Portugal has one of the lowest rates of primary percutaneous coronary intervention (p-PCI) in Western Europe. This study assessed the progress of Portuguese p-PCI performance indicators one year after Portugal joined the Stent for Life (SFL) initiative.
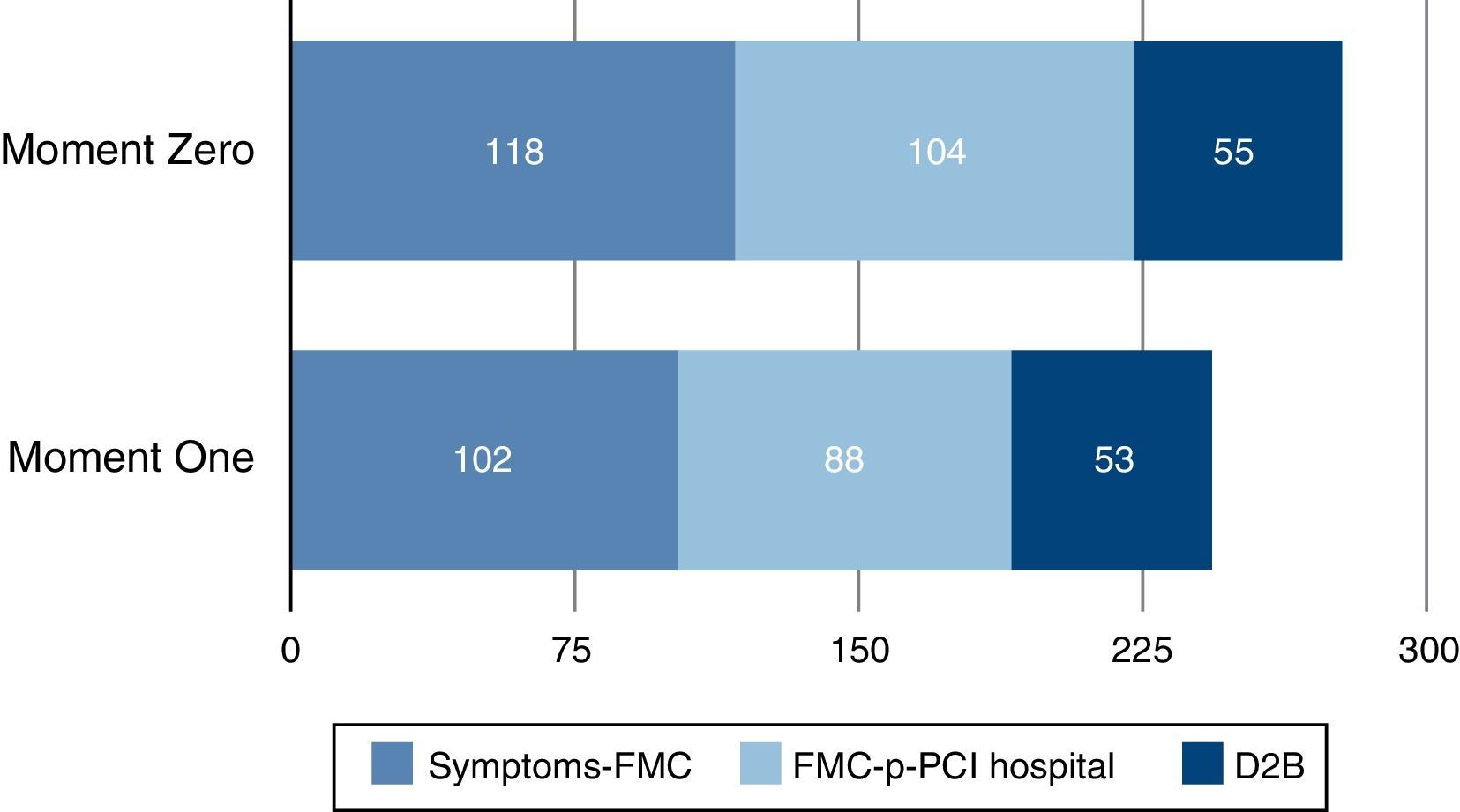
Methods and ResultsTwo national surveys were carried out, each covering a period of one month: the first when Portugal joined the SFL in 2011 (Moment Zero), and the second one year later (Moment One). A total of 397 consecutive patients with probable ST-segment elevation myocardial infarction were enrolled (201 at Moment Zero and 196 at Moment One) from 15 centers. During this period, the number of patients who arrived at a local hospital without p-PCI decreased (62–47%; p=0.004) and transportation to a p-PCI hospital by the National Institute for Medical Emergencies (INEM) increased significantly (13–37%; p<0.001). Shorter times to revascularization were observed, due to shorter patient delay (118–102 min; p=0.008). Door-to-balloon delay and system delay remained unchanged.
ConclusionsImprovements in performance indicators for p-PCI demonstrate the success of the first year of the local SFL plan, which was mainly focused on raising public awareness of the need to use the INEM emergency services, which has reduced patient delay, and on improving secondary transportation.
Portugal é um dos países europeus que apresenta uma das mais baixas taxas de angioplastia primária (p-PCI). O objetivo deste estudo foi avaliar os indicadores de performance, em termos de p-PCI, um ano após Portugal ter integrado a Iniciativa Stent for Life (SFL).
Métodos e resultadosforam efetuados dois inquéritos nacionais, com a duração de um mês, o primeiro em 2011, no momento inicial de integração do projecto SFL em Portugal («Momento Zero») e o segundo em 2012 após um ano de atuação («Momento Um»). Foram incluídos 397 doentes consecutivos submetidos a cateterismo por suspeita de enfarte agudo do miocárdio com supradesnivelamento de ST (EMSST), em 15 centros nacionais de cardiologia de intervenção (201 Momento Zero, 196 Momento Um). Ocorreu uma redução significativa dos doentes que recorreram a centros sem cardiologia de intervenção (62% versus 47%, p=0,004) e aumentou o transporte dos doentes pelo sistema nacional de emergência médica (INEM) para um centro com ICP primária (13% versus 37%, p<0,001). A principal melhoria observada nos intervalos de tempo para a revascularização, foi no «atraso do doente» (118 minutos no «Momento Zero» diminuiu para 102 minutos no «Momento Um», p=0,008). O «tempo porta-balão» manteve-se constante.
Conclusãoa melhoria dos indicadores de desempenho da rede nacional de tratamento do enfarte do miocárdio com supradesnivelamento de ST aponta para o sucesso do plano de ação da Iniciativa Stent for Life, que neste primeiro ano se centrou na sensibilização da população para recurso ao INEM em caso de suspeita de enfarte, e na realização do transporte interhospitalar por esta instituição.
Referral Center for Emergency Patients
door-to-balloon
door-to-door
electrocardiogram
European Society of Cardiology
first medical contact
National Institute for Medical Emergencies
myocardial infarction
primary percutaneous coronary intervention
Stent for Life
ST-segment elevation myocardial infarction
The Stent for Life (SFL) initiative aims to improve the delivery of facilities that will reduce mortality and morbidity in patients with ST-segment elevation myocardial infarction (STEMI), by increasing timely access to primary percutaneous coronary intervention (p-PCI).1,2 A 2010 study that compared how patients with STEMI were treated in different European countries reported that there was a low rate of p-PCI in Portugal, as well as a high proportion of patients who did not receive any reperfusion therapy.3
Several countries participating in the SFL initiative have reported encouraging results, with a significant increase in the rate of p-PCI per million population.4–11 Portugal was one of the latest countries to join SFL, in February 2011, and a local action program has been implemented to increase patient access to p-PCI and to improve its quality, mainly by reducing the time between symptom onset and p-PCI.
The SFL Portugal initiative implemented a national survey to characterize STEMI treatment that included all centers on the Portuguese mainland with an interventional cardiology unit available 24/7 and which followed p-PCI protocols. A prospective registry was set up for one month, from May 9 to June 8, 2011 (“Moment Zero”).12 This study revealed that the time between symptom onset and first medical contact (FMC) was too long, and that only one-third of patients requested medical assistance from the Portuguese emergency medical system, the National Institute for Medical Emergencies (INEM). Consequently, more than half of the patients attended local hospitals without interventional cardiology units.
The SFL Portugal Task Force set out an action plan with three main aims: (1) to launch a national public campaign to raise public awareness of the symptoms of myocardial infarction (MI) and of the actions that should be taken to ensure timely and appropriate treatment; (2) to cooperate with INEM to improve patient routing, by enabling direct admission to a hospital with p-PCI facilities (“p-PCI hospital”) and transfer from hospitals without interventional cardiology units to a p-PCI hospital; (3) to improve hospital performance in the treatment of STEMI by p-PCI.
To assess the impact of these actions, in 2012, exactly one year after the Portugal SFL initiative was launched, a new registry was set up for one month, designated Moment One.
MethodsStudy design and data collectionA national survey was carried out in 15 centers in Portugal equipped for p-PCI, with an interventional cardiology unit available 24/7, to record all consecutive catheterized patients with a presumed diagnosis of STEMI for a period of one month (May 9–June 8). Patients who received fibrinolytic therapy prior to being transferred from another hospital were excluded from the study.
The survey was carried out in each center at two time points: the first immediately after Portugal joined the SFL initiative (Moment Zero), and the second one year later, in 2012 (Moment One). The patients’ demographic variables and cardiovascular history were recorded.
Data collected also included the number of patients who used the national medical emergency number (112) to obtain direct assistance from INEM, who are responsible for pre-hospital transportation. The type of FMC was registered, as well as the transportation used to attend the center for p-PCI. It was also recorded whether the patient attended another hospital or healthcare facility before arriving at an institution with p-PCI.
The two time points (Moment Zero and Moment One) were compared in terms of time between symptom onset and p-PCI.
The rates of timely delivery of p-PCI were analyzed according to the guidelines of the European Society of Cardiology17: the recommended time between FMC and the first electrocardiogram (ECG) should be ≤10 min, and from FMC to p-PCI should be ≤90 min. However, in p-PCI hospitals, door-to-balloon (D2B) time (time between presentation at the p-PCI hospital and use of first device in the culprit artery) should be ≤60 min.
No data were collected regarding the clinical outcomes of the interventions performed.
SFL Task Force strategy for actionDuring the first year of the SFL initiative in Portugal, one of the major priorities was to reduce patient delay (time between symptom onset and FMC), by raising awareness of MI symptoms and of the actions that should be taken to ensure timely and appropriate treatment, especially the use of the 112 emergency call service. To achieve this goal, a national public campaign with the slogan “Não perca tempo. Salve uma vida” (“Act now. Save a life”) was launched in December 2011. SFL partners from different industries, including medical devices, pharmaceuticals, energy and telecommunications, helped to increase the visibility of the campaign in the media, while various educational activities, such as distribution of leaflets and screening for cardiovascular disease, were also carried out at clinics and shopping centers, in private companies and in the Portuguese Parliament.
Time measuresFMC was defined as the time at which medical personnel, including pre-hospital paramedical staff, arrived to attend the patient, or the time of arrival at a hospital equipped for fibrinolysis or p-PCI. The delays between symptom onset and p-PCI were defined as: (1) patient delay – the time between symptom onset and FMC; (2) pre-hospital transportation delay – the time between FMC by pre-hospital paramedical staff and hospital attendance; (3) local hospital delay or door-to-door (D2D) delay – the time between attendance at the local hospital and attendance at the p-PCI hospital; (4) door-to-balloon (D2B) delay – the time between attendance at the p-PCI hospital and use of first device in the culprit artery; (5) system delay – the time between FMC and reperfusion therapy (for patients who go directly to a p-PCI hospital, system delay corresponds to D2B, while for others, it is pre-hospital transportation delay plus D2B); and (6) treatment delay – the time between symptom onset and reperfusion therapy, corresponding to patient delay plus system delay.
Statistical analysisContinuous variables were expressed as mean±standard deviation, except time intervals, which were expressed as median and interquartile range. Categorical variables were summarized as absolute and relative frequency distributions. Independent Student's t-tests were used for group comparisons of continuous variables, while the chi-square test or Fisher's exact test was used for categorical variables.
The Mann–Whitney nonparametric test was used to compare time intervals between the two surveys (Moment Zero vs. Moment One). All tests were two-sided and assumed a significance level of 5%. All statistical analyses were performed using SPSS Statistics for Windows, version 17.0 (SPSS Inc., Chicago, USA).
ResultsBaseline demographic and clinical characteristicsOf the 19 centers that perform p-PCI in mainland Portugal, 15 participated in this study and included data from 397 patients (201 patients assessed and treated at Moment Zero and 196 at Moment One).
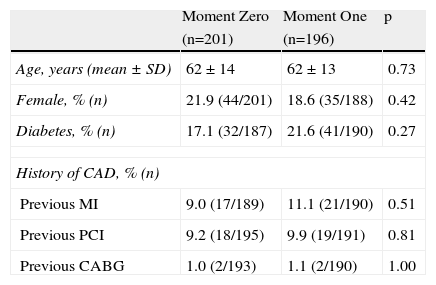
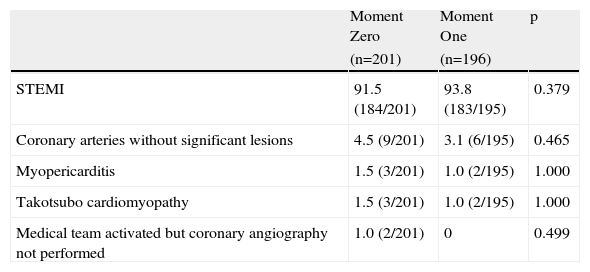
Table 1 presents the patients’ demographic data and clinical background. Mean age was 62±13 years, 20% were female and 18% presented a history of diabetes. The incidence of a history of cardiovascular disease was low and did not differ significantly between groups. A diagnosis of STEMI was confirmed in 92% of the patients (Table 2).
Demographics and clinical background.
| Moment Zero | Moment One | p | |
| (n=201) | (n=196) | ||
| Age, years (mean±SD) | 62±14 | 62±13 | 0.73 |
| Female, % (n) | 21.9 (44/201) | 18.6 (35/188) | 0.42 |
| Diabetes, % (n) | 17.1 (32/187) | 21.6 (41/190) | 0.27 |
| History of CAD, % (n) | |||
| Previous MI | 9.0 (17/189) | 11.1 (21/190) | 0.51 |
| Previous PCI | 9.2 (18/195) | 9.9 (19/191) | 0.81 |
| Previous CABG | 1.0 (2/193) | 1.1 (2/190) | 1.00 |
CABG: coronary artery bypass graft; CAD: coronary artery disease; MI: myocardial infarction; PCI: percutaneous coronary intervention; SD: standard deviation.
Diagnosis after medical team activation, % (n).
| Moment Zero | Moment One | p | |
| (n=201) | (n=196) | ||
| STEMI | 91.5 (184/201) | 93.8 (183/195) | 0.379 |
| Coronary arteries without significant lesions | 4.5 (9/201) | 3.1 (6/195) | 0.465 |
| Myopericarditis | 1.5 (3/201) | 1.0 (2/195) | 1.000 |
| Takotsubo cardiomyopathy | 1.5 (3/201) | 1.0 (2/195) | 1.000 |
| Medical team activated but coronary angiography not performed | 1.0 (2/201) | 0 | 0.499 |
STEMI: ST-elevation myocardial infarction.
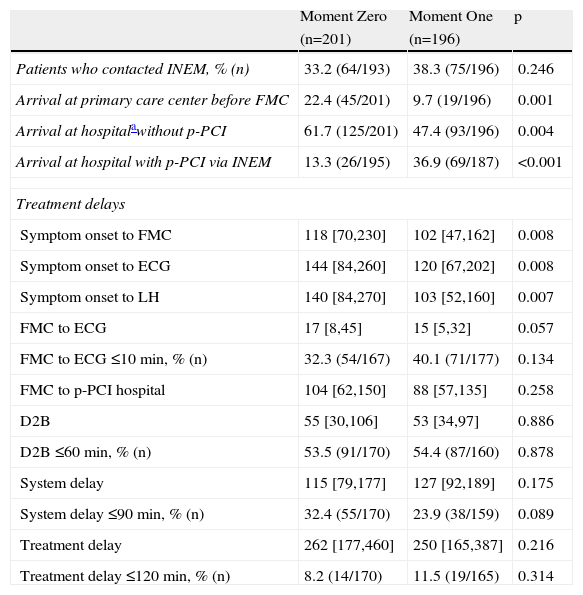
At Moment Zero, only 33% of the patients used the national medical emergency number, 112, to call for assistance. During this first year the main goal was to shorten patient delays. At Moment One, one year after Portugal joined the SFL initiative, an improvement of 5% (not statistically significant) was observed. On the other hand, the number of patients who first went to local hospitals without p-PCI facilities fell significantly, from 62% to 47% (p=0.004, Table 3).
Means of transportation to a p-PCI hospital and treatment delays.
| Moment Zero | Moment One | p | |
| (n=201) | (n=196) | ||
| Patients who contacted INEM, % (n) | 33.2 (64/193) | 38.3 (75/196) | 0.246 |
| Arrival at primary care center before FMC | 22.4 (45/201) | 9.7 (19/196) | 0.001 |
| Arrival at hospitalawithout p-PCI | 61.7 (125/201) | 47.4 (93/196) | 0.004 |
| Arrival at hospital with p-PCI via INEM | 13.3 (26/195) | 36.9 (69/187) | <0.001 |
| Treatment delays | |||
| Symptom onset to FMC | 118 [70,230] | 102 [47,162] | 0.008 |
| Symptom onset to ECG | 144 [84,260] | 120 [67,202] | 0.008 |
| Symptom onset to LH | 140 [84,270] | 103 [52,160] | 0.007 |
| FMC to ECG | 17 [8,45] | 15 [5,32] | 0.057 |
| FMC to ECG ≤10 min, % (n) | 32.3 (54/167) | 40.1 (71/177) | 0.134 |
| FMC to p-PCI hospital | 104 [62,150] | 88 [57,135] | 0.258 |
| D2B | 55 [30,106] | 53 [34,97] | 0.886 |
| D2B ≤60 min, % (n) | 53.5 (91/170) | 54.4 (87/160) | 0.878 |
| System delay | 115 [79,177] | 127 [92,189] | 0.175 |
| System delay ≤90 min, % (n) | 32.4 (55/170) | 23.9 (38/159) | 0.089 |
| Treatment delay | 262 [177,460] | 250 [165,387] | 0.216 |
| Treatment delay ≤120 min, % (n) | 8.2 (14/170) | 11.5 (19/165) | 0.314 |
Time values are presented as median [Q1, Q3] in minutes.
Regarding transportation, the number of patients transported to a p-PCI hospital by INEM increased significantly, from 13% to 37% between Moment Zero and Moment One (p<0.001). This was due to a greater number of patients using the 112 telephone number who were transported by emergency and resuscitation ambulances prepared to perform pre-hospital ECG (32% at Moment Zero vs. 68% at Moment One, p<0.001). Additionally, inter-hospital transfers to p-PCI centers began to be carried out by INEM (at Moment One, 31% of patients who went to local hospitals without p-PCI facilities were transferred by INEM to a p-PCI center).
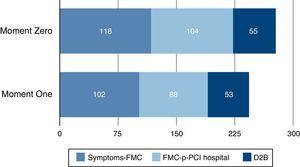
Treatment delays in the general populationOne year after the SFL initiative was launched in Portugal, the main positive impact was observed in patient delay, which had decreased significantly by Moment One (Table 3 and Figure 1). The median time from symptom onset to ECG and from symptom onset to arrival at a hospital without p-PCI also decreased between Moment Zero and Moment One, suggesting that patients are requesting assistance sooner.
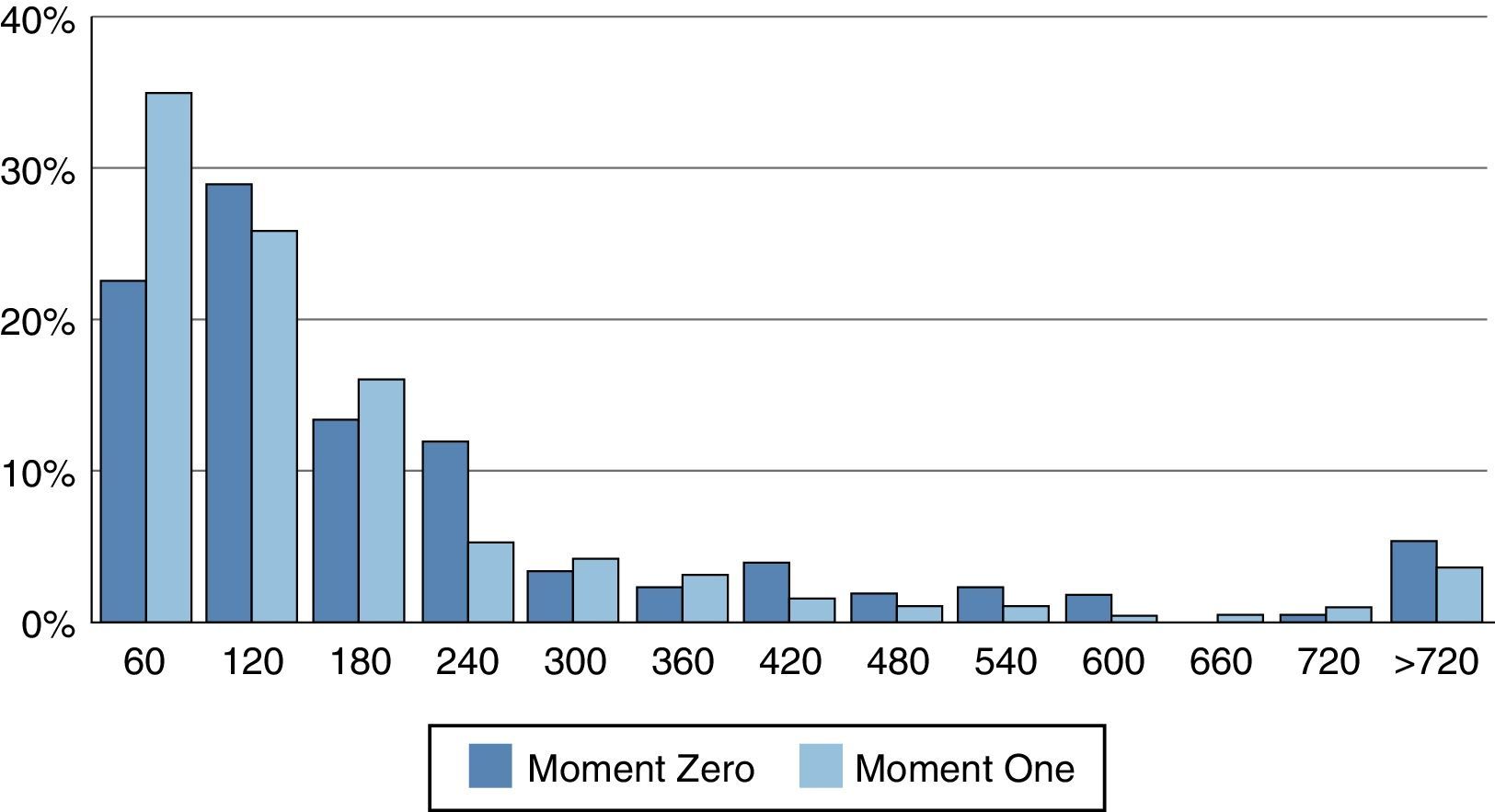
In both groups, 84% of the patients reached FMC within six hours of symptom onset. The number of patients who arrived at the hospital more than six hours after symptom onset had decreased at Moment One (17% at Moment Zero vs. 10% at Moment One, p=0.048). At the same time, an increase was observed in the number of patients arriving at the hospital within 30 minutes of symptom onset (9% at Moment Zero vs. 15% at Moment One, p=0.066) and within one hour of symptom onset (23% at Moment Zero vs. 35% at Moment One, p=0.007) (Figure 2).
The median system delay at Moment One was 127 minutes (interquartile range, 92–189), not significantly different from Moment Zero. The median treatment delay at Moment One was four hours, also not statistically different from the median treatment delay observed one year before.
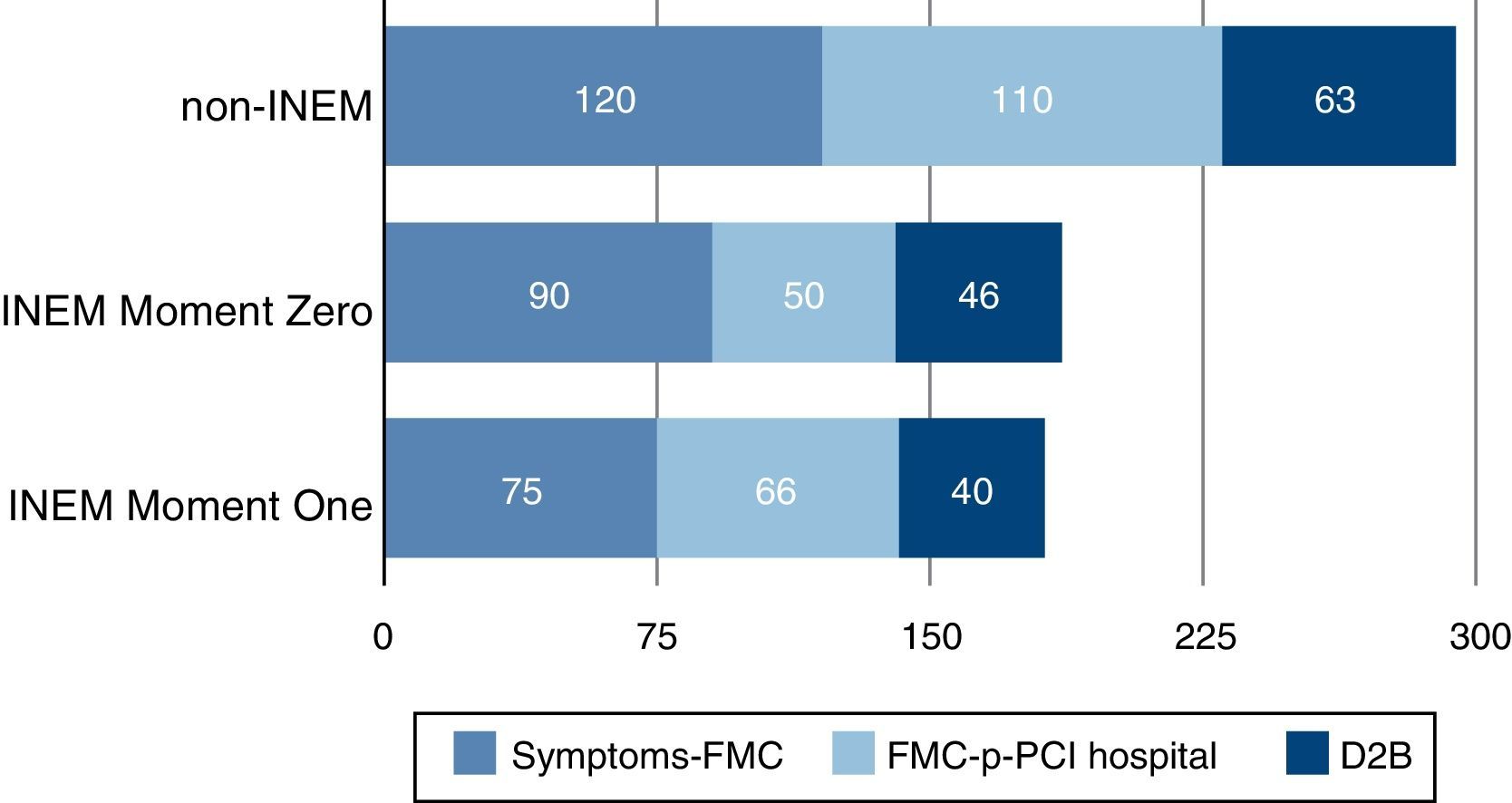
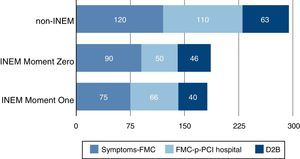
Treatment delay in patients transported to p-PCI hospitals by INEMOf the 397 patients enrolled in this study, 95 were transported to a p-PCI hospital by INEM (26 patients at Moment Zero and 69 at Moment One). At both points, transportation to a p-PCI hospital by INEM was associated with significantly shorter treatment delays, compared to patients who arrived at p-PCI hospitals by other means. Differences were observed in patient delay (78 min vs. 120 min, p<0.001); pre-hospital transportation delay (60 min vs. 110 min, p<0.001); D2B delay (42 min vs. 63 min, p=0.007); and treatment delay (211 min vs. 267 min, p=0.002). Regarding patients transported by INEM, patient delay and D2B delay did not differ significantly between Moment Zero and Moment One. On the other hand, the FMC to p-PCI hospital time was longer at Moment One than at Moment Zero in this subgroup (66 min vs. 50 min, p=0.044), following implementation of a new inter-hospital transportation system by INEM at Moment One (Figure 3). At Moment One, the D2D delay in the 27 patients transferred by INEM to a p-PCI hospital was significantly longer than the pre-hospital transportation delay of 42 patients directly transported by INEM to a p-PCI hospital without previously attending a local hospital without p-PCI (121 min vs. 52 min; p<0.001).
Treatment delays (in min) of patients transported by INEM vs. patients transported by other means to a p-PCI hospital. FMC: first medical contact; INEM: National Institute for Medical Emergencies (emergency medical system); non-INEM: transported by means other than INEM; p-PCI: primary percutaneous coronary intervention.
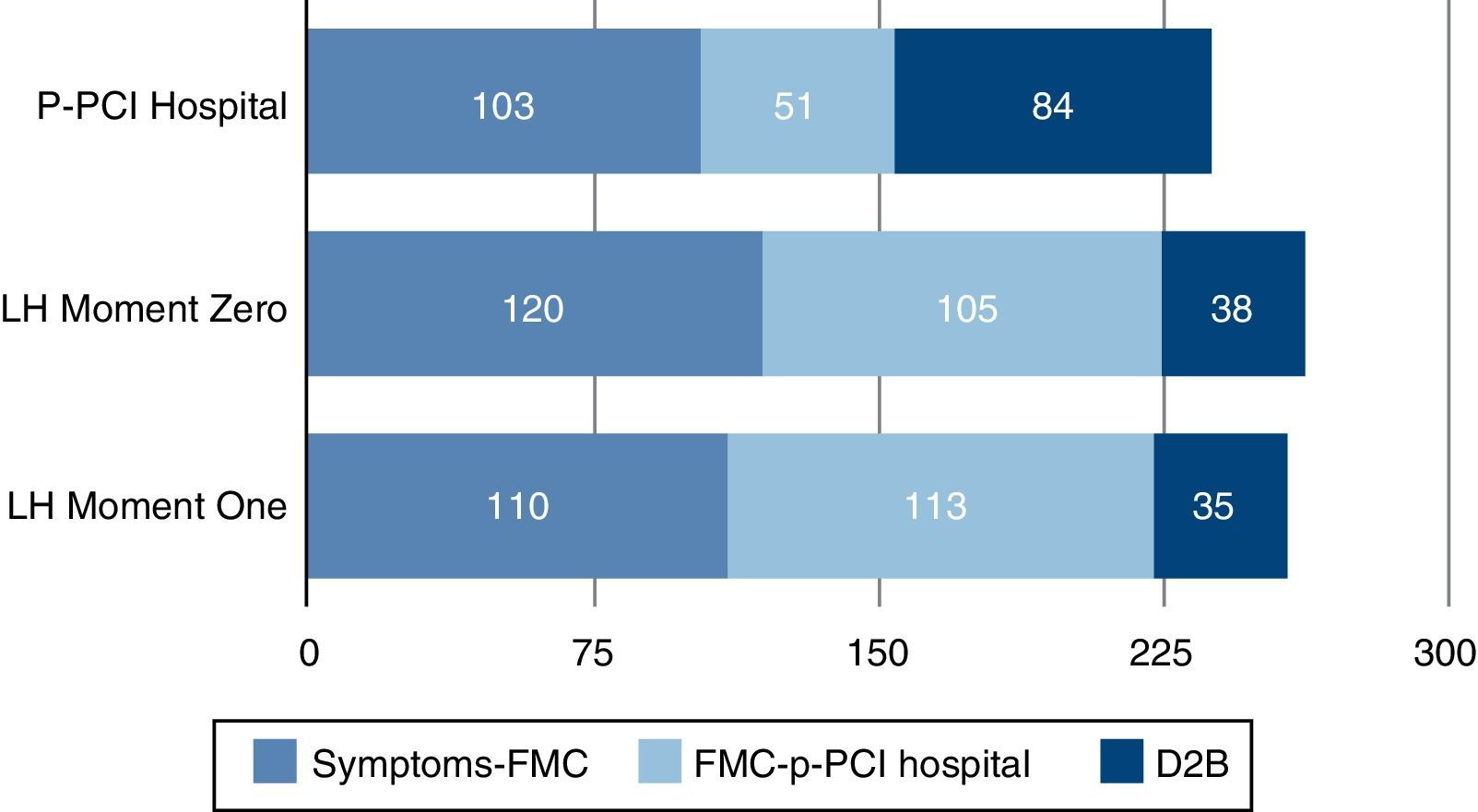
Overall, 55% of the patients attended a local hospital without p-PCI or a clinic (125 patients at Moment Zero and 93 patients at Moment One). A significantly greater treatment delay was observed for these patients (283 min vs. 223 min for patients arriving directly at a p-PCI hospital, p<0.001). D2B time was shorter in patients attending a local hospital and transferred after diagnosis to a p-PCI hospital (36 min vs. 84 min, p<0.001) compared to patients who went directly to p-PCI hospitals. On the other hand, D2D time was considerably longer than pre-hospital transportation time (109 min vs. 51 min, p<0.001), which resulted in a significantly greater system delay in patients undergoing inter-hospital transfer (140 min vs. 103 min, p<0.001). Patient transportation time to p-PCI hospitals was not statistically different between Moment Zero and Moment One (Figure 4).
DiscussionCardiovascular disease is the leading cause of mortality in Europe. MI, stroke and other cardiovascular diseases claim more than two million lives per year, and account for more than 40% of all deaths in the region.13
The SFL initiative was launched in 2008 by the European Association for Percutaneous Cardiovascular Interventions and EuroPCR together with the Working Group on Acute Cardiac Care of the European Society of Cardiology (ESC) and national cardiology societies of the participating countries.1,2,4 The SFL initiative is a three-year project aiming to reduce mortality and morbidity in patients suffering from STEMI in ESC member countries, by improving patient access to p-PCI.4
A 2008 study of Portuguese performance indicators reported that only 19% of the patients received p-PCI and a high percentage did not receive any revascularization therapy.3 According to a study by the Portuguese Cardiology Society (SPC) based on the Portuguese Registry of Acute Coronary Syndromes, in 55% of the STEMI patients who did not receive any form of revascularization therapy, the reason was hospital arrival more than 12 hours after symptom onset.14
For these reasons, the Portuguese Association of Cardiovascular Intervention proposed to join the SFL initiative, which it did in February 2011.
The SFL Portugal constituted a Task Force that defined a three-year action plan, with three major aims: (1) to increase the use of p-PCI to more than 70% of STEMI patients; (2) to achieve p-PCI rates of more than 500 per million population per year; (3) to improve the network of p-PCI centers offering a 24/7 catheterization service.
From May to June 2011, a national survey was carried out for one month, to evaluate performance indicators at the beginning of the SFL initiative in Portugal, designated Moment Zero. The results from this first survey gave an up-to-date picture of how STEMI patients were treated in Portugal and identified the main barriers to improving the p-PCI program in Portugal as being long symptom onset to FMC times, the low number of patients who contacted the national medical emergency number (112), and the high number of patients (more than half) who attended centers without p-PCI facilities.12
To overcome these barriers, the SFL Portugal Task Force developed an action plan with three main aims: (1) to launch the national public campaign “Act now. Save a life”, in order to raise public awareness of the symptoms of MI and to encourage people to call the national medical emergency number (112) immediately; (2) to collaborate with INEM to improve direct communication between pre-hospital services and p-PCI equipped hospitals and to provide transportation from hospitals without interventional cardiology units to p-PCI hospitals; (3) to implement a national plan enabling access to p-PCI for all STEMI patients, through INEM and its operational center, the Referral Center for Emergency Patients (CODU).
Achievements during the first year of the SFL Portugal initiativeAction 1: Educational information in the form of leaflets, pins and posters was distributed to raise public awareness of MI symptoms and the need to act quickly and call 112. A website (www.stentforlife.pt) was set up to introduce the SFL initiative and its work in Portugal. SFL partners from different industries, including medical devices, pharmaceuticals, energy and telecommunications, have helped to increase the visibility of the campaign in the media. The campaign was widely covered by newspapers (with an average of 26 news segments or articles per month), radio and TV (with over two hours of coverage on three national television channels in eight months).
Action 2: During the first year of the SFL Portugal initiative, INEM began to contact cardiologists operating at p-PCI hospitals directly, by telephone. In addition, all INEM ambulances were equipped with telemetry and facilities to transfer ECGs to p-PCI hospitals. In most cases, this enabled patients to be transferred immediately to the catheterization laboratory without first passing through the emergency room, minimizing delay. Later, a new inter-hospital transportation system was also implemented; during 2012, INEM began to take over patient transfer from local hospitals to hospitals with interventional cardiology units, which will soon be implemented at the national level.
Action 3: According to the Portuguese Registry of Acute Coronary Syndromes, the rate of fibrinolysis has decreased substantially. In 2011 only 7% of the STEMI patients were reperfused by fibrinolysis and 25% did not receive any form of revascularization. No studies or official data are yet available, but based on information from countries with better performance in this field, we estimate that a substantial number of patients do not receive any form of reperfusion and some patients treated by fibrinolysis could have been treated by p-PCI instead. For patients treated by fibrinolysis, it is not known whether they underwent early coronary angiography in accordance with the relevant guidelines. The Task Force aims to implement a national strategy to provide p-PCI to all STEMI patients, discouraging fibrinolysis whenever the patient can be transferred by INEM to a p-PCI hospital. If a STEMI patient presents at a hospital unable to provide p-PCI, CODU should be contacted immediately and asked: “Can this patient be treated by p-PCI in less than 120 min?” Fibrinolysis should only be performed if the answer is negative. In either case, INEM should immediately transfer the patient to a 24/7 p-PCI center to perform further coronary angiography, pharmacoinvasive therapy or rescue angioplasty.
The present study, designated Moment One, was carried out exactly one year after Moment Zero and sought to evaluate the progress of Portuguese performance indicators for p-PCI one year after joining the SFL initiative.
Improvements were observed in key performance indicators, such as an increase in the number of patients using the national medical emergency number (112) to call for assistance, from 33% in 2011 to 38% in 2012. From the available data it is not possible to determine whether this outcome is a direct result of the SFL campaign; in order to be effective, such campaigns should be prolonged and persistent.15 Moreover, there are limitations to the availability of the INEM service, and patients may therefore be referred to other means of transportation. However, improvements were also observed in this aspect, since the number of STEMI patients transported by INEM increased from 13% at Moment Zero to 37% at Moment One.
Another important change is the fall in the number of patients initially arriving at hospitals without p-PCI, from 62% to 47%. Additionally, INEM began to provide inter-hospital secondary transportation, which accounted for 31% at Moment One. This new approach to inter-hospital patient transfer is intended by the SFL to be widened to all STEMI patients, to provide p-PCI, pharmacoinvasive therapy or rescue angioplasty.
The SFL initiative aims not only to increase the number of patients treated by p-PCI in Portugal, but also to improve the quality of such therapy. In this context, delays between symptom onset and use of first device in the culprit artery are excellent quality indicators.16
The most notable improvement was observed in patient delay, which decreased from 118 min at Moment Zero to 112 min at Moment One. In particular, a greater number of patients reached FMC within one hour of the first symptom (23% vs. 35%).
Treatment delay did not change significantly between the two time points (262 min at Moment Zero, and 250 min at Moment One), and no significant differences were found in system delay (115 min at Moment Zero, and 127 min at Moment One), or for time between FMC and ECG.
The essential role of INEM in STEMI patient care was highlighted by significantly shorter treatment delay when transportation to a p-PCI hospital was carried out by INEM (211 min vs. 267 min for patients arriving at the hospital by other means). Transportation by INEM is associated not only with reduced pre-hospital transport times, but also with shorter patient delay and system delay. The increase in median pre-hospital transport time observed at Moment One was due to the implementation of inter-hospital transfer by INEM. Patients transferred from centers without p-PCI to hospitals with interventional cardiology units presented longer times than recommended between FMC and p-PCI hospital (121 min), probably as a result of delays in hospitals without p-PCI.
The most important indicator was probably the fact that patients arriving at a local hospital without an interventional cardiology unit spent more time in inter-hospital transfer (transportation time: 109 min) than those transported directly to a p-PCI hospital by INEM (transportation time: 51 min). For this reason, the SFL initiative should continue and the “Act now. Save a life” campaign should be intensified.
As previously reported,12 this study demonstrates again that D2B time is not a good performance index. Although D2B times (55 min at Moment Zero and 53 min at Moment One) were shorter than those in the ESC guidelines,17 they do not reflect the very long treatment delays and the overall performance of p-PCI in Portugal.
The latest ESC guidelines state that, in order to optimize STEMI treatment, a hospital network should be implemented and coordinated with pre- and inter-hospital transportation to minimize treatment delays.17 According to these guidelines, systems for data recording, monitoring and quality control should also be implemented.
To summarize, one year after implementation of the SFL initiative in Portugal, we observed a positive impact, with greater use of the 112 emergency call service and a smaller number of patients arriving by their own means at local hospitals without p-PCI facilities. Patient delay was identified at Moment Zero as a major barrier to p-PCI performance.12 However, a considerable improvement was observed in this area, indicating that the SFL's public awareness campaign is progressing successfully and should be intensified. Although system delays are similar to those recommended by the guidelines, the SFL initiative will focus next year on further improving overall system performance.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
Hospital Vila Real (Dr. Henrique Carvalho), Hospital Braga (Dr. João Costa), Hospital S. João (Dr. João Carlos Silva), Hospital Santo António (Dr. Henrique Carvalho), Centro Hospitalar Vila Nova de Gaia (Dr. Vasco Gama Fernandes), Hospital de Viseu (Dr. João Pipa), Centro Hospitalar de Coimbra (Dr. Leitão Marques), Hospital de Leiria (Dr. João Morais), Hospital Fernando da Fonseca (Dr. Pedro Farto e Abreu), Hospital de Santa Maria (Dr. Pedro Canas da Silva), Hospital Santa Cruz (Dr. Manuel Almeida), Hospital da CUF (Dr. Sousa Ramos), Hospital Pulido Valente (Dr. Pedro Cardoso), Hospital de Santa Marta (Dr. Rui Ferreira), Hospital Curry Cabral (Dr. Luís Mourão), Hospital Garcia de Orta (Dr. Hélder Pereira), Hospital Setúbal (Dr. Ricardo Santos); Hospital de Évora (Dr. Lino Patrício e Dr. Renato Fernandes), H de Faro (Dr. Victor Brandão).


 D2B: door-to balloon delay;
D2B: door-to balloon delay; 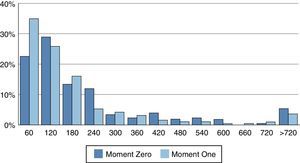
 INEM vs. patients transported by other means to a
INEM vs. patients transported by other means to a 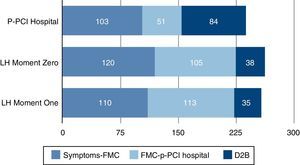 FMC: first medical contact; LH: local hospital;
FMC: first medical contact; LH: local hospital; 
