A 62-year-old man with a history of smoking and alcohol consumption went to the emergency room due to a one-week history of coughing and progressively worsening dyspnea (especially when in a left lateral decubitus position), as weight loss over one month.
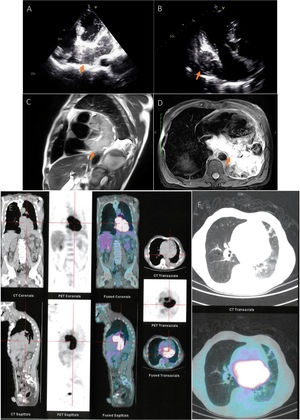
The echocardiogram (Figure 1A and B) showed a cardiac mass occupying the pericardial cavity and the left atrium (LA), with a maximum diameter of 28 mm. Chest computed tomography (CT) showed a large nodular formation in the LA. The lesion was heterogeneous (96 mm×57 mm), and invading adjacent structures. Cardiac magnetic resonance imaging (Figure 1C and D) revealed a paracardiac mass in the posterior mediastinum, extending from the pulmonary artery (PA) to the diaphragm (91 mm×63 mm×110 mm), infiltrating the LA (27 mm) and the left branch of the PA. It was isointense on T1 and hyperintense on T2.
(A) Transthoracic echocardiogram showing cardiac mass involving the left atrium in four-chamber view and (B) in three-chamber view (arrows). (C and D) Cardiac magnetic resonance imaging revealing a posterior mediastinal mass with cardiac infiltration (arrows). (E and F) Positron emission tomography/computed tomography showing a hypermetabolic mass located in the posterior mediastinum.
Positron emission tomography/CT (PET/CT) showed a hypermetabolic mass located in the posterior mediastinum (Figure 1E and F), no cleavage planes with adjacent structures, which are characteristics of a malignant lesion. Additionally, there was paratracheal, hilar and infraclavicular adenopathy. He underwent a biopsy of the mediastinal lesion, and a diagnosis of diffuse large B-cell lymphoma (Ann Arbor II-A stage) was made.
He began R-CHOP therapy (rituximab, cyclophosphamide, doxorubicin, vincristine, prednisone) with a favorable clinical response.
PET/CT was subsequently repeated, which showed a significant reduction of the mass, and only a small hypodense defect in the atrium. However, the patient became infected with SARS-CoV2 and died four months after starting treatment.
The authors suggest that in this case tumor invasion of the left PA caused a ventilation-perfusion imbalance. This was exacerbated by the left lateral decubitus position, since there is a relative reduction in perfusion of the right PA by gravity. Additionally, left lateral decubitus potentially leads to a partial obstruction of the pulmonary veins, reducing atrial blood inflow and exacerbating pulmonary edema.
Conflicts of interestThe authors have no conflicts of interest to declare.