Transient ST-segment elevation occurring in the context of percutaneous cardiac interventions has not been fully characterized. We present a case of an inferior ST-segment elevation associated with angina and hypotension following percutaneous mitral valvuloplasty. Coronary angiography during ST elevation found no abnormalities and no myocardial necrosis was documented. Thus, as the Inoue balloon had been reinflated and overinflated, we suggest that mechanical myocardial compression might be responsible for the transmural transient ischemia observed in some cardiac percutaneous procedures involving balloons or closure devices.
Elevaçãotransitória do segmento ST ocorrem no contexto de intervençõespercutâneas cardíacas nãofoi completamente caracterizado. Apresentamosum caso de umaelevação inferior do segmento ST associadacom angina e hipotensãoapós plastia mitral percutânea. A coronariografia durante a elevação do ST nãoencontrou anormalidades e sem necrose miocárdica foi documentada. Assim, quando o balão de Inouetinha sido reinflated e inflacionado, sugerimos que a compressãomecânica do miocárdio pode ser responsável pela isquemia transiente transmural observada emalgunsprocedimentospercutâneos cardíacas envolvendobalõesou dispositivos de fecho.
The most frequent risks associated with percutaneous mitral valvuloplasty (PMV) are cardiac tamponade and systemic embolism related to transseptal puncture and manipulation of catheters or wires inside the cardiac chambers, and increases in mitral regurgitation after balloon inflation.1 We present an uncommon and less understood complication of this procedure.
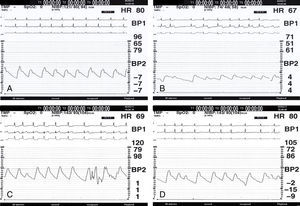
A 55-year-old Caucasian man was admitted to our hospital complaining of dyspnea and edema of ten days’ duration. Two years before, he had had a first episode of atrial fibrillation (AF) and was diagnosed with moderate mitral stenosis at that time. Although he had been asymptomatic, anticoagulated and in sinus rhythm in recent months, the patient was once more in AF with fast ventricular response (110–120bpm) that required high doses of beta-blockers and digoxin to control. The echocardiogram now showed a rheumatic mitral valve with a mean gradient of 6mmHg, an area of 1.2cm2 and a Wilkins score of 6. In the absence of formal contraindications, PMV following the Inoue technique was performed with a 28-mm balloon (patient's height 165cm). There were no complications during septal puncture (Figure 1A), so the balloon was inflated initially to 28mm four times and for the last time to 30mm (Figure 2A). Immediately following the final inflation, a new ST-segment elevation in the inferior leads was recorded on the ECG and the patient started complaining of severe chest pain. His blood pressure also dropped significantly (Figure 1B), and intravenous phenylephrine was administered to normalize it. At this time, as the patient's angina was worsening, it was decided to perform coronary angiography. After intracoronary nitroglycerin administration (200μg), though the ST segment remained elevated (Figure 1C), coronary angiograms showed right coronary dominance with TIMI flow grade 3 and no significant lesion, spasm, thrombus or air embolism (Figure 2B and C). A few minutes later the condition resolved (Figure 1D) and did not recur. During hospital stay there were no more complications and the patient was discharged with a transmitral mean gradient of 3mmHg and mild mitral regurgitation, and without documented myocardial injury (maximum troponin T 0.03ng/ml and no wall motion abnormalities on the echocardiogram).
Electrocardiogram and invasive blood pressure (BP) records during percutaneous mitral valvuloplasty (PMV). (A) Isoelectric ST segment and normal BP before performing PMV; (B) after last balloon inflation to 30mm, a new ST-segment elevation in lead II accompanied by significant BP drop is recorded; (C) intravenous phenylephrine was required to normalize BP, but the ST segment remained elevated so coronary angiography was performed at this time; (D) the condition resolved spontaneously in a few minutes, the ST segment and BP returning to baseline levels.
In an international series of PMVs published some years ago, Vahanian et al.2 described transient inferior ST-segment elevation with no or minor chest pain after Inoue balloon deflation in 10 patients (2.6%). The right coronary artery presented no abnormalities, so they attributed the episodes to air microembolisms. In another series of 108 PMVs, Ludman et al.3 identified eight patients (7.4%) with transient inferior ST-segment elevation just after crossing the interatrial septum with the balloon but before any inflation. Seven patients reported angina but there were no changes in blood pressure. Symptoms resolved after 1–2minutes and right coronary angiography performed in three patients showed no spasm or thrombus, so the authors rejected microembolism as a cause and subsequently proposed a neurally-mediated mechanism.4
Our case presents several differences from previous reports. The patient was very symptomatic (severe angina and blood pressure drop), and ST-segment elevation persisted for more than seven minutes. In addition, heart rate did not decrease in parallel with blood pressure, so we consider vagal stimulus unlikely. Coronary embolism is also questionable as no significant elevation in troponin T levels was observed in the following days and coronary flow during angina and ST-segment elevation was completely normal. So given the absence of spasm on the angiogram (although this cannot be totally excluded), we suggest that mechanical myocardial compression induced by repeated inflations and overinflation of a 28-mm balloon to 30mm might have led to transient transmural ischemia in the inferior basal segments. This mechanism might be responsible for some of the ST-segment changes observed during PMV and other percutaneous interventions.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.