We present a 73-year-old man with severe aortic stenosis (area 0.6 cm2) and left ventricular dysfunction in New York Heart Association class III. He had a previous history of hypertension, peripheral vascular disease, chronic obstructive pulmonary disease and porcelain aorta. His logistic EuroSCORE was 20.01% and Society of Thoracic Surgeons score was 2.78%.
After careful evaluation by the heart team, the patient was referred for transcatheter aortic valve implantation (TAVI).
Femoral and left subclavian routes were not suitable for the procedure due to calcified and severe stenoses. Other routes were also rejected, the right subclavian artery due to aortic annulus angulation (>60°) and direct aortic access due to porcelain aorta (Figure 1). The minimum diameter of the left common carotid artery was 6.3 mm, so TAVI was scheduled. Cerebral magnetic resonance angiography was carried out to confirm the presence of collateral perfusion through the circle of Willis.
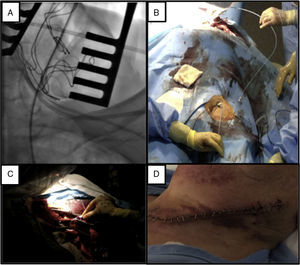
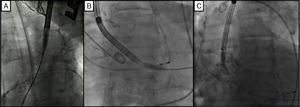
The procedure was performed in the catheterization laboratory, the team members being specially positioned for this approach (Figure 2). The proximal left common carotid artery was exposed under general anesthesia. Thereafter, sequential dilation of the carotid artery was performed and an 18F vascular access sheath was carefully advanced into the ascending aorta. The valve delivery system was then advanced and a 29 mm CoreValve Evolut R self-expanding prosthetic valve was successfully deployed. There was no residual gradient or significant aortic regurgitation (Figure 3, Video 1). The patient was discharged five days after the procedure without complications.
A transcarotid approach represents an alternative access route for TAVI in selected cases with no other suitable vascular approach.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.