Stress-induced cardiomyopathy, also known as ‘broken heart syndrome’ or Takotsubo cardiomyopathy, is characterized by transient systolic dysfunction of the apical and/or mid segments of the left ventricle, in the absence of significant coronary artery disease. We report the case of a 56-year-old male patient with chronic obstructive pulmonary disease (COPD), with stress-induced cardiomyopathy associated with the use of ipratropium bromide, administered in the context of an acute exacerbation of COPD.
A cardiomiopatia associada ao stress, também conhecida por cardiomiopatia de Takotsubo, é caracterizada por uma disfunção sistólica transitória dos segmentos apicais e/ou médios do ventrículo esquerdo, na ausência de doença coronária significativa. Apresentamos um caso clínico de um doente do sexo masculino, com 56 anos de idade, com doença pulmonar obstrutiva crónica (DPOC), com cardiomiopatia associada ao stress que surgiu após uso de brometo de ipratrópio, administrado no contexto de uma exacerbação de DPOC.
Stress-induced cardiomyopathy, also known as ‘broken heart syndrome’ or Takotsubo cardiomyopathy (TC), is characterized by transient systolic dysfunction of the apical and/or mid segments of the left ventricle that mimics myocardial infarction, in the absence of significant obstructive coronary artery disease.1 There is often a history of recent emotional or physical stress or severe acute illness. Stress cardiomyopathy has been described in patients with chronic obstructive pulmonary disease (COPD).2–7
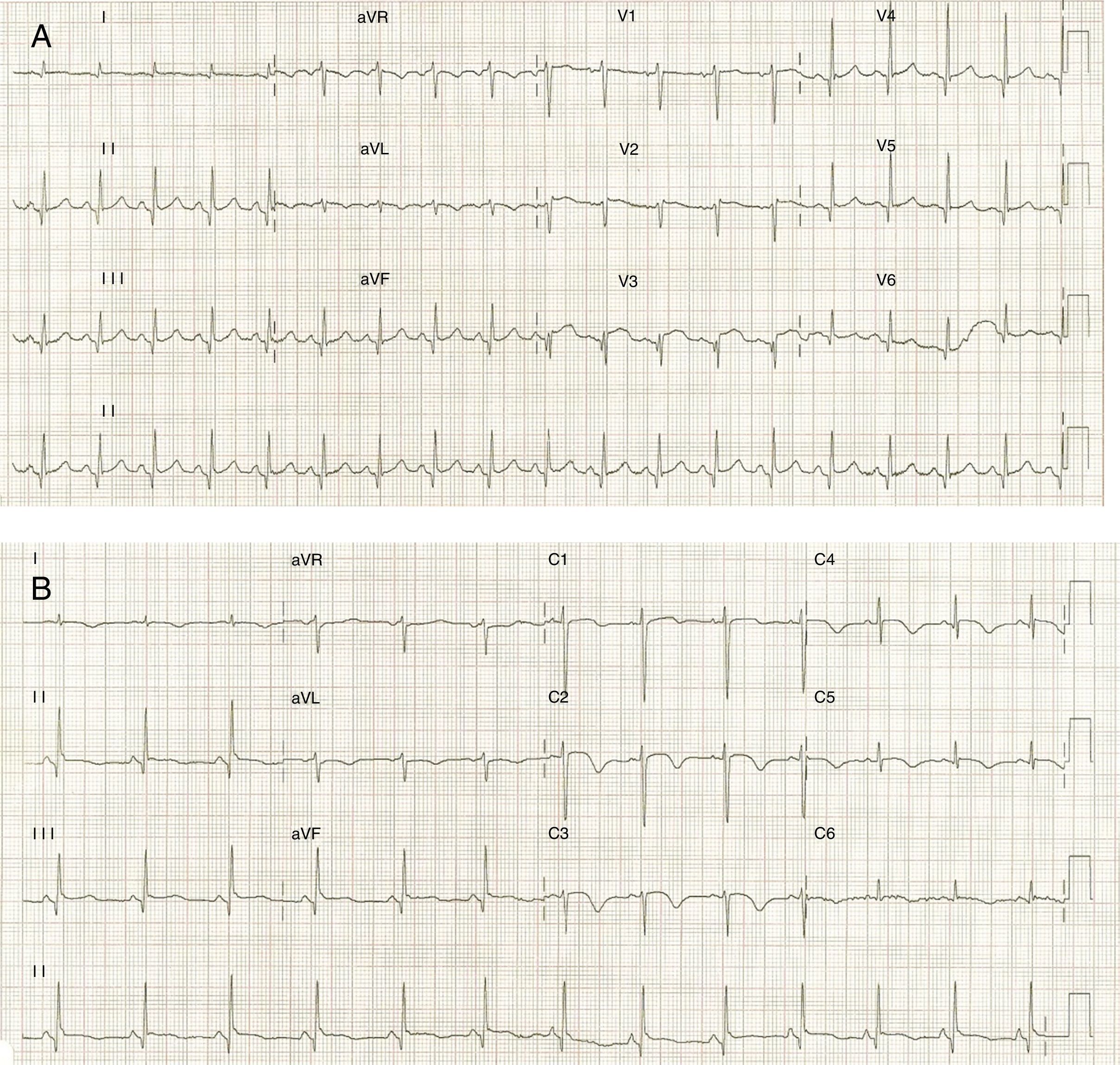
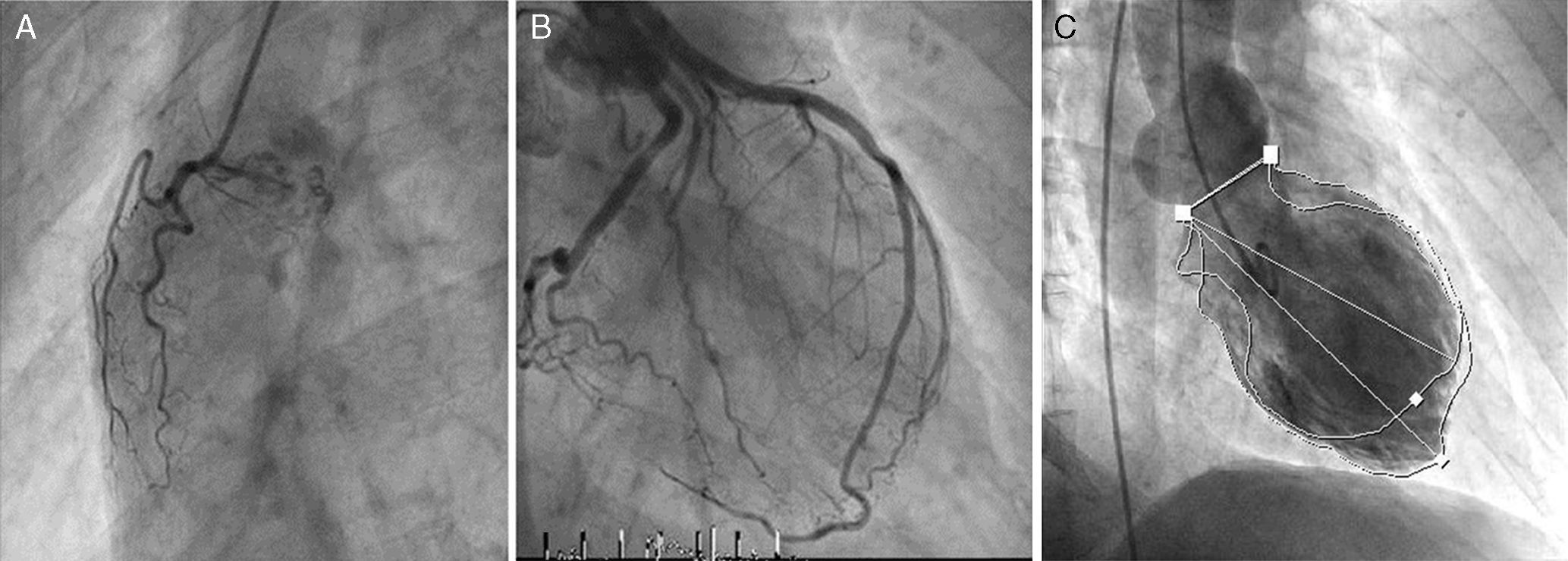
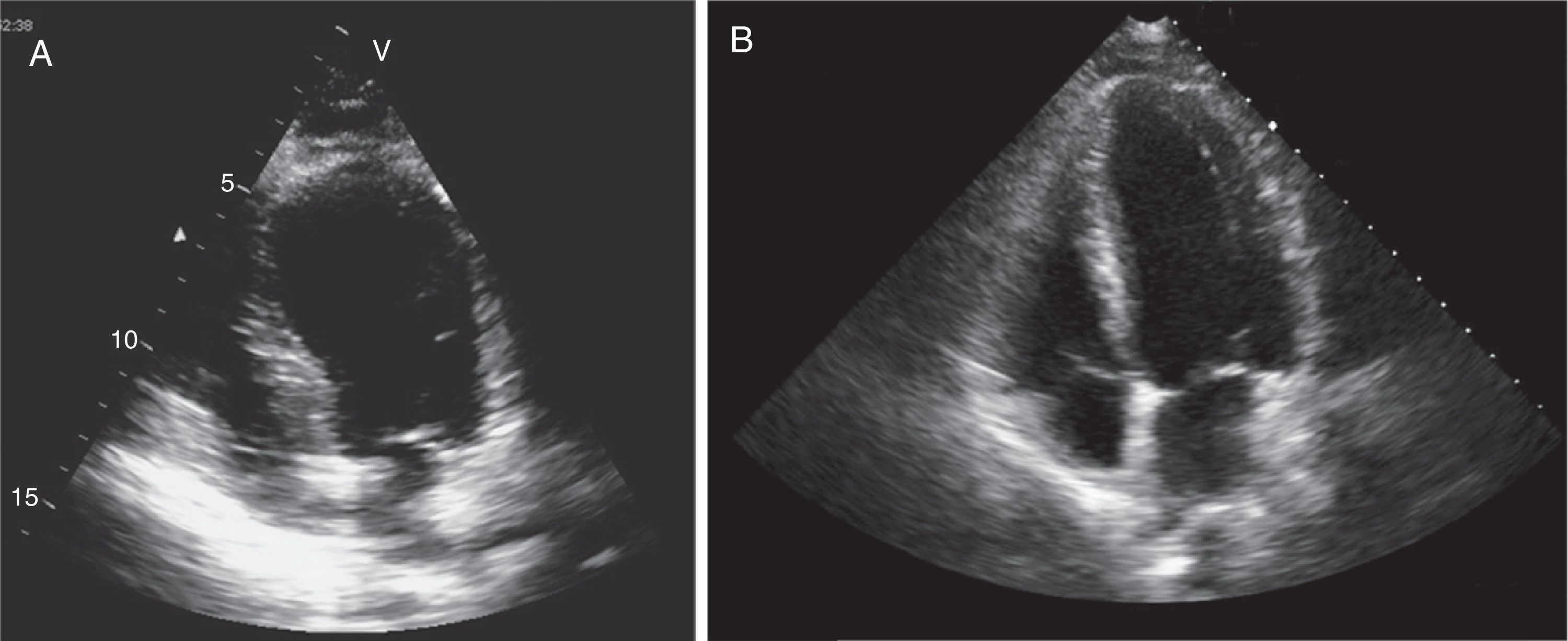
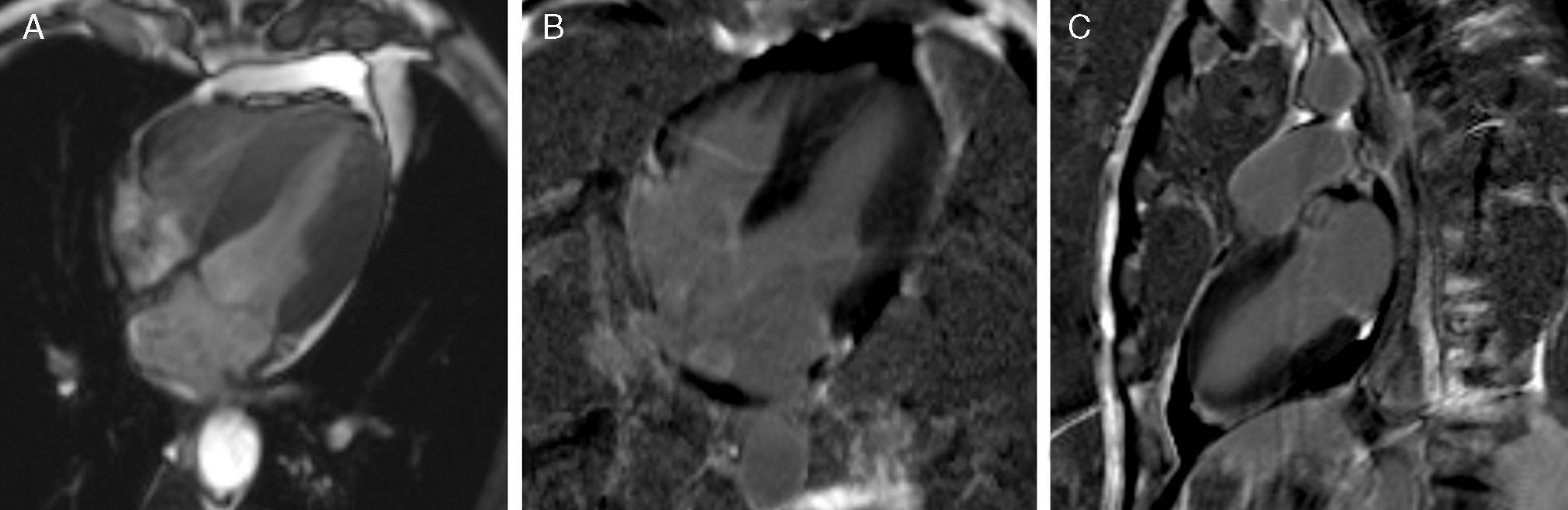
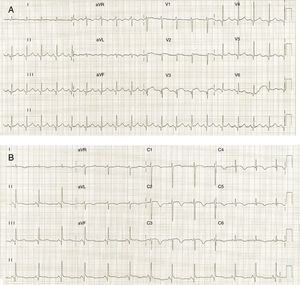
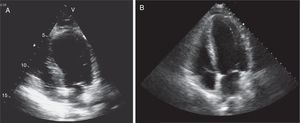
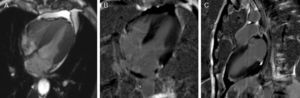
Case reportA 56-year-old Caucasian patient with COPD (irregularly treated with tiotropium bromide, acetylcysteine and mometasone) was admitted to the emergency room (ER) of our hospital with dyspnea and cough with sputum for two weeks. On admission to the ER, the patient was hemodynamically stable (systolic/diastolic blood pressure: 126/65 mmHg; heart rate: 98 bpm), eupneic at rest and with fever (39.1°C). Pulmonary auscultation revealed rumbles in the left hemithorax. The chest radiograph showed left paratracheal consolidation. There was no evidence of respiratory failure on arterial blood gas analysis. Laboratory tests revealed elevated leukocytes. After treatment with inhaled ipratropium bromide, the patient suffered severe bronchospasm and retrosternal chest pain accompanied by sweating and pallor. An electrocardiogram (Figure 1A), with pain, showed sinus tachycardia (heart rate 110 bpm), incomplete right bundle branch block, 2-mm ST-segment elevation in leads V1–V3 and Q waves in leads V3–V6. Given the possibility of an acute coronary syndrome, emergency coronary angiography was carried out, which showed normal coronary arteries (Figure 2A and B), severe systolic dysfunction with mid-apical akinesia and basal hypercontraction (Figure 2C). The echocardiogram confirmed severe compromise of left ventricular systolic function (LVSF), with akinesia of the mid-apical segments and an aneurysm-like dilatation (Figure 3). During hospitalization the patient remained hemodynamically and electrically stable, but the electrocardiographic pattern evolved with T-wave inversion in the left anterior precordial leads (Figure 1B) and plasma troponin I was elevated (peak value 2.28 ng/ml). After further use of ipratropium bromide, on the second day of hospitalization, the patient developed a new episode of marked bronchospasm and respiratory acidosis (pH 7.29; pCO2 53 mmol/l). He was started on non-invasive ventilation and was treated with hydrocortisone, inhaled salbutamol and furosemide, with progressive clinical improvement. He was also started on antibiotics (azithromycin plus ceftriaxone), but microbiological screening (bacteriological study of sputum and search for urinary antigens of Streptococcus pneumoniae and Legionella pneumophila) was negative. There was no significant increase in C-reactive protein levels. Repeat chest radiograph documented pulmonary overinflation. To assess the severity of lung disease, respiratory function tests were performed, which revealed a severe obstructive ventilatory syndrome with lung hyperinflation. The patient underwent a chest computed tomography scan on the fifth day after admission that showed scattered bronchiectasis and a ground-glass pattern in the area of the left lower lobe bronchus. The setting was interpreted as an infection in the process of resolution. Echocardiographic reassessment (Figure 3B) on the sixth day of hospitalization showed recovery of LVSF, with no segmental wall motion abnormalities, which was confirmed by cardiac magnetic resonance imaging (LVEF 57%) with no areas of delayed enhancement (Figure 4). The patient was discharged seven days after admission, treated with lisinopril 2.5 mg/day and inhaled salmeterol/fluticasone propionate. At six months of follow-up, no events had been registered.
Transthoracic echocardiogram in 4-chamber apical view (systolic frames) on admission revealing akinesia of the mid-apical segments and aneurysmatic dilatation (A) and echocardiographic reassessment (B), on the sixth day of hospitalization, showing recovery of left ventricular systolic function, with no segmental wall motion abnormalities.
Cardiac magnetic resonance imaging. Cine true fast imaging with steady-state free precession in 4-chamber at end-systole (A) shows normal contractility of the left ventricular apex with complete resolution of apical ballooning; 4-chamber (B) and 2-chamber (C) delayed post-contrast imaging shows no abnormal myocardial enhancement.
TC was first described in Japan in 1991.1 According to Gianni et al., TC represents up to 2% of all cases presenting as suspected ST-segment elevation infarction.8 Various mechanisms have been proposed for its pathogenesis, including coronary artery spasm, abnormal perfusion of cardiac microcirculation and sympathetic hyperactivity. Most patients have suffered physical or emotional stress that acts as a trigger. The diagnostic criteria for TC presented by Kawai et al. in 2007 include definitions and exclusion criteria, as well as a series of references for diagnosis.9 The present case is in complete accordance with the criteria of Kawai et al.9
Ipratropium bromide is an anticholinergic drug with bronchodilator properties used in the treatment of COPD. It is a quaternary ammonium congener of atropine and is poorly absorbed when given by inhalation.10 A serious but rare idiosyncratic reaction is paradoxical bronchospasm, the mechanism of which is unknown.10
White and Stewart described two cases of stress cardiomyopathy in patients with COPD exacerbations.3 In one of these cases, salbutamol was self-administered in a large dose.3 According to these authors, anticholinergic therapy may increase heart rate and sympathetic relative to parasympathetic activity. This mechanism could be at play in the case reported here.
In the present case, either possible emotional stress experienced by the patient or paradoxical bronchospasm associated with inhalation of ipratropium bromide could have led to the clinical picture of TC. Moreover, the time-course of the association between the administration of ipratropium bromide and TC is suggestive of a causal role, and this view is strengthened by the second episode of bronchospasm. However, it is not certain that paradoxical bronchospasm is due to ipratropium itself. The present case adds to the evidence on possible cardiovascular effects associated with the use of anticholinergic drugs in COPD patients.11,12
In conclusion, in the setting of acute COPD exacerbation, careful attention to the patient's cardiac status may be important, including in some cases (particularly in patients with chest pain or worsening clinical condition) the electrocardiogram, measurement of cardiac biomarkers, and, if there is suspicion of TC, further imaging studies, since this diagnosis may lead to changes in therapy.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.