Patients with thoracic aortic aneurysm (TAA) are mostly asymptomatic and TAA is rarely related to heart failure (HF). We report the case of an 80-year-old female patient, with type A TAA without dissection, with right pulmonary artery and left atrium compression, who presented with HF, preserved ejection fraction and acute pulmonary edema.
Pacientes com aneurisma da aorta torácica (AAT) são geralmente assintomáticos e o AAT é raramente associado à insuficiência cardíaca (IC). Nós relatamos o caso de uma paciente feminina, 80 anos, com um AAT tipo A sem sinais de dissecção, que apresentou compressão do átrio esquerdo e da artéria pulmonar direita e desenvolvimento de IC com fração de ejeção preservada e edema agudo de pulmão.
Patients with thoracic aortic aneurysm (TAA) are mostly asymptomatic and TAA is rarely related to heart failure (HF). TAA may present acutely with rupture or dissection, or chronically, with symptoms related to surrounding structures.1 Extrinsic compression of the left atrium (LA) and the pulmonary vessels is an uncommon cause of hemodynamic compromise and may be secondary to the involvement of mediastinal structures, including TAA. This compression can lead to increased atrial and pulmonary artery pressures and may consequently cause pulmonary hypertension or pulmonary edema.2,3 We report the case of a patient with type A TAA with right pulmonary artery and LA compression, who had HF with preserved ejection fraction (HFpEF) and acute pulmonary edema (APE).
Case reportAn 80-year-old female patient, with a previous diagnosis of hypertension and HFpEF, was hospitalized with dry cough, progressive dyspnea on exertion, New York Heart Association (NYHA) functional class III/IV, orthopnea and lower limb edema. She also reported moderate atypical chest pain and dysphagia for solids.
On physical examination, blood pressure was 162/82 mmHg; heart rate was 88 bpm and respiratory rate was 27 ipm. Pathological jugular venous distention was present. The patient had a regular heart rhythm, with no murmurs; fine crackles in both lung bases and bilateral lower limb edema (++/4+).
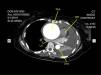
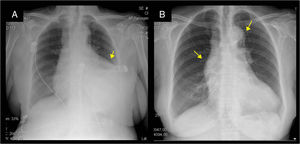
Complete right bundle branch block was observed on the electrocardiogram. Chest radiography showed cardiomegaly, mediastinal widening, and left pleural effusion that resolved with medical treatment. (Figure 1). Echocardiogram revealed left ventricular ejection fraction of 72%, increased LA, TAA diameter of 7.2 cm, moderate pericardial effusion with no signs of restriction, and left pleural effusion.
Twelve hours after admission she progressed with APE, which was controlled with medication. Seventy-two hours later she had atrial fibrillation without hemodynamic impairment. Clinical improvement occurred following drug treatment and she was discharged in NYHA class II.
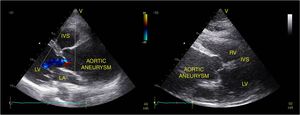
Echocardiogram one week later showed giant TAA with left atrial compression, diastolic dysfunction and preserved left ventricular ejection fraction, without pericardial or pleural effusion. (Figure 2)
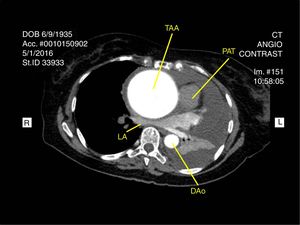
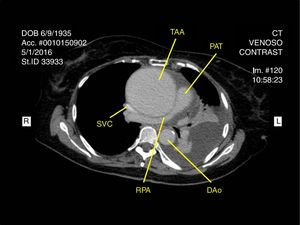
Chest angiography was performed and revealed a giant 8.3×7.7-cm TAA, which compressed the right pulmonary artery, the left and right atriums, the right ventricle and the esophagus, without any evidence of dissection (Figures 3 and 4).
Her clinical status significantly improved after administration of carvedilol, enalapril and furosemide. Correcting the TAA surgically was proposed; however, the patient and her family opted for conservative treatment.
DiscussionThe ascending aorta measures about 5cm in length and is connected to the right with the superior vena cava and right atrium; to the left with the pulmonary artery and posteriorly to the left atrium and the right pulmonary artery.
The compression of surrounding structures, particularly the LA, rarely causes hemodynamic effects.4 The few reports of HF caused by TAA are mainly associated with aneurysms with dissection.1,3–5 TAA complications are related to the compression of neighboring structures or a dissecting aneurysm. A large ascending aortic aneurysm can compress vessels, leading to hypertension and pulmonary edema, as in this patient.
HFpEF management has limitations related to comorbidities and the lack of strong evidence for specific treatment. It is reasonable to assume that AF triggered the HF decompensation.
In this case, it is important to note that there was no aneurysm dissection, clinical status stabilized and functional class improved with pharmacological treatment. Furthermore, it is worth highlighting that this is an unusual and unexpected cause of HF symptoms.
Aneurysm repair surgery was not performed due to a shared decision between the patient, her family and the physician, prioritizing the patient's quality of life.
Conflicts of interestThe authors have no conflicts of interest to declare.