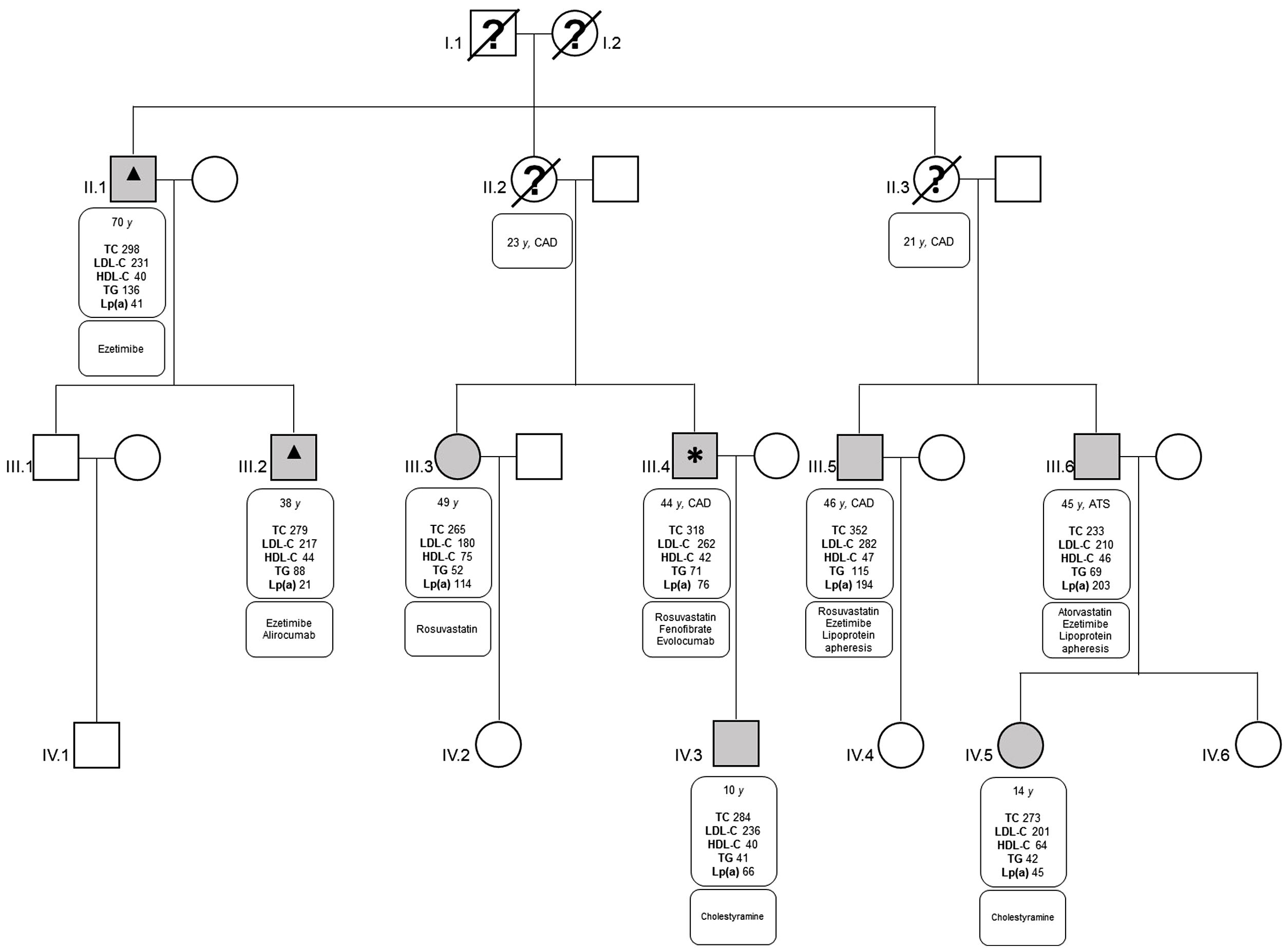
The paper by Ellis et al. has the merits of unifying the vision of Lp(a) across the Atlantic and draws attention to an argument which, still today, represents a missed opportunity in cardiovascular medicine, especially considering that we finally have the therapeutic means to intervene in patients with elevated Lp(a). In addition, the study provides the impetus to associate cascade screening with personalized therapy, as exemplified by the case of a family cared for at our Institute (Figure 1). In these cases, we were able to obtain an optimal balance between maximally tolerated lipid-lowering therapy, proprotein convertase subtilisin kexin type 9 inhibitors (PCSK9i) and lipoprotein apheresis. It should be borne in mind that PCSK9i therapy can be titrated to maintain adequate LDL-C levels while increasing the administration interval,10 although the effect on Lp(a) levels may be unpredictable.11
Pedigree of the proband family 1.
The proband (subject III.4) was referred to our Institute after percutaneous coronary intervention and was diagnosed with FH LDL-receptor gene (c.1860G>A) mutation. The other family members were identified by cascade screening and consequently treated. Two cousins with extremely high levels of Lp(a) associated with FH were started on lipoprotein apheresis (subject III.5 had undergone percutaneous coronary intervention, whereas subject III.6 had had a rapid progression of carotid atherosclerosis despite statin therapy). The proband (subject III.4) was treated temporarily with lipoprotein apheresis, which was subsequently replaced with PCSK9i therapy.
Legend: *: Proband; ▴: concomitant spinocerebellar ataxias with hyper-CPK; ATS: peripheral atherosclerosis on carotid vessels; CAD: coronary artery disease; HDL-C: high density lipoprotein cholesterol (mg/dl); LDL-C: low density lipoprotein cholesterol (mg/dl); Lp(a): lipoprotein(a) (mg/dl); TC: total cholesterol (mg/dl); TG: triglycerides (mg/dl); y: years.
No financial support was received.
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors are grateful to Mascia Pianelli and Roberta Luciani for the excellent work in the apheresis unit.