ST-elevation myocardial infarction (STEMI) is a medical emergency that benefits from rapid access to specialized care. The objective of this study was to describe developments in patient transport via the pre-hospital emergency medical system (EMS) and its impact on clinical outcomes.
MethodsWe retrospectively studied STEMI patients who underwent primary percutaneous coronary intervention between January 2008 and July 2015. Patients were divided according to type of admission. Total ischemic time (TIT), door-to-balloon time (DBT) and in-hospital and one-year clinical outcomes were assessed for each group.
ResultsA total of 764 patients were included, of whom 33.5% were transported by the EMS and 45.8% by their own means, 13.7% were transferred from another institution and 6.9% were transported by non-EMS ambulance. There was a trend for more frequent recourse to the EMS over the eight-year period. There was a higher percentage of patients with prior myocardial infarction and Killip class III/IV in the EMS group compared to the non-EMS group. Significant differences were seen between groups in reperfusion times, EMS patients having the shortest TIT and DBT (195 vs. 286 min, p<0.001 and 61 vs. 90 min, p<0.001, respectively), but no significant difference in event rates was observed. Patients presenting to the hospital early had higher rates of effective reperfusion and lower in-hospital mortality (6.9% vs. 33.9%, p<0.001).
ConclusionsRecourse to the EMS significantly reduced ischemic times. Although this improvement was not directly associated with significant differences in event rates, it was associated with higher rates of effective reperfusion that were reflected in lower in-hospital mortality.
O enfarte agudo do miocárdio com elevação de ST (EAMcST) constitui uma emergência médica, beneficiando de um acesso rápido a cuidados diferenciados. O objetivo deste estudo foi avaliar a evolução do transporte através da emergência pré-hospitalar (EPH) e o seu impacto nos eventos clínicos.
MétodosEstudo retrospetivo de doentes com EAMcST, submetidos a intervenção coronária percutânea primária entre janeiro de 2008 e julho de 2015. Os doentes foram divididos de acordo com o modo de transporte/admissão. Para cada grupo foi analisado tempo isquémico total (TIT), tempo porta-balão (TPB) e eventos intra-hospitalares e a um ano.
ResultadosDe um total de 764 doentes, 33,5% foram transportados pela EPH, 45,8% chegaram por meios próprios, 13,7% transferidos de outra instituição e 6,9% pelos bombeiros. Nos últimos oito anos, verificou-se uma tendência para uma utilização crescente da EPH. O grupo EPH, comparado com os restantes (não-EPH), englobou uma percentagem maior de doentes com enfarte prévio, em classe III/IVKillip e apresentou uma redução significativa do TIT e TPB (195 versus 286 minutos p<0,001 e 61 versus 90 minutos p<0,001), mas não se verificaram diferenças significativas na taxa de eventos hospitalares ou a um ano. Os doentes que se apresentaram mais precocemente obtiveram taxas mais elevadas de reperfusão eficaz e menor mortalidade intra-hospitalar (6,9 versus 33,9% p<0,001).
ConclusãoVerificou-se um impacto significativo da ativação da EPH na redução dos tempos de isquemia. Apesar de essa melhoria não se ter associado de forma direta a diferenças significativas na taxa de eventos, associou-se a taxas mais elevadas de reperfusão eficaz, que se refletiram numa redução da mortalidade intra-hospitalar.
ST-elevation myocardial infarction (STEMI) is a medical emergency that has high morbidity and mortality if not promptly and appropriately treated. Since mortality is higher in the first few hours, and early reperfusion, ideally by primary percutaneous coronary intervention (PPCI), is associated with better prognosis, it is essential to transport patients as quickly and safely as possible to the catheterization laboratory.1,2
Based on the notion that “time is myocardium”, current guidelines recommend a target door-to-balloon time (DBT) of ≤90 min (ideally ≤60 min, especially in high-risk patients with anterior myocardial infarction [MI] who present early – within two hours of symptom onset – or who are seen in an institution with 24-hour PPCI capability), which is a measure of the quality of hospital care for STEMI patients.2,3 Various measures have been proposed and different programs implemented in order to improve the quality of care and to reduce delays in access to PPCI. A pre-hospital emergency medical system (EMS) is a crucial link in the chain of survival for STEMI patients, since it enables rapid diagnosis and referral for PPCI, with the patient being transported directly to a center capable of performing mechanical reperfusion, accompanied by a team trained in advanced life support.4–6 Pre-hospital diagnosis, triage and initial treatment by an EMS team have been shown to be associated with greater use of reperfusion therapy and reduced delays, leading to better clinical outcomes in STEMI.7,8 Nevertheless, studies report that the EMS continues to be underused and that many patients arrive at the hospital by their own means.4,9,10 The Portuguese Registry of Interventional Cardiology shows that despite greatly improved access in recent years to PPCI, only 38% of MI patients use the EMS.5
The objective of this study was to describe developments in pre-hospital transport of a series of STEMI patients undergoing PPCI over an eight-year period to 2015 and to characterize this population and assess the impact of recourse to the EMS on in-hospital and one-year clinical outcomes.
MethodsStudy population and definitionsThis was a retrospective single-center study of consecutive patients admitted for STEMI and who underwent PPCI between January 2008 and July 2015. The type of admission was ascertained for each patient, and the study population was initially divided into four groups as follows: admission via the pre-hospital EMS (which includes trained medical teams able to perform electrocardiography [ECG] and thus establish a diagnosis of STEMI, institute initial treatment and perform advanced life support); by their own means (by private car, taxi or public transport); by non-EMS ambulance; and transferred from another facility (public or private, without PPCI capability). Patients who were already hospitalized for another reason at the time of symptom onset were excluded. For the purposes of comparative analysis, the population was subsequently divided into two groups: EMS and non-EMS. Clinical, laboratory and procedure-related variables from admission to discharge were compiled from the hospital's database.
The diagnosis of STEMI was based on clinical criteria, supported by the following ECG alterations: ST elevation of ≥0.15 mV in V2-V3 or ≥0.1 mV in at least two contiguous leads; ST depression of ≥0.15 mm in V2-V3 with positive T wave; or de novo complete left bundle branch block. Total ischemic time (TIT) was defined as the time between onset of intense and persistent symptoms and passage of the guidewire. Door-to-balloon time (DBT) was defined as the time between the first recorded contact at the hospital and passage of the guidewire. The no-reflow phenomenon was defined as failure to achieve distal coronary TIMI ≥2 flow after angioplasty or TIMI 2-3 flow but with no myocardial blush (myocardial perfusion grade 0), or if after perfusion, contrast staining was observed (myocardial perfusion grade 1), in the absence of spasm, dissection or epicardial coronary thrombus, which persisted after intracoronary administration of nitroglycerin and adenosine. Effective reperfusion was considered to be achieved in the absence of the no-reflow phenomenon. Creatinine clearance was calculated by the Cockcroft-Gault formula. Risk stratification was performed by determining GRACE (for in-hospital and six-month mortality) and TIMI (for STEMI) scores for all patients, as well as classification of coronary artery disease complexity by the SYNTAX score II. Left ventricular ejection fraction (LVEF) was calculated during hospital stay by two-dimensional echocardiography using Simpson's biplane method. For the purposes of statistical analysis, LVEF was classified into two groups: preserved or mildly impaired left ventricular systolic function (LVEF >45%); and moderate/severe left ventricular dysfunction (LVEF ≤45%). Cumulative major adverse cardiac events (in-hospital and at one-year follow-up) were defined as cumulative overall mortality (cardiac and non-cardiac), new myocardial infarction (with or without ST-segment elevation), target vessel revascularization, or stroke. Clinical events were assessed through consultation of medical records or through direct contact with the patient, relatives or the attending physician.
Procedures and medicationA 6F or 7F introducer was used during PPCI. Unfractionated heparin (70 UI/kg) was administered during the procedure. Use of aspiration thrombectomy and glycoprotein IIb/IIIa inhibitors, and choice of stent and other adjuvant devices were left to the operator's discretion. All patients were medicated with aspirin 300 mg and clopidogrel 600 mg or ticagrelor 180 mg prior to PCI.
After the procedure, all patients were admitted to the coronary care unit, where they remained for at least 48 h. Myocardial necrosis markers (troponin T and creatine kinase) were measured six, 12, 24 and 48 h after reperfusion. At discharge all patients were prescribed dual antiplatelet therapy (aspirin 100 mg/day and clopidogrel 75 mg/day or ticagrelor 90 mg twice daily), as well as any other medication deemed necessary by the attending physician in accordance with current guidelines.
Statistical analysisContinuous variables were expressed as means±standard deviation or medians and interquartile range (IQR) for variables with normal or non-normal distribution, respectively. Continuous variables with normal distribution were compared using the Student's t test for independent samples, while those with non-normal distribution were compared using the Mann-Whitney test. Categorical variables were expressed as frequencies and percentages and compared using the chi-square test or Fisher's exact test. Unadjusted mortality associated with type of admission was calculated using the Kaplan-Meier method, differences being analyzed by the log-rank test. Predictors of mortality were determined using a Cox model, with mortality as the dependent variable and including all variables with p<0.1 on univariate analysis.
All results were considered significant with p<0.05. The statistical analysis was performed using SPSS version 20 (IBM SPSS, Chicago, IL, USA).
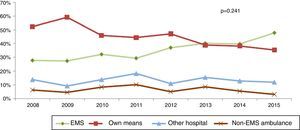
ResultsDuring the study period, 788 consecutive patients were admitted to our center for STEMI and underwent PPCI, of whom 24 were excluded due to incomplete data. Of the 764 analyzed, 256 (33.5%) were transported by the EMS and the remaining 508 by non-EMS means: 350 (45.8%) arrived at the emergency department by their own means, 105 (13.7%) were transferred from another hospital and 53 (6.9%) were transported by non-EMS ambulance. Figure 1 shows developments in type of hospital admission over the last eight years. There was a general trend for greater use of the EMS rather than patient's own means, although without statistical significance (p=0.241).
Table 1 summarizes the clinical, demographic and procedure-related characteristics of the EMS and non-EMS groups. There were no significant differences in cardiovascular risk factors, current therapy or procedure-related variables. Patients with previous infarction were more likely to use the EMS than those who presented with preinfarction angina. Although there were no significant differences in clinical risk scores (GRACE or TIMI) at admission, the EMS group more often presented in Killip class III/IV heart failure.
Clinical, demographic and procedure-related characteristics of the study population.
| EMS | Non-EMS | p | |
|---|---|---|---|
| Clinical and demographic characteristics | |||
| Age±SD (years) | 62.71±13.03 | 62.60±13.48 | 0.911 |
| Male, n (%) | 190 (74.2) | 369 (72.6) | 0.354 |
| Diabetes, n (%) | 67 (26.4) | 131 (25.8) | 0.489 |
| Dyslipidemia (%) | 142 (55.9) | 284 (56.0) | 0.519 |
| Hypertension, n (%) | 143 (56.5) | 221 (57.4) | 0.439 |
| Smoking, n (%) | 140 (55.1) | 257 (50.7) | 0.141 |
| Body mass index±SD (kg/m2) | 26.42±3.63 | 26.48±3.76 | 0.829 |
| Previous infarction, n (%) | 28 (11.0) | 34 (6.7) | 0.030 |
| Preinfarction angina, n (%) | 74 (29.0) | 179 (35.4) | 0.045 |
| Admission Hb±SD (mg/dl) | 13.87±1.71 | 14.16±1.82 | 0.040 |
| Admission CrCl±SD (ml/min) | 87.66±38.17 | 86.57±36.49 | 0.702 |
| Previous medication | |||
| Beta-blocker, n (%) | 33 (13.3) | 61 (12.1) | 0.370 |
| ACE inhibitor, n (%) | 48 (19.3) | 84 (16.7) | 0.219 |
| ARB, n (%) | 40 (16.1) | 90 (17.9) | 0.303 |
| CCB | 22 (8.8) | 48 (9.5) | 0.433 |
| Nitrates, n (%) | 9 (3.6) | 22 (4.4) | 0.388 |
| Statin, n (%) | 62 (24.8) | 115 (22.9) | 0.307 |
| Aspirin, n (%) | 40 (16.1) | 70 (13.0) | 0.248 |
| Clopidogrel, n (%) | 18 (7.2) | 13 (2.6) | 0.003 |
| Oral antidiabetics, n (%) | 46 (18.5) | 89 (17.7) | 0.438 |
| Insulin, n (%) | 15 (6.0) | 21 (4.2) | 0.175 |
| Risk scores | |||
| TIMI (IQR) | 3.76 (3) | 4.13 (3) | 0.311 |
| GRACE (IQR) | 212.96 (63) | 208.69 (58) | 0.410 |
| Killip class III/IV, n (%) | 44 (17.3) | 60 (11.9) | 0.028 |
| Procedure-related variables | |||
| Mean SBP (mmHg) | 118±25 | 121±27 | 0.104 |
| Radial access | 150 (58.8) | 304 (60.1) | 0.345 |
| Number of vessels | 1.88±0.85 | 1.89±0.84 | 0.837 |
| Target vessel | |||
| LAD, n (%) | 105 (41.0) | 222 (43.8) | |
| Cx, n (%) | 26 (10.2) | 81 (15.8) | |
| RC, n (%) | 122 (47.7) | 200 (39.5) | |
| LM, n (%) | 3 (1.2) | 5 (1.0) | |
| Aspiration thrombectomy | 167 (65.2) | 331 (65.3) | 0.525 |
| Drug-eluting stent, n (%) | 156 (60.9) | 295 (58.1) | 0.432 |
| Gp IIb/IIIa inhibitors | 68 (26.8) | 133 (26.4) | 0.488 |
| IABP | 7 (2.7) | 13 (2.6) | 0.528 |
| SYNTAX score (IQR) | 18.95 (12) | 18.70 (12.5) | 0.792 |
| PCI of non-culprit vessels | 34 (13.4) | 106 (21.1) | 0.006 |
ACE: angiotensin-converting enzyme; ARB: angiotensin receptor blocker; CCB: calcium channel blocker; CrCl: creatinine clearance; Cx: circumflex artery; EMS: Emergency medical system; Gp: glycoprotein; Hb: hemoglobin; IABP: intra-aortic balloon pump; IQR: interquartile range; LAD: left anterior descending artery; LM: left main artery; PCI: percutaneous coronary intervention; RC: right coronary artery; SBP: systolic blood pressure; SD: standard deviation.
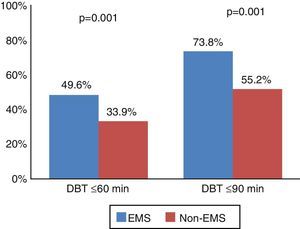
The study population presented a median TIT of 240 min (83.8% had TIT of >120 min) and median DBT was 85 min. The EMS group had significantly shorter TIT and DBT, by 91 and 29 min, respectively, compared to the non-EMS group (median TIT 195 [IQR 150] vs. 286 [IQR 360] min, p<0.001; and median DBT 61 [IQR 55] vs. 90 [IQR 90] min, p<0.001) (Table 2). A significantly larger proportion of patients in the EMS group achieved the target DBTs of ≤90 min (73.8% vs. 55.2%, p<0.001) and ≤60 min (49.6% vs. 33.9%, p<0.001) (Figure 2).
With regard to in-hospital results (Table 3), there were no significant differences in peak enzyme levels, length of hospital stay or major adverse cardiac events. A lower percentage of patients in the EMS group presented moderate to severe left ventricular systolic dysfunction, albeit without statistical significance.
In-hospital results.
| EMS | Non-EMS | p | |
|---|---|---|---|
| Peak enzyme levels | |||
| hs-cTnT (ng/l)±SD | 6.95±8.22 | 6.80±8.22 | 0.821 |
| Creatine kinase (U/l)±SD | 2580.94±2669.03 | 2435.12±2052.61 | 0.412 |
| Length of hospital stay (days)±SD | 8.28±7.10 (median 6) | 7.44±5.71 (median 6) | 0.104 |
| Advanced AV block, n (%) | 10 (3.9) | 28 (5.5) | 0.216 |
| Mortality, n (%) | 24 (9.4) | 46 (9.1) | 0.490 |
| Reinfarction, n (%) | 3 (1.2) | 9 (1.8) | 0.387 |
| Stroke, n (%) | 4 (1.6) | 7 (1.4) | 0.533 |
| LV systolic function (n=727) | 0.075 | ||
| Preserved/mildly impaired, n (%) | 163 (66.5) | 292 (59.9) | |
| Moderate/severe dysfunction, n (%) | 82 (33.5) | 195 (40.0) | |
AV: atrioventricular; EMS: pre-hospital emergency medical system; hs-cTnT: high-sensitivity cardiac troponin T; LV: left ventricular.
The no-reflow phenomenon was observed in 8.2% of patients after PCI, effective reperfusion being achieved in 91.8%. Patients who presented at the hospital earlier (DBT ≤60 min) showed significantly higher reperfusion rates (94.8% with DBT ≤60 min vs. 90.2% with DBT >60 min, p=0.020). Among the patient subgroup with DBT ≤60 min, those that used the EMS derived greater benefit, with effective reperfusion rates of 97.6% vs. 92.4% in the non-EMS group (p=0.042). Effective reperfusion was associated with significantly lower in-hospital mortality, 6.9% vs. 33.9% in those not effectively reperfused (p<0.001). After multivariate analysis (adjusted for Killip class at admission, age, diabetes, dyslipidemia, smoking, preinfarction angina and creatinine clearance), effective reperfusion was an independent predictor of in-hospital mortality (hazard ratio [HR]: 3.78 [95% confidence interval (CI) 1.69-8.47], p=0.001), as was presentation in Killip class III/IV and low creatinine clearance (HR: 10.72 [95% CI 5.46-21.06], p<0.001 and HR: 0.98 [95% CI 0.96-0.99], p=0.008), respectively.
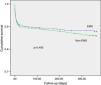
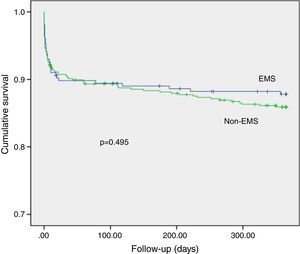
Analysis of one-year follow-up (Table 4) showed that mortality was higher in the non-EMS group, but without statistical significance. There were also no significant differences in other adverse cardiac events. Figure 3 shows the one-year cumulative survival curve. In univariate analysis, age, diabetes, hypertension, current smoking, previous infarction or preinfarction angina, TIT, DBT, Killip class III/IV at admission and moderate/severe left ventricular dysfunction at discharge correlated with cumulative mortality. These variables and type of admission (EMS vs. non-EMS) were included in the multivariate analysis, which showed that only Killip class III/IV at admission (HR: 6.315 [95% CI: 3.314-12.042], p<0.001), moderate/severe left ventricular dysfunction (HR: 2.486 [95% CI: 1.352-4.57], p=0.003) and age (HR: 1.050 [95% CI: 1.020-1.082], p=0.001) remained as independent predictors, use of the EMS having no independent effect on this outcome. Similarly, there were no statistically significant differences in one-year mortality between patients with and without effective reperfusion (9.8% vs. 4.2%, p=0.105).
Following the implementation of various measures and programs in Portugal in recent years, our study shows a progressive increase in use of the EMS as opposed to patients’ own means, which has resulted in significant reductions in both DBT and TIT. Compared to the non-EMS group, patients using the pre-hospital EMS had significantly shorter reperfusion times, the target DBT of ≤90 min being achieved in 73.8%, and in 49.6% of these, DBT was ≤60 min. These results are in agreement with various studies that have shown the positive impact on reducing ischemic times of measures such as use of the EMS, pre-hospital ECG, and direct transport of STEMI patients to centers with catheterization laboratories.4,9–13 Nevertheless, only a third of patients in our study used the EMS, a disappointingly low proportion. As in a study by Fujii et al.,13 patients with previous MI were more likely to use the EMS, as were those in shock or with more severe heart failure at admission. This suggests that this group includes more severe patients, whose condition makes it easier to recognize the need to activate the EMS. In addition, with regard to those with previous infarction, the education and knowledge gained during the previous event means that they are more likely to recognize the symptoms and therefore to use the EMS.13 By contrast, patients with preinfarction angina are less likely to use the EMS, which may be explained by the fact that since angina can be intermittent these patients tend to perceive their condition as being less serious. Furthermore, in the above study by Fujii et al., patients who presented chest pain as the initial symptom, as opposed to syncope, dyspnea or disturbed consciousness, were less likely to use the EMS, which to some extent shows patients’ lack of knowledge, or failure to recognize the symptoms of MI, particularly atypical manifestations.13
Clinical and experimental studies have shown a direct and continuous relationship between ischemic time, transmural necrosis and microvascular obstruction. Thus, greater benefit will be derived if blood flow is restored sufficiently early to prevent irreversible necrosis.14–16 In a study by Francone et al., the percentage of myocardial salvage as assessed by cardiac magnetic resonance imaging was higher in the patient group with TIT ≤90 min, and the extent of microvascular obstruction was less.17 Eitel et al. also showed that the myocardial salvage index was higher in the first two hours following symptom onset and that the strongest predictors of this index were complete ST-segment resolution, time from symptom onset to reperfusion and anterior infarction.18
Various recent studies have focused on DBT and its impact on clinical outcomes, but the results have been conflicting. Efforts to reduce DBT have not consistently been associated with reduced mortality.6,19 Some studies failed to show improved prognosis despite progressively shorter ischemic times.19–21 Our study found that although patients in the EMS group presented significantly shorter DBT and TIT, this was not reflected in lower mortality or fewer in-hospital major cardiac events. Similarly, although there was a trend for lower mortality in the EMS group at one-year follow-up, the survival curve diverging during follow-up, the difference was not statistically significant. These results are in line with those of large-scale studies, particularly that of Menees et al., which included 96738 STEMI patients undergoing PPCI, and showed that despite annual reductions in DBT, in-hospital and short-term mortality rates remained unchanged, even after analysis of risk subgroups.19 A Portuguese study by Bettencourt et al. also showed that although use of the EMS had a significant impact on reducing ischemic times, this was not reflected in significant differences in clinical course or in-hospital or one-year mortality.22 On the other hand, several other studies have reported an association between reductions in DBT and improved clinical outcomes.23,24 Such conflicting results may be due to the presence of multiple confounding factors. While DBT is an essential component, it does not fully reflect TIT since it does not take into consideration the time between symptom onset and admission, and does not necessarily mean significantly shorter TIT. A study by Prasad et al., which assessed the effect of TIT and DBT on microvascular perfusion, showed that TIT is an independent predictor of impaired myocardial perfusion as determined by both reduced myocardial blush grade and incomplete resolution of ST-segment elevation, and that this is associated with three-year mortality. DBT of ≤90 min only had an impact in patients with TIT of less than two hours.25 Other studies, such as those of Solhpour et al.26 and Sardar et al.,27 which compared the impact of reductions in TIT and DBT, showed that TIT is a better predictor of infarct size and 30-day mortality. Shiomi et al. also showed that a reduction in DBT was independently associated with lower risk for the composite endpoint of death and heart failure in patients who presented early (≤120 min) but not in those who presented later, which highlights the importance of seeking rapid medical attention.28 Many patients present late, outside the critical window for myocardial salvage. This may partly explain our results, since although the EMS helped to reduce ischemic times, median TIT in both groups was over two hours, which may have lessened the potential benefit of shorter DBT. However, in recent years, new reperfusion techniques and drug therapies have led to a significant reduction in mortality due to STEMI.2,6 Great emphasis has been placed on DBT and various efforts have been made to reduce it, not only during the pre-hospital period but also during in-hospital triage and management. In our study, even though the EMS group had significantly shorter DBT, both groups presented DBT of ≤90 min, with a median difference of 29 min. This raises the question of what benefits in terms of clinical outcomes can be expected from a modest reduction in ischemic times, particularly in an era in which mortality is already relatively low. DBT may now have reached the point where further reductions will have little impact on in-hospital or short-term mortality but may affect long-term outcomes or future hospitalizations for heart failure.6,14 However, our study showed that patients who presented earlier (DBT ≤60 min) had a significantly higher rate of effective reperfusion (particularly those in the EMS group), and that this was independently associated with significantly lower in-hospital mortality. This reflects the beneficial effect of early presentation on angiographic results and its correlation with in-hospital clinical outcomes.
When analyzing the impact of ischemic times on clinical outcomes, other confounding variables should be taken into account. Patients with longer DBT may have had other reasons for delay in seeking medical attention, including comorbidities or a more severe clinical setting that required stabilization before PPCI, which in itself would confer a worse prognosis. Furthermore, patients who use the EMS may generally have less favorable characteristics. In our study, the percentage of patients in Killip class III/IV at admission was significantly higher in the EMS group, and this parameter, together with age and moderate/severe left ventricular dysfunction, was an independent predictor of cumulative mortality. The time from symptom onset may not in fact correspond to TIT; many patients present silent ischemia, atypical or fluctuating symptoms with prodomal angina, which can make it difficult to establish the actual time of symptom onset. In addition, as in other studies on this subject, our analysis did not include patients who died before reaching hospital, which introduces a survival bias.4,6,13,19,29
Reducing TIT in the context of STEMI should still be a priority. There are many benefits, especially in areas without ready access to PPCI and in patients who present late. Additional efforts to raise awareness among the general public of the symptoms of MI and of the importance of seeking early treatment, aimed at reducing delays in seeking medical attention and in transport (particularly by using the pre-hospital EMS), may lead to more patients presenting in the first hours of ischemia when the benefits are greatest, which will undoubtedly be reflected in clinical outcomes.
LimitationsThe study has the limitations inherent to its retrospective, observational nature and the fact that it is based on the experience of a single center and may not therefore be fully representative of the situation in the country as a whole. The study did not include patients who suffered sudden death before coronary angiography could be performed, nor did it analyze those who underwent resuscitation by EMS teams, which means that the true impact of the EMS on mortality may be underestimated. Presenting symptoms, socioeconomic data and educational levels of the study population were not analyzed, nor were the reasons that they did or did not activate the EMS.
ConclusionOur study found that recourse to the EMS significantly reduced ischemic times. Although this improvement was not directly associated with significant differences in mortality or in-hospital or one-year clinical outcomes, it was associated with higher rates of effective reperfusion that were reflected in lower in-hospital mortality. Recent years have seen a trend for increased use of the EMS, albeit still less than desirable, and a significant percentage of patients continue to present late, with TIT of >120 min. New measures and increased efforts to raise awareness among the general population should continue in order to improve the prognosis of STEMI patients.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Silveira I, Sousa MJ, Rodrigues P, Brochado B, Santos RB, Trêpa M, et al. Evolução e impacto do transporte pré-hospitalar em doentes com enfarte agudo do miocárdio com elevação do segmento ST. Rev Port Cardiol. 2017;36:847–855.