Successful treatment of myocardial infarction (MI) is one of the major achievements in cardiovascular disease management in recent decades. Internationally this favorable outcome was mainly obtained through national primary percutaneous coronary intervention (P-PCI) programs available 24/7.
In Portugal, this organizational challenge was addressed in 2007 with specific regulatory documents1 aimed at pre-hospital emergency system management for MI and stroke and procedures for referral to emergency departments and catheterization laboratories (the coronary and stroke fast-track systems). In 2010, P-PCI was officially defined as the priority strategy.2 A national network of P-PCI facilities was set up in 20153 with hubs covering more than 95% of the overall resident population.
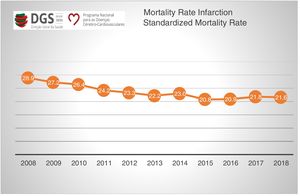
The latest available national data4 showed an impressive 25% reduction in standardized overall MI-related mortality over a one-decade period (Figure 1). This reduction was more marked in female patients aged over 70 years, who are conventionally considered to be an under-treated group.
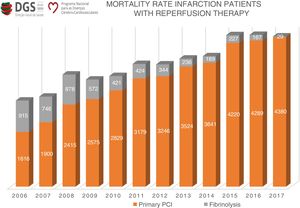
In this period, a significant increase was noted in the numbers of nationwide P-PCI procedures, along with a corresponding decrease in patients treated by fibrinolysis (Figure 2). However, this growth has become less steep in the last few years, which warrants further analysis.
Yearly changes in the number of patients with myocardial infarction undergoing reperfusion therapy in Portugal. Source: annual report of the National Program for Cerebrovascular and Cardiovascular Disease (PNDCCV) 2017, Directorate-General of Health (DGS). PCI: percutaneous coronary intervention.
These results were obtained through the convergence of official regulatory initiatives regarding the pre-hospital emergency services (INEM) and hospital institutions with programs promoted by medical societies, such as the Stent for Life initiative of the European Society of Cardiology, endorsed by the Portuguese Society of Cardiology.
The work published by Pereira et al. in this issue of the Journal5 summarizes the differences between parameters in ST-segment myocardial infarction patients in 2011 and 2016 and reveals a significant improvement in MI treatment pathways, as shown by a consistent reduction in patient-related time delays. As the authors point out, a similar improvement was not recorded in system delays, emphasizing the need to maintain and strengthen these initiatives.
Another important finding concerns improvements in access to appropriate therapy, with a significant reduction in admissions to non-PCI capable centers along with increased activation of the pre-hospital emergency system by use of the 112 emergency telephone number. These improvements have had major repercussions in system performance, considering the chronic difficulties related to secondary patient transportation between different hospital institutions.
The importance of public health gains obtained with adequate treatment of MI (one of the leading causes of death in Portugal as well as in other European countries) highlights the need for more complete data collection at a national level, for example enabling monitoring of system and institutional performance.
The quantitative aspects of this question must be complemented with qualitative information regarding, for example, geographical inequalities and location-specific limitations to access.
The complete lack of information regarding non-revascularized patients and the real reasons for their status should also be addressed.
In recent years, several initiatives have been promoted designed to lead to the establishment of a national MI registry, in various circumstances and with different official interlocutors. We consider such a registry to be an essential tool to support strategic decisions based on real-word data that are sometimes very different from those expected.
This registry would overcome one of the most important current limitations: matching clinical data from the pre-hospital emergency system with hospital information and subsequent prognostic assessments.
Although this goal has yet to be attained, we note some recent hopeful developments, including an increasing awareness of the importance of this information.
Conflicts of interestThe author has no conflicts of interest to declare.