Sarcoidosis increases inhomogeneity in ventricular repolarization due to the presence of sarcoid granuloma, which significantly correlates with ventricular fibrillation. Various studies have suggested that the interval from the peak to the end of the electrocardiographic T wave (T-peak to T-end [Tpe] interval) may correspond to the transmural dispersion of repolarization and that increased Tpe interval and Tpe/QT ratio are associated with malignant ventricular arrhythmias. The present study hypothesized that QT and Tpe intervals are significantly prolonged in sarcoidosis patients without apparent cardiac involvement.
MethodsThe study population consisted of 54 patients (37 female; mean age 43.4±10.6 years) under follow-up for sarcoidosis and 56 healthy subjects (37 female; mean age 42.4±8.6 years).
ResultsThere was no statistically significant difference between the groups in maximum QT interval, QT dispersion or corrected QT (QTc) interval, but QTc dispersion and Tpe interval were significantly prolonged in the sarcoidosis group compared to the control group (QTc dispersion 59.9±22.5 and 44.4±23.8, respectively, p=0.001; Tpe interval 79.4±9.3 and 70.7±7.03, respectively, p<0.001). We also found that the Tpe/QT ratio was significantly higher in sarcoidosis patients compared to the control group (0.21±0.02 and 0.18±0.23, respectively, p<0.001).
ConclusionOur study revealed that QTc dispersion, Tpe and Tpe/QT ratio were greater in sarcoidosis patients compared to the control group. To our knowledge, the present study is the first to use Tpe interval analysis in patients without cardiac involvement in sarcoidosis. Tpe interval and Tpe/QT ratio may be promising markers for cardiovascular morbidity and mortality due to ventricular arrhythmias in patients with and without cardiac involvement in sarcoidosis.
A sarcoidose aumenta a heterogeneidade na repolarização pelo granuloma sarcoide, aspeto que se correlaciona significativamente com a fibrilhação ventricular. Vários estudos sugeriram que o intervalo do pico ao fim da onda T no eletrocardiograma (Tpe) pode corresponder à dispersão transmural da repolarização e que um intervalo Tpe aumentado e o rácio Tpe/QT poderiam estar associados com o risco de arritmias ventriculares malignas. O presente trabalho coloca como hipótese que os intervalos QT e Tpe possam estar significativamente prolongados nos doentes com sarcoidose sem aparente envolvimento cardíaco.
MétodosA população do estudo foi constituída por 54 doentes (37 do sexo feminino, média de 43,4±10,6 anos) seguidos por sarcoidose e 56 indivíduos saudáveis (37 do sexo feminino; média de 42,4±8,6 anos).
ResultadosNão se encontraram diferenças significativas entre os dois grupos nos parâmetros intervalo QT máximo, dispersão QT e intervalo QTc. A dispersão do QTc e o intervalo TPE estavam significativamente mais prolongados no grupo de doentes com sarcoidose (dispersão do QTc 59,9±22,5 versus 44,4±23,8, p=0,001; Tpe 79,4±9,3 versus 70,7±7,03, p<0,001). Foi ainda possível demonstrar que o rácio Tpe/QT era significativamente mais alto nos doentes com sarcoidose em relação ao grupo de controlo (0,21±0,02; 0,18±0,23; p<0,001).
ConclusãoO nosso estudo revela que a dispersão do QTc, o intervalo Tpe e o rácio Tpe/QT são mais altos nos doentes com sarcoidose, quando comparados com um grupo de controlo. No nosso conhecimento, o presente estudo é o primeiro a usar a análise do intervalo Tpe em doentes sem envolvimento cardíaco na sarcoidose. O intervalo Tpe e o rácio Tpe/QT poderão vir a ser marcadores promissores para prever a morbilidade e a mortalidade cardiovascular por arritmias ventriculares em doentes com e sem envolvimento cardíaco da sarcoidose.
Sarcoidosis is a chronic multisystem disorder of unknown etiology1 that is most commonly seen in young and middle-aged adults. It is a worldwide disease, with a prevalence of about 4.7-64 per 100000.1 Non-caseating granulomas are the pathological hallmark and are most often associated with pulmonary involvement, but may also involve the heart, liver, peripheral lymph nodes, spleen, skin, eyes, phalangeal bones, parotid glands or other organs and tissues. Recent studies suggest that the disease may be an immunological response to an unidentified antigenic trigger.2 Given the multisystem nature of the disease, its systemic presentations are myriad. Even the cardiac manifestations of the disease vary widely from patient to patient. Symptomatic cardiac involvement is detected clinically in perhaps 5% of patients with pulmonary or systemic sarcoidosis, although cardiac granulomas are found in as many as 30% at autopsy.2 Imaging studies have found asymptomatic cardiac involvement in 3.7-54.9% of patients with extracardiac sarcoidosis.3 In particular, early-stage sarcoidosis has a silent progression in most patients despite the presence of cardiac involvement. Clinicians have come to recognize cardiac sarcoidosis (CS) as an uncommon but potentially fatal condition.4 The clinical manifestations of CS are dependent on the location, extent, and activity of the disease.5 The three principal sequelae of CS are conduction abnormalities, ventricular arrhythmias, and heart failure.3,5
A potential clinical application of interlead QT difference, termed QT dispersion (QTd), was proposed in 1990 by Day et al.6 Increased QTd on the surface electrocardiogram (ECG) has been linked to increased heterogeneity of ventricular repolarization, which is implicated in the genesis of ventricular arrhythmias, and has been associated with an adverse prognosis in a variety of patient populations.7–9 Myocardial repolarization has been assessed by various methods, including QT dispersion, corrected QT dispersion (cQTd), and transmural dispersion of repolarization. Studies have shown that T-peak to T-end interval (Tpe), the interval between the peak and the end of the T wave on the ECG, can be used as an index of total dispersion of repolarization (TDR).10 TDR reflects the heterogeneity rather than the total duration of repolarization.10 Recently, a new index, the Tpe/QT ratio, has been proposed as a more accurate measure of the dispersion of ventricular repolarization compared to QTd, cQTd and Tpe intervals, and is independent of alterations in heart rate.11
Changes in QTd in the course of sarcoidosis have been investigated before. Previous studies show that QTd, cQTd, maximum QT interval (QTmax), and maximum corrected QT interval (cQT) are affected in patients with CS.12 To our knowledge, the present study is the first to use Tpe interval analysis in patients without cardiac involvement in sarcoidosis. The present study hypothesized that QT and Tpe intervals are significantly prolonged in sarcoidosis patients without cardiac involvement.
MethodsPatient selectionA total of 54 patients (37 female; mean age 43.4±10.6 years) under follow-up for sarcoidosis and 56 healthy subjects (37 female; mean age 42.4±8.6 years) were included in the study. In the patient group, sarcoidosis was diagnosed by means of transbronchial ultrasound-guided lymph node biopsy. Chest X-ray was performed in all patients and staging was performed according to the Scadding classification,13 in which stage I was defined as bilateral hilar lymphadenopathy (BHL) with normal pulmonary parenchyma, stage II as parenchymal infiltration and BHL, stage III as bilateral parenchymal infiltration without BHL, and stage IV as pulmonary fibrosis or fibrocystic parenchymal involvement. The patients with sarcoidosis had no organ involvement other than the lungs. During the course of the study, none of the patients exhibited clinical signs or symptoms potentially associated with CS. None were being or had been treated with corticosteroids. Exclusion criteria were coronary artery disease, systemic hypertension, renal failure, chronic obstructive pulmonary disease, heart failure, diabetes, left ventricular systolic dysfunction previously determined by echocardiography (left ventricular ejection fraction [LVEF] <55%), moderate or severe heart valve disease, atrial fibrillation, thyroid and parathyroid conditions, stage III-IV sarcoidosis and connective tissue disorders. All patients underwent a physical examination, and medication histories were recorded. The study was approved by the ethics committee of our hospital, informed consent forms were signed by all participants, and the study was conducted in accordance with the 2008 Helsinki Declaration.
Echocardiographic assessmentTransthoracic echocardiography (TTE) was performed by one of the authors using a Philips iE33 ultrasound system with a 2.5-3.5 mHz transducer (Philips Medical Systems, Andover, MA, USA) with all subjects in left lateral decubitus position. M-mode measurements were obtained in parasternal view and two-dimensional (2D) and Doppler measurements in parasternal and apical views. M-mode and 2D assessments were performed according to the American Society of Echocardiography criteria.14 Left ventricular wall motion was assessed in standard apical 2- and 4-chamber views. Simpson's method was used to measure LVEF. The echocardiographic evaluation was performed by the same individual for each subject.
ElectrocardiographyAll standard 12-lead ECGs were obtained at rest in supine position simultaneously using a recorder (Nihon Kohden Corporation, Tokyo, Japan) set at 50 mm/s paper speed and 1 mV/cm standardization. The ECGs were numbered and presented to the analyzing investigators without name or date information. They were each assessed by two cardiologists and to reduce measurement error, QT and Tpe intervals were assessed with calipers and magnifying glass.
The QT interval in each precordial lead was measured from the first deflection of QRS onset to the end of the T wave as it merged with the isoelectric TP baseline. In the presence of a U wave, the end of the QT interval was taken as the nadir between the T-wave peak and the U-wave peak. Correction of the QT interval for heart rate (QTc) was performed using Bazett's formula.15 QT and QTc interval dispersion was calculated as the difference between maximum and minimum precordial values.
T-wave variables, including T-wave duration and amplitude and Tpe interval, were manually measured. T-wave variables were only assessed in lead V5. T-wave duration was determined by the intersection of the base line with the line that followed the steepest part of the T wave, before and after its peak. Tpe was defined as the difference between the QT interval and the QT-peak interval. The peak of the T wave was defined as the highest amplitude of the T-wave deflection. T-wave amplitude was measured from the base line to the peak of the T wave. Two consecutive QT intervals and T waves were measured for each ECG recording, and the arithmetic mean was calculated.
Statistical analysisSPSS version 20 (IBM SPSS, Chicago, IL, USA) was used to assess the data. Quantitative data were presented as means ± standard deviation, median value, and qualitative data were presented as percentages. The Mann-Whitney U test was used for the paired comparison of qualitative data, and the Student's t test was used for comparison of quantitative data. The results were analyzed with a 95% confidence interval at a significance level of p<0.05 or with a 99% confidence interval at a high significance level of p<0.01.
ResultsAmong the 110 participants included in the study, 54 had stage I or II sarcoidosis (49 stage I, five stage II) and 56 were healthy. There were no statistically significant differences between the two groups regarding age, gender, systolic or diastolic blood pressure, heart rate, body mass index or smoking (Table 1). None of the patients with sarcoidosis was receiving oral or inhaled steroids. There was no clinical finding suggestive of cardiac involvement in any of the patients.
Clinical characteristics of patients with sarcoidosis and healthy subjects included in the study.
| Sarcoidosis patients (n=54) | Controls (n=56) | p | |
|---|---|---|---|
| Age, years | 43.4±10.6 | 42.4±8.6 | 0.60 |
| Gender, M/F | 17/37 | 19/37 | 0.78 |
| Smoking, n (%) | 12 (22.2) | 11 (19.6) | 0.74 |
| Family history, n (%) | 12 (22.2) | 13 (23.2) | 0.90 |
| Dyslipidemia, n (%) | 6 (11.1) | 6 (10.7) | 0.94 |
| BMI, kg/m2 | 27.9±4.3 | 27.6±4.5 | 0.67 |
| HR, bpm | 80.2±11.6 | 77.8±8.9 | 0.23 |
| SBP, mmHg | 119±8.9 | 116.9±8.7 | 0.21 |
| DBP, mmHg | 75.5±8.8 | 70.1±8.6 | 0.002 |
| Disease stage I or II, n | 49/5 | - |
BMI: body mass index; bpm: beats per minute; DBP: diastolic blood pressure; F: female; HR: heart rate; M: male; SBP: systolic blood pressure.
Echocardiographic assessment revealed no significant differences between the two groups regarding left ventricular end-systolic and end-diastolic diameters, LVEF, or annular velocity determined by tissue Doppler (Table 2). LVEF calculated by the modified Simpson's method was 61.8±7.8% in the sarcoidosis group vs. 64.1±2.7% in the control group (p=0.04). Left ventricular interventricular septum thickness, posterior wall thickness and relative wall thickness were significantly greater in the sarcoidosis group than in the control group (p<0.001).
Two-dimensional and conventional Doppler echocardiographic parameters in the sarcoidosis and control groups.
| Sarcoidosis patients (n=54) | Controls (n=56) | p | |
|---|---|---|---|
| LVDD, mm | 4.3±0.3 | 4.1±0.2 | 0.003 |
| LVSD, mm | 2.8±0.3 | 2.7±0.2 | 0.24 |
| IVSD, mm | 1.04±0.08 | 0.94±0.12 | <0.001 |
| PWD, mm | 1.04±0.08 | 0.93±0.12 | <0.001 |
| RWT | 0.43±0.06 | 0.49±0.04 | <0.001 |
| LVEF (2D), % | 63.6±4.7 | 63.1±2.4 | 0.55 |
| LVEF (Simpson), % | 61.8±7.8 | 64.1±2.7 | 0.04 |
| Mitral inflow E velocity | 0.92±0.17 | 1±0.09 | 0.11 |
| Mitral inflow A velocity | 0.67±0.18 | 0.57±0.13 | 0.006 |
| DT, ms | 179.7±68.7 | 174.5±15.8 | 0.59 |
| Septal E | 0.09±0.03 | 0.11±0.10 | 0.04 |
| Septal A | 0.09±0.02 | 0.09±0.01 | 0.21 |
| Septal S | 0.10±0.09 | 0.09±0.01 | 0.60 |
2D: two dimensional echocardiography; DT: deceleration time; IVSD: interventricular septum diameter; LVDD: left ventricular diastolic diameter; LVEF: left ventricular ejection fraction; LVSD: left ventricular systolic diameter; PWD: posterior wall diameter; RWT: relative wall thickness.
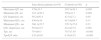
The electrocardiographic parameters of the groups are presented in Table 3. Although QTmax, QT dispersion and QTc intervals were not different between groups, QTc dispersion and Tpe interval were significantly greater in the sarcoidosis group compared to the control group (59.9±22.5 vs. 44.4±23.8, p=0.001, and 79.4±9.3 vs. 70.7±7.03, p<0.001, respectively). We also found that the Tpe/QT ratio was significantly higher in sarcoidosis patients compared to controls (0.21±0.02 vs. 0.18±0.23, p<0.001).
Electrocardiographic parameters of the sarcoidosis and control groups.
| Sarcoidosis patients (n=54) | Controls (n=56) | p | |
|---|---|---|---|
| Maximum QT, ms | 379±33.7 | 392.5±39.1 | 0.056 |
| Minimum QT, ms | 322.1±50.1 | 350±41.7 | 0.002 |
| QT dispersion, ms | 59.2±56.4 | 42.5±27.2 | 0.05 |
| Maximum QTc, ms | 430.6±34 | 415.9±64.7 | 0.13 |
| Minimum QTc, ms | 366.1±52.7 | 376.7±37.6 | 0.23 |
| QTc dispersion, ms | 59.9±22.5 | 44.4±23.8 | 0.001 |
| Tpe, ms | 79.4±9.3 | 70.7±7.03 | <0.001 |
| Tpe/QT ratio | 0.21±0.02 | 0.18±0.23 | <0.001 |
QTc: corrected QT interval; Tpe: T-peak to T-end interval.
CS is a rare clinical entity, affecting perhaps 5% of patients with systemic sarcoidosis; however, it is associated with a spectrum of clinically significant conduction abnormalities and arrhythmias.1 Cardiac involvement remains a morbid and potentially lethal manifestation of sarcoidosis. Clinicians should maintain a high degree of suspicion for cardiac involvement in patients with extracardiac sarcoidosis and likewise should consider CS in patients with unexplained ventricular tachyarrhythmia, high-degree heart block, or cardiomyopathy. The first manifestation of CS may be high-degree atrioventricular block, sustained atrial arrhythmias, or malignant ventricular arrhythmia (including sudden death). The substrate for arrhythmias may be active granuloma formation in the myocardium or myocardial fibrosis.
Dispersion of repolarization of the ventricular myocardium is thought to be an important factor in the pathogenesis of arrhythmias.16 Electrical instability of the heart muscle can be detected by QTd on the surface ECG17 but simple QTd provides only an imperfect estimate of the degree of heterogeneity of repolarization. Several studies have suggested that QTd helps identify patients at increased risk of ventricular arrhythmias or clinical events in a variety of clinical settings.10 However, the value of QTd in risk stratification is the subject of debate.
In the Rotterdam Study, de Bruyne et al.8 studied cQTd using the Modular ECG Analysis System. During follow-up, risk for cardiac death, sudden cardiac death, and total mortality were higher in the highest cQTd tertile. In a study of patients with familial Mediterranean fever (FMF), Nussinovitch et al.18 reported that amyloidosis of FMF is associated with increased QT variability index compared with controls, but it remains unknown whether this finding is solely amyloidosis-related or whether it has any prognostic significance. Kunisek et al.,19 studying 187 patients with left ventricular hypertrophy (LVH), found no significant association of QTc interval with the degree and type of LVH. Analysis by gender showed that men with severe concentric and eccentric LVH had higher QTc interval and QTd values than those with asymmetric LVH (not significant). In another study,12 QTd, cQTd, QTmax, and maximum cQT were prolonged in patients with CS compared to patients with noncardiac sarcoidosis and control subjects. This study highlights the importance of the ECG, a useful, simple, noninvasive, broadly accessible, easily repeatable and applied, and affordable tool in the differentiation of patients with and without cardiac involvement in sarcoidosis. Unlike this study, we investigated Tpe interval, Tpe/QT and Tpe/QTc ratio in sarcoidosis patients compared to control subjects.
Tpe interval is a measure of transmural dispersion of left ventricular repolarization and is accepted as a surrogate for increased risk of ventricular arrhythmogenesis. The underlying mechanism of Tpe prolongation and ventricular repolarization abnormalities was proposed by Antzelevitch et al.20 and other authors to be related to the different types of cells in ventricular myocardium. Previous studies showed that Tpe interval prolongation is associated with increased mortality in Brugada syndrome, long QT syndrome, hypertrophic cardiomyopathy, and myocardial infarction.21 Recently, Tpe interval and Tpe/QT ratio have emerged as novel electrocardiographic markers of increased dispersion of ventricular repolarization.10 Tpe/QT ratio has been shown to be a more sensitive index of ventricular repolarization and arrhythmogenesis than Tpe interval and, unlike the latter, was found to remain constant despite dynamic changes in heart rate.
Yan et al.22 proposed that changes in Tpe interval may predict the risk of ventricular arrhythmia, while Demir et al. showed that Tpe interval and Tpe/QT ratio were prolonged in nondipper patients.23 Zehir et al.24 found that slow coronary flow (SCF) is associated with increased Tpe interval and Tpe/QT ratio and that measurement of these two parameters ratio can be used to indicate increased risk of SCF-related adverse cardiovascular events.
Our results demonstrated that QTc dispersion, Tpe interval, and Tpe/QT and Tpe/QTc ratios were increased in sarcoidosis patients compared to the control group. To our knowledge, the present study is the first to use analysis of Tpe intervals and the Tpe/QT ratio in patients with sarcoidosis.
In conclusion, cardiac involvement is an independent predictor of mortality in sarcoidosis, and is associated with poor prognosis.25 It is therefore important to detect cardiac involvement during the subclinical stage, before the occurrence of symptoms. Variability in clinical presentation, disease severity, organ involvement, and response to steroids make it difficult to determine the natural history and prognosis of sarcoidosis. The risk of arrhythmia in this disease should be borne in mind, and consideration should be given to prophylactic implantation of a cardioverter-defibrillator, particularly in the presence of ventricular arrhythmias or reduced LVEF.
The measurement of Tpe interval and Tpe/QT ratio may be used to indicate increased risk of sarcoidosis-related adverse cardiovascular events. According to the current study's findings, the risk of development of ventricular arrhythmia may be increased in sarcoidosis patients due to myocardial voltage gradients resulting from heterogeneity of repolarization.
Further studies are required to determine the relation between Tpe interval and Tpe/QT ratio and ventricular arrhythmia in patients with sarcoidosis.
ConclusionOur study revealed that QTc dispersion, Tpe interval, and Tpe/QT and Tpe/QTc ratios were greater in sarcoidosis patients compared to the control group. Tpe interval and Tpe/QT ratio may be promising markers for cardiovascular morbidity and mortality due to ventricular arrhythmias in patients with and without cardiac involvement in sarcoidosis.
Conflicts of interestThe authors report no conflicts of interest, sources of financial support or corporate involvement, and confirm that the contents have not been partially or wholly published elsewhere.