We present the case of a 50-year-old patient with several episodes of syncope and documented simultaneous wide and narrow QRS complex tachycardia. We then review this tacharrhythmia, focusing on electrophysiological findings and pathophysiology, diagnosis and treatment.
Apresentamos um caso de um doente de 50 anos com diversos episódios de síncope e documentação de taquicardia com complexo QRS simultaneamente largo e estreito. Fazemos uma revisão desta taquiarritmia tendo em especial atenção achados electrofisiológicos e fisiopatologia, diagnóstico e tratamento.
We present the case of a 50-year-old patient with several episodes of syncope and documented simultaneous wide and narrow QRS complex tachycardia. We then review this tachyarrhythmia, focusing on electrophysiological findings and pathophysiology, diagnosis and treatment.
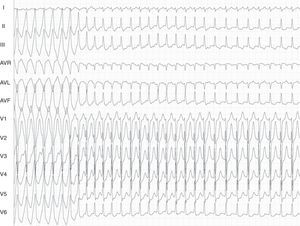
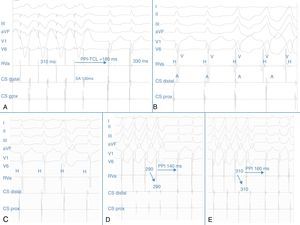
Case reportA 50-year-old man presented to the emergency department due to an episode of palpitations and dizziness. He reported several episodes of sudden syncope. The standard 12-lead electrocardiogram (ECG) performed on admission showed a wide QRS complex tachycardia, which changed spontaneously into a narrow QRS complex tachycardia (Figure 1) and vice versa. Blood pressure during the episode was 90/65mmHg. Due to the fact that the tachycardia was repetitive, bisoprolol was administered intravenously and sinus rhythm was restored. An emergency echocardiogram revealed no evidence of structural heart disease. An electrophysiological study (EPS) was subsequently performed. A bipolar catheter was placed initially in the right ventricular (RV) apex (afterwards withdrawn towards the His position) and a quadripolar catheter in the coronary sinus (CS). Ventricular stimulation performed from the right RV apex showed decremental retrograde conduction with a proximal to distal activation sequence in the CS. Programmed atrial stimulation revealed a dual AV nodal physiology with an AH jump and subsequent induction of atrioventricular nodal reentrant tachycardia (AVNRT). The diagnosis of AVNRT was based on the long postpacing interval (PPI) during entrainment of the tachycardia from the RV apex (PPI-TCL=180ms) (Figure 2A), septal VA interval of -10ms (Figure 2A), a stimulus-atrial (during pacing from the RV apex) minus ventriculo-atrial (during tachycardia) interval greater than 85ms, and absence of fusion during entrainment of the tachycardia. As in the baseline ECG, runs of wide QRS complex tachycardia with left bundle brunch morphology (LBBB) interacting with the narrow QRS tachycardia were also observed. The intracardiac signal during the latter confirmed that it was a ventricular tachycardia (VT) (Figure 2B) (VA dissociation, without anterograde His potential). Another interesting finding was the absence of atrial advancement by spontaneous single ventricular extrastimuli when the His bundle was refractory (Figure 2C). Transient entrainment of the AVNRT by non-sustained VT was also seen. During this phenomenon, the interval from the last beat of the VT to the first beat of the SVT minus the tachycardia cycle length (TCL) [(VVT − VSVT) − TCL] was longer than 115ms (Figure 2C and D), suggesting AVNRT, and making the diagnosis of an orthodromic septal tachycardia unlikely.
Twelve-lead ECG. In the first part of the tracing a broad QRS tachycardia is shown, with LBBB inferior axis morphology and negative QRS complex in aVL. After this run there is a change to a narrow QRS complex. Surface leads (I, II, III, aVF, V1 and V6), and electrograms recorded from the right ventricular apex and the coronary sinus.
(A): The long postpacing interval (PPI-TCL>180ms) after tachycardia entrainment from the right ventricular apex and the tachycardia cycle length are shown; (B): intracardiac recordings during the tachycardia. The first two beats correspond to an AVNRT, and the last three to the ventricular tachycardia. Note the absence of His bundle deflection and variable retrograde conduction during the runs of broad complexes; (C): absence of atrial advancement by spontaneous extrastimulus when the His bundle was refractory; (D and E): transient entrainment of the AVNRT by the spontaneous non-sustained ventricular tachycardia is observed, at different cycle lengths (290 and 310ms respectively). The long interval after the last beat of the broad QRS complex tachycardia and the first beat of the narrow QRS complex tachycardia can also be seen, with VAV response and a fixed VA interval after the ventricular tachycardia (see text).
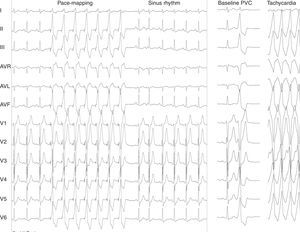
Based on these observations, radiofrequency catheter ablation of the slow pathway region was performed using a 4-mm non-irrigated bidirectional catheter (Biosense Webster, Diamond Bar, CA). Post-ablation programmed atrial and ventricular stimulation failed to induce any supraventricular tachycardia even under isoproterenol infusion. However, premature ventricular complexes (PVC) and a wide QRS complex tachycardia identical to the initial one were induced. Because the patient was extremely symptomatic, the decision was taken to ablate the ventricular focus. The twelve-lead ECG suggested a septal origin of the tachycardia in the right ventricular outflow tract (RVOT) with a predominant R and small S wave in I and tall S waves in V1/V2, with transition in the precordial leads (R/S≥1 by V4). Furthermore, the PVC precordial transition occurred later than the sinus rhythm transition, excluding a left ventricular outflow tract origin.1 The ablation catheter was then placed in the subpulmonary septal RVOT for mapping and ablation. The PVC and the VT could not be further induced, perhaps due to mechanical pressure (“bump termination”). As conventional local activation mapping was not possible, pace-mapping was performed from this stable septal RVOT, which revealed 12/12 lead concordance with the PVC/VT (Figure 3). Moreover, ablation at this point unleashed runs of PVC and non-sustained tachycardia with QRS morphology similar to that seen during spontaneous VT, which terminated during radio frequency application with 50W and 55°C. Thirty minutes after ablation, no tachycardia was induced either with or without isoproterenol and there was no recurrence during 12 months of follow-up.
DiscussionWe describe the fascinating electrophysiological interplay between a narrow and a wide QRS tachycardia. Interestingly, the two different tachycardias did not occur simply by coincidence, but showed a degree of mutual interdependence in inducing, resetting and terminating each other.
This association (RVOT VT/AVNRT) is a case of double tachycardia.2 It is reported to occur more often in patients with poor left ventricular function or in association with digoxin treatment,1,3 but it has also been described in patients without known structural heart disease4; in fact, Kautzner et al5 reported that 15% of patients with clinically documented idiopathic outflow tract VT were also found to have reproducibly inducible AVNRT at the time of the EPS. Additionally, it has also been postulated that concealed retrograde engagement of the AV node could occur, allowing the next anterograde impulse to depolarize the ventricle via the slow pathway and thus initiate tachycardia.6 Finally, RVOT tachycardia is a triggered arrhythmia, whose induction would be favored by the high catecholamine levels which can occur during AVNRT.7
From the electrophysiological point of view it is worth analyzing the response after the transient “entrainment” of the AVNRT by the non-sustained ventricular tachycardia. During the latter, the atrial cycle length accelerated to the VT cycle length and the narrow tachycardia resumed after the VT spontaneously stopped. We suggest that similar information to that obtained during the ventricular entrainment of SVT could also be inferred from spontaneous transient entrainment of an AVNRT by a VT [(VVT−VSVT)−TCL], to the best of our knowledge never previously described. This is in favor of an AVNRT rather than orthodromic tachycardia (AVRT) due to the long [(VVT−VSVT)−TCL] interval (140ms-160ms), similar to the PPI-TCL measurement, which is also supported by the absence of atrial advancement by the spontaneous occurring PVC when the His bundle was refractory. The VAV response also helps to rule out an atrial tachycardia. In this regard, during the VT runs and the subsequent SVT, the first VA after the narrow QRS tachycardia was always fixed, regardless of the different cycle lengths of the RVOT-VT, another clue that helps to rule out an atrial tachycardia (Figure 2D and E).
The fact that the syncope disappeared after ablation is interesting. As is known, syncope often has multiple contributory factors. In the present case, the high heart rate during orthostatism and a possible inadequacy of vascular compensation could have contributed to the syncope episodes. However, this is only supposition and the exact mechanism cannot be completely explained.
To summarize, in such situations, in which during tachycardia there is intermittent widening of the QRS, care should be taken to not classify it as a simple transient aberrancy. Subsequent analysis looking for clues pointing towards the presence of a double tachycardia should be taken into account.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestDr. Moisés Rodríguez-Mañero is funded by a post-residency grant on clinical electrophysiology from the European Society of Cardiology.