Timely reperfusion with primary percutaneous coronary intervention (PPCI) in ST-segment elevation myocardial infarction (STEMI) improves patient outcomes. In recent years, the Stent for Life (SFL) initiative in Portugal developed an action plan to improve timely access to PPCI. This study aims to evaluate performance indicators in high-risk populations (elderly, female, and diabetic patients).
MethodsData on 1340 patients with suspected STEMI who were admitted to 18 Portuguese interventional cardiology centers were collected during a one-month period every year from 2011 to 2016. The risk of longer patient and system delay in elderly, female, and diabetic patients was assessed by logistic regression analysis.
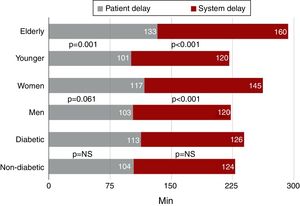
ResultsPatient and system delays were longer in elderly patients (incremental median 32 and 40 min; p=0.001 and p<0.001, respectively). Median system delay was also longer in women (incremental median 25 min; p<0.001). Consequently, times to revascularization were longer in elderly patients (incremental median 92 min; p<0.001) and women (incremental median 67 min; p<0.001). There was no significant difference in reperfusion delay in diabetic patients.
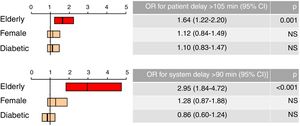
After adjustment for gender and diabetes, elderly age was an independent predictor of patient delay longer than the median (OR 1.64; 95% CI 1.22-2.20; p=0.001) and system delay >90 min (OR 2.95; 95% CI 1.84-4.72; p<0.001).
ConclusionElderly patients showed longer patient and system delays, regardless of gender and presence of diabetes. These data suggest that the elderly subgroup should be the target of a new action by the SFL initiative.
Nos últimos anos, a Iniciativa Stent for Life (SFL) em Portugal desenvolveu um plano de ação de forma a aumentar o acesso atempado à angioplastia primária (ICPP). Este trabalho pretende avaliar os indicadores de desempenho no enfarte agudo do miocárdio com supradesnivelamento de ST (EAMCSST), em populações de alto risco: idosos, mulheres e diabéticos.
MétodosDados de 1340 doentes com suspeita de EAMCSST, admitidos em 18 centros nacionais de cardiologia de intervenção, foram recolhidos durante um mês, em anos consecutivos (2011-2016). O risco de atraso do doente e do sistema em idosos, mulheres e diabéticos foi avaliado por análise de regressão logística.
ResultadosOs atrasos do doente e do sistema foram superiores nos idosos (mediana incremental de 32 e 40 min, p = 0,001 e p < 0,001, respetivamente). A mediana do atraso do sistema também foi superior nas mulheres (mediana incremental de 25 min, p < 0,001). Consequentemente, houve tempos mais longos até à revascularização nos idosos (mediana incremental de 92 min; p < 0,001) e mulheres (mediana incremental de 67 min; p < 0,001). Não houve diferença significativa no atraso de reperfusão nos diabéticos.
Após ajuste para género e diabetes, os idosos foram o preditor independente de «atraso do doente maior que a mediana» (OR 1,64; IC95% 1,22-2,20; p = 0,001) e «atraso do sistema > 90 min» (OR 2,95; IC95% 1,84-4,72; p < 0,001).
ConclusãoOs idosos apresentaram maior atraso do doente e do sistema, independentemente do género e da presença de diabetes mellitus. Esses dados sugerem que o subgrupo dos idosos deve ser alvo de uma nova ação da Iniciativa SFL.
Timely coronary reperfusion in patients diagnosed with ST-segment elevation myocardial infarction (STEMI) reduces the risk of mortality and development of heart failure.1–3 However, this therapy is still often administered late.4 Around ten years ago, Portugal had one of the lowest rates in Europe of primary percutaneous coronary intervention (PPCI),5,6 the reperfusion strategy recommended by the current European guidelines.7,8 Aiming to improve the number of PPCI procedures performed per year per million population and the quality of treatment, Portugal joined the European Stent for Life (SFL) initiative in 2011.9 Since then, various initiatives have been conducted to reduce time to reperfusion, targeting not only on door-to-balloon time, but also, and especially, patient delay and system delay. The literature reports longer time to reperfusion in some high-risk subgroups of patients, including elderly, female and diabetic patients.1 Western populations are aging rapidly,10 increasing the prevalence of STEMI in the elderly6 and in women11 referred for PPCI. In this study, we aim to analyze the risk of increased time to reperfusion in these high-risk subgroups and changes in performance indicators after Portugal joined the SFL initiative.
MethodsStudy design and data collectionThis observational study collected data during a national survey conducted by the SFL initiative in Portugal in 18 interventional cardiology centers with 24/7 PPCI in mainland Portugal. The survey included patients suspected of having STEMI referred for PPCI in each center. The survey was carried out during a one-month period in six consecutive years from May 9 to June 8, 2011, immediately after Portugal joined SFL (time zero, T0), and in the same period in 2012 (time one, T1), 2013 (time two, T2), 2014 (time three, T3), 2015 (time four, T4), and 2016 (time five, T5).
The following patients were excluded: those who received fibrinolytic therapy prior to PPCI; those whose onset of STEMI symptoms was in hospital; those admitted in the autonomous island regions of Madeira and the Azores; those with late presentation of STEMI (more than 12 hours between symptom onset and first medical contact [FMC]); and those diagnosed without electrocardiographic (ECG) criteria of STEMI. A total of 1340 patients suspected of having STEMI and referred for urgent PPCI were enrolled in the study, and three high-risk groups were defined: elderly patients (aged ≥75 years); women; and diabetic patients (those previously diagnosed as such). Demographic data were collected, including age and gender, presence of diabetes, and previous history of myocardial infarction (MI) or coronary revascularization. Information about how patients requested assistance after symptom onset was also collected: whether there was FMC with the emergency medical system (EMS) by calling the national emergency number (112), whether they attended a healthcare center or local hospital without PPCI capability, and what means of transport were used to go to a center with PPCI capability (by their own means, EMS, or inter-hospital transfer). The date and time of the following events were recorded: symptom onset; FMC; first ECG recording after FMC; arrival at a hospital with PPCI capability; and reperfusion.
Based on these data, various components of the delay in coronary reperfusion treatment were calculated: patient delay (time from symptom onset to FMC); FMC-ECG (time from FMC to the ECG recording that provided the STEMI diagnosis); system delay (time from FMC to coronary reperfusion, by balloon, wiring or mechanical thrombectomy; door-to-balloon time (time from the patient's arrival at a hospital with PPCI capability to reperfusion); and treatment delay (time from symptom onset to reperfusion).
In the high-risk groups under study, the percentage of patients presenting delays within the limits defined by the European guidelines7,8 was determined, since these are quality indicators of STEMI treatment: FMC-ECG ≤10 min; door-to-balloon time ≤60 min; system delay ≤90 min; and treatment delay ≤120 min. Off-hours FMC was defined as FMC with the EMS during the weekend or at night (between 8:00 pm and 8:00 am).
Interventions by the Stent for Life initiativeAfter Portugal joined the SFL initiative in February 2011, various campaigns were conducted targeting the general population (aiming to reduce patient delay) and the organization of prehospital and in-hospital emergency systems (aiming to reduce system delay). During the study period, SFL promoted a national public campaign called “Act now. Save a life!” to teach the population to recognize the symptoms of MI and to encourage patients to request assistance by dialing 112. This campaign was publicized by the media, particularly television, but also radio and newspapers, and ‘ambassadors’ were invited to participate in the initiative and to spread the message. Concerning the organization of the prehospital system, the priorities were to reorganize the network, to optimize the transmission of a prehospital ECG recording to the emergency cardiologist, and to promote inter-hospital transfer by the EMS from local centers without PPCI capability to PPCI-capable hospitals. Regarding the organization of in-hospital systems, the 24/7 PPCI network was widened with the opening a new catheterization laboratory at Hospital de Évora in 2012, to improve coverage for the Alentejo region. In addition, the STEMICARE program held several hospital training meetings targeting medical emergency teams to improve communication and coordination, to reduce the delay between the patient arriving at the hospital and entering the catheterization laboratory. The differences in patient delay and system delay before and after the SFL initiative in Portugal were assessed for the different risk groups.
Statistical analysisContinuous variables were presented as means ± standard deviation. The normality of data was assessed by the Kolmogorov-Smirnov test and equality of variances was assessed by the Levene test. The Student's t test was used to analyze variables, such as age, with normally distributed data or equality of variances. Categorical variables were presented as percentages and assessed by the chi-square test or Fisher's exact test.
Continuous variables with non-normally distributed data, such as patient delay and system delay, were presented as medians and interquartile range (IQR) and tested using the Mann-Whitney U test and the Kruskal-Wallis test for two or more independent samples, respectively.
The effect of each risk variable (age, gender and presence of diabetes) as a predictor of patient delay longer than the median and system delay >90 min was assessed by logistic regression analysis. The effect of these potential predictors was tested in a multivariate model, and the corresponding odds ratios (OR) and 95% confidence intervals (CI) were calculated. Goodness-of-fit was assessed by the Hosmer-Lemeshow test. Two-sided p values were calculated and p<0.05 was considered statistically significant. All statistical analyses were performed using IBM SPSS for Windows, version 21.
ResultsA total of 1340 patients suspected of having STEMI admitted to 18 centers with PPCI capability were enrolled in the study. The mean age of the population was 62±13 years. Median (IQR) patient delay was 105 (55-203) min and median (IQR) system delay was 125 (90-192) min; 58.1% of these patients presented system delay >90 min.
Over the course of the five-year study period, the analysis included a total of 263 patients aged ≥75 years (19.6%), 309 women (23.1%) and 281 patients with diabetes (21.0%).
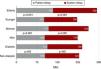
Elderly patientsElderly patients were mostly female and diabetic (Table 1). There was no difference from younger patients (age <75 years) regarding the way they requested assistance (Figure 1). Forty per cent of elderly patients called 112, and only 22.9% were thereafter transferred to a hospital with PPCI capability by a prehospital EMS vehicle (vs. 25.1% of younger patients; p=NS). Twenty elderly patients (7.8%) attended a healthcare center before FMC (vs. 8.6% of younger patients; p=NS), and 46.4% (vs. 46.7% of younger patients; p=NS) attended a healthcare center or hospital without PPCI capability and needed transport to a PPCI-capable hospital. Although the percentage of patients with symptom onset at night (8:00 pm-8:00 am) was similar for both groups, elderly individuals less frequently presented FMC at night (32.8% vs. 39.3%; p=0.067).
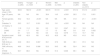
Differences in baseline clinical characteristics within each high-risk group (elderly, female and diabetic patients).
| Elderly (n=263) | Younger (n=1047) | p | Women (n=309) | Men (n=1003) | p | Diabetic (n=281) | Non-diabetic (n=1017) | p | |
|---|---|---|---|---|---|---|---|---|---|
| Age, years (mean ± SD) | 82±5 | 58±10 | <0.001 | 68±15 | 61±13 | <0.001 | 67±12 | 61±13 | <0.001 |
| Age ≥75 years, % | NA | NA | NA | 38.4 | 14.5 | <0.001 | 26.5 | 17.6 | 0.001 |
| Female gender, % | 45.2 | 18.3 | <0.001 | NA | NA | NA | 31.8 | 21.1 | <0.001 |
| Diabetes, % | 29.3 | 19.7 | 0.001 | 29.2 | 19.1 | <0.001 | NA | NA | NA |
| CV history, % | |||||||||
| PCI | 11.8 | 11.2 | NS | 8.0 | 12.1 | 0.047 | 10.1 | 10.9 | NS |
| CABG | 0.4 | 1.7 | NS | 1.7 | 1.3 | NS | 3.6 | 0.8 | 0.002 |
| MI | 9.1 | 12.0 | NS | 8.4 | 12.2 | 0.076 | 11.5 | 10.7 | NS |
| Symptom onset 8:00 pm-8:00 am, % | 39.8 | 42.9 | NS | 40.3 | 42.9 | NS | 43.8 | 41.8 | NS |
| FMC 8:00 pm-8:00 am, % | 32.8 | 39.3 | 0.067 | 39.1 | 37.9 | NS | 39.1 | 37.3 | NS |
| FMC off-hours, % | 48.6 | 54.8 | 0.086 | 52.0 | 54.5 | NS | 52.4 | 54.0 | NS |
| STEMI diagnosis, % | 90.7 | 88.0 | NS | 85.9 | 91.3 | 0.006 | 89.1 | 90.4 | NS |
CABG: coronary artery bypass grafting; CV: cardiovascular; FMC: first medical contact; PCI: percutaneous coronary intervention; MI: myocardial infarction; NA: not applicable; NS: not significant; SD: standard deviation; STEMI: ST-elevation myocardial infarction.
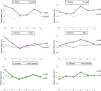
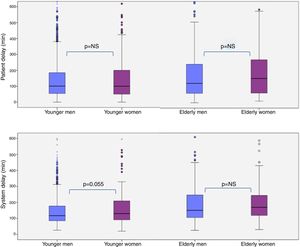
Median (IQR) patient delay in elderly patients was 133 (60-255) min and median (IQR) system delay was 160 (109-246) min. Both patient and system delays were longer in elderly than in younger patients (incremental median 32 min; p=0.001 for patient delay; incremental median 40 min; p=0.001 for system delay) (Figure 2). This is in line with the greater delay before reperfusion treatment in elderly patients (incremental median 92 min; p<0.001).
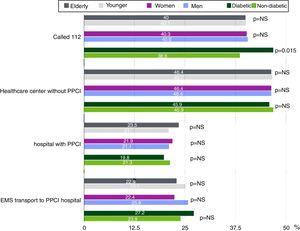
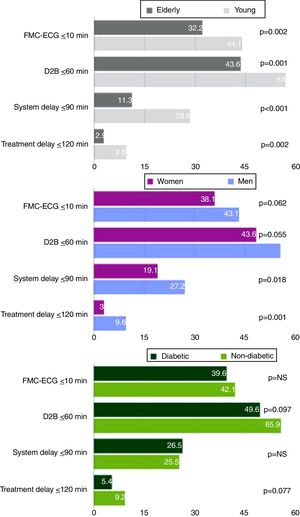
As a result, elderly patients were less compliant with the times recommended by the European guidelines7,8: only 32.2% of these patients presented FMC-ECG ≤10 min, 43.6% presented door-to-balloon time ≤60 min, 11.3% presented system delay ≤90 min, and 2.9% presented treatment delay ≤120 min (Figure 3).
Univariate analysis revealed that elderly patients presented a 1.6-fold higher risk of presenting patient delay longer than the median and a 3.1-fold higher risk of presenting system delay >90 min. Multivariate analysis after adjustment of the variable ‘age’ for gender and presence of diabetes showed that age was an independent predictor of patient delay longer than the median (OR 1.64; 95% CI 1.22-2.20; p=0.001) and of system delay >90 min (OR 2.95; 95% CI 1.84-4.72; p<0.001) (Figure 4).
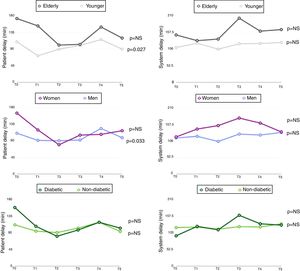
Over all the periods assessed, patient delay tended to decrease, from T0 (173 min, IQR 60-294) to T5 (120 min, IQR 35-241), although without statistical significance (Figure 5). On the other hand, system delay was approximately constant during the study (Figure 5).
WomenIn this study, the mean age of women with STEMI was approximately seven years older than men, and 38.4% of women were aged ≥75 years (vs. 14.5% of elderly men; p<0.001).
Compared to men, women presented a higher prevalence of diabetes (29.2% vs. 19.1%; p<0.001) and a lower prevalence of previous PCI (8.0% vs. 12.1%; p=0.047) (Table 1).
Moreover, a definitive STEMI diagnosis was less frequent in women (85.9% vs. 91.3%; p=0.006), 5.9% presented no significant coronary artery lesions, 4.6% presented stress cardiomyopathy (Takotsubo syndrome), 0.7% presented myopericarditis, 0.7% presented non-ST-elevation MI, 0.7% did not undergo coronary angiography, and 1.7% had another diagnosis. Differences were observed in the diagnosis of Takotsubo syndrome, which was more frequent in women than in men (4.6% vs. 0.5%; p<0.001).
System delay was longer in women (incremental median 25 min; p<0.001) (Figure 2), which was reflected in a higher percentage of women with system delay >90 min (80.9% vs. 72.8%; p=0.018) (Figure 3). There was also a trend for longer patient delay in women than in men (incremental median 14 min; p=0.061). Treatment delay was also longer in women than in men (incremental median 67 min; p<0.001).
Univariate analysis showed that the variable ́women‘was not a predictor of patient delay longer than the median (OR 1.27; 95% CI 0.97-1.67; p=0.081), but it did predict system delay >90 min (OR 1.58;95% CI 1.09-2.29; p=0.015). However, after adjustment for age and presence of diabetes, the variable ́women‘did not predict system delay >90 min (OR=1.28; 95% CI 0.87-1.88; p=0.218) (Figure 4).
When the analysis of reperfusion times was stratified according to age, no significant differences were found in median patient delay in women compared to men, for both age subgroups (Figure 6). Younger women (aged <75 years) tended to have a longer system delay than younger men (median 130 min, IQR 90-209, vs. median 117 min, IQR 85-178; p=0.055).
Analysis of patient and system delays before and after Portugal joined the SFL initiative revealed a tendency toward shorter patient delays in women, though without statistical significance (reduction of 48 min from T0 to T5; p=NS). System delay showed no significant variations over all the periods assessed (Figure 5).
DiabetesThere was a higher proportion of elderly patients and women in the subgroup of diabetic patients, who also showed a higher prevalence of previous coronary artery bypass grafting (CABG) than non-diabetic patients (3.6% vs. 0.8%; p=0.002), although there were no differences in the prevalence of previous MI or PPCI (Table 1).
Diabetic patients more often requested assistance after symptom onset by calling 112 than non-diabetic patients (46.9% vs. 38.6%; p=0.015). Despite this difference, the percentage of patients transferred to a hospital with PPCI capability by EMS was not significantly higher in diabetic patients (27.2% vs. 23.9%; p=NS) (Figure 1).
No differences were observed in patient or system delay between diabetic and non-diabetic patients (Figure 2). However, there was a trend toward longer treatment delay in diabetic patients (incremental median 39 min; p=0.063). The presence of diabetes did not increase the risk of patient delay longer than the median (OR 1.13, 95% CI 0.86-1.49; p=0.391) or of system delay >90 min (OR 0.95, 95% CI 0.67-1.34; p=0.772).
DiscussionIn our analysis, as in De Luca's study,1 older age, female gender and presence of diabetes were associated with longer reperfusion treatment delay in STEMI patients. However, it was observed that elderly age was the greatest contributor to this delay, and is an independent predictor from gender and presence of diabetes for longer patient and system delays.
Elderly patientsWestern populations are aging rapidly and the number of elderly patients with STEMI referred for PPCI is increasing.5,10 At the same time, revascularization tends to be performed later in older than in younger patients,12–14 which is partially related to delays in requesting assistance after symptom onset.15,16 This delay may be explained by the difficulty that the elderly have in recognizing the symptoms of MI.17,18 Furthermore, like women and diabetic patients, older patients often have atypical MI symptoms, without chest pain.19 Previous studies showed that patients presenting typical chest pain and sudoresis take less time to FMC, as they are aware that cardiovascular symptoms require immediate treatment,20 whereas elderly patients presenting atypical symptoms, with epigastric or dorsal pain, or painless MI, tend to request assistance later. Our study showed that elderly patients requested assistance less often during the night. The literature shows that FMC during the day is associated with late MI, as many patients requesting assistance during the day presented the first symptoms during the previous night.21 This may be related to the social isolation of older patients, who often live alone and tend to wait for the next day to request assistance, which is usually done by their relatives.
Treatment delay in the elderly is due not only to patient-related factors, but also to system-related factors. System delay in this risk subgroup was significantly greater than in younger patients in our study, which may be related to the fact that less than one third of elderly patients underwent ECG recording within 10 min of FMC, and to the difficulty of assessing and interpreting MI symptoms in elderly patients with multiple comorbidities. Thus, this study highlights the need to educate the general population, and particularly the elderly, on how to recognize the symptoms of MI and to request assistance as soon as possible, even if symptom onset occurs at night. National campaigns explaining the importance of rapid attendance at a hospital with PPCI capability after symptom onset, preferably by calling 112, are also important. Over the five-year study period, the SFL initiative implemented such campaigns in Portugal and, though there were no changes in system delay, patient delay tended to decrease during this period, particularly in elderly and female patients. There is also a need to improve procedures in the healthcare system to reduce system delay in elderly patients, which may include an ECG recording during medical triage, even in patients who do not present typical MI symptoms. Nevertheless, system delay cannot be explained simply by late ECG recording leading to a late diagnosis. Approximately 32% of elderly patients underwent an ECG within 10 min of FMC, as recommended, and only 11% of these patients presented a system delay ≤90 min, suggesting that system delay can be partially explained by late patient transfer to a PPCI-capable unit, mainly when inter-hospital transfer is needed. Less often, technical difficulties during PPCI may contribute to reperfusion delay.
WomenConcerning reperfusion delay in women, previous studies have presented contradictory results, with several studies reporting that women present longer patient delay than men,22,23 while others showed no differences between genders in prehospital delay.24–26 This disparity may result from methodological differences between studies. Our study demonstrated that there is a tendency for longer patient delay in women, though without statistical significance, which may result from the small sample size of this study.
Reasons for longer patient delay in women include first MI at older age, effects of chronic diseases that may be confused with the symptoms of MI, higher prevalence of atypical MI symptoms, and misperception of chest pain severity by women, who are less often aware of the cardiac origin of these symptoms.27
There is still an erroneous belief that the most frequent causes of death in women are breast and gynecological malignancies,28 so there is a need for educational campaigns emphasizing that cardiovascular disease, especially MI, is the leading cause of death in women.29
In this study, similarly to others,30–32 system delay was longer in women than in men, suggesting negative discrimination by the healthcare system. The percentage of women who underwent ECG recording within 10 min of FMC was lower (36% in women vs. 43% in men). Although these differences had no statistical significance, they also indicate that suspicion of MI by the physician tends to differ between women and men.32 The later MI diagnosis can be partially explained by the higher prevalence of atypical MI symptoms in women.33 It may also be related to their higher prevalence of acute coronary syndrome without obstructive coronary disease (15% in women vs. 8% in men).34 As reported in the literature,35–37 coronary arteries without significant obstructive lesions are more often observed in women, as is Takotsubo syndrome (4.6% in women vs. 0.5% in men). According to a recent review article, 6% of cases of MI are with non-obstructive coronary arteries, and 40% of these cases occur in women. The clinical presentation of these cases is similar to MI with obstructive coronary lesions.38 Takotsubo syndrome is also more frequent in postmenopausal women and is often preceded by physical or emotional stress. The clinical presentation of this syndrome is similar to acute coronary syndrome, but angiographically patients do not present coronary artery lesions with significant obstruction.39
Similarly to elderly patients, the longer system delay observed in women cannot be explained simply by delays in obtaining an ECG recording, but is also due in part to difficulties in transferring patients to a PPCI-capable center and to technical problems during the procedure. However, as this is an observational study, it is not possible to confirm the specific causes of the longer system delay in women. After adjustment for age and diabetes, the variable ‘women’ was not significantly associated with longer system delay. This finding suggests that, in general, the healthcare system does not discriminate against women with MI, which is not in agreement with previously published data.30,32 However, when the sample was subdivided by age, it was confirmed that younger women (aged <75 years) presented longer system delay, suggesting that the healthcare system may discriminate against younger women. This may be explained by the lower incidence of MI in women of this age group, due to the protective effect of estrogens in premenopausal women.40 This longer system delay may be a modifiable factor that leads to higher in-hospital mortality in younger women with MI.41 In fact, system delay is the stage at which the healthcare system can act directly in order to reduce reperfusion delay. In recent years, system delay in women has remained steady, indicating that further measures are required to improve pre- and in-hospital organization.
DiabetesUnlike other studies,1,21,23,26,42 our analysis showed no differences in the patient delay of diabetic patients. It is known that diabetic patients frequently have altered perception of pain in MI, explained by diabetic neuropathy,43 and symptoms associated with diabetes, such as sudoresis and dizziness in hypoglycemic episodes, may confuse or mask the symptoms of MI.44,45 Nevertheless, a study with a large patient population showed that symptom characteristics (typical vs. atypical) do not explain the longer patient delay in diabetic patients reported in previous studies.26 In our study, diabetic patients called the emergency number more frequently and presented a higher prevalence of previous CABG, which may had contributed to the lack of difference in patient delay. Other studies also reported no differences in patient delay in diabetic patients, though to a lesser extent.46,47
Concerning system delay, similarly to previous studies42 in which the presence of diabetes was associated with longer door-to-balloon time, this study revealed a tendency for a lower percentage of diabetic patients to have door-to-balloon time ≤60 min, as recommended by the European guidelines,7,8 though without statistical significance.
As stated above, a significantly higher percentage of diabetic patients requested assistance by calling 112. However, this did not affect the percentage of diabetic patients transported by the EMS to a hospital with PPCI capability, which may be related to a higher probability of prehospital system error in medical triage of diabetic patients with STEMI, possibly due to difficulties in interpreting symptoms.
In all three defined high-risk groups (elderly, female and diabetic patients), there was a trend towards a reduction in patient delay over the first years of the SFL initiative in Portugal, between 2011 and 2016 (as inferred from the yearly study periods), but system delay remained constant. These results should be taken into consideration in the future strategy of SFL in Portugal, particularly concerning the strengthening of current educational programs and the implementation of strategies to optimize prehospital and in-hospital organization, aiming to improve system delay in these high-risk groups.
LimitationsData for this study were collected during a one-month period every year, so the impact of seasonal factors on the results is not considered. Moreover, sociodemographic characteristics such as race, socioeconomic status and education level that could affect patient delay were not recorded in this study. The presence of diabetes may have been underdiagnosed, considering that some patients reported as non-diabetic may have been diagnosed as diabetic during hospital stay after reperfusion. Also, the characteristics of symptoms were not assessed.
ConclusionElderly patients with STEMI presented longer patient and system delays before reperfusion treatment, independently of gender and presence of diabetes. These findings suggest that the elderly subgroup should be the preferential target for new educational campaigns developed by the SFL initiative in Portugal. These campaigns should aim to educate the older population and their caregivers to reduce patient delay, and to optimize prehospital and in-hospital triage in order to reduce system delay in this high-risk subgroup.
FundingThe authors state that they have no funding to declare.
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors gratefully acknowledge all the national centers that participated in the Stent for Life Initiative Portugal, with the support of the Portuguese Association of Interventional Cardiology (APIC), between 2011 and 2016: Hospital Vila Real (Henrique Cyrne Carvalho, MD; Paulino Sousa, MD); Hospital Braga (João Costa, MD); Hospital S. João (João Carlos Silva, MD); Hospital Santo António (Henrique Cyrne Carvalho, MD); Centro Hospitalar Vila Nova de Gaia (Vasco Gama Fernandes, MD); Hospital de Viseu (João Pipa, MD); Centro Hospitalar de Coimbra (Marco Costa, MD; Vítor Matos, MD); Hospital de Leiria (João Morais, MD); Hospital Fernando da Fonseca (Pedro Farto e Abreu, MD); Hospital de Santa Maria (Pedro Canas da Silva, MD); Hospital Santa Cruz (Manuel Almeida, MD); Hospital de Santa Marta (Rui Ferreira, MD); Hospital Curry Cabral (Luís Mourão, MD); Hospital Pulido Valente (Pedro Cardoso, MD); Hospital Garcia de Orta (Hélder Pereira, MD); Hospital Setúbal (Ricardo Santos, MD); Hospital de Évora (Lino Patrício, MD; Renato Fernandes, MD); Hospital de Faro (Victor Brandão, MD).