A 50-year-old woman with a history of deep venous thrombosis presented to our clinic for evaluation of pulmonary hypertension. On examination, she had a strong pulmonary component of the second heart sound and a grade 2/6 systolic murmur on the left sternal border. Echocardiography revealed severe right ventricular dilatation, with mildly depressed function and severe tricuspid regurgitation. Estimated pulmonary artery systolic pressure was 52mmHg. Contrast-enhanced chest computed tomography suggested the presence of thrombi in the pulmonary vasculature.
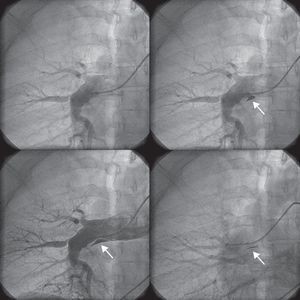
Right heart catheterization through the right femoral vein was then performed to confirm the clinical suspicion of chronic thromboembolic pulmonary hypertension and to assess operability. Access to the proximal segment of the right pulmonary artery was obtained using a 5-French NIH catheter. A 40-ml bolus of contrast material was then injected into the right pulmonary artery at a rate of 15ml/s (Supplementary Video 1). A small amount of subintimal opacification was seen after clearance of the contrast, a finding suggestive of iatrogenic pulmonary artery dissection (Fig. 1). This complication is thought to be due to fluctuations in the catheter tip due to respiration, causing high-pressure injection of contrast against a weakened pulmonary vessel wall. The patient remained completely asymptomatic and hemodynamically stable. No therapeutic measures were taken. Contrast-enhanced chest computed tomography performed the next day showed no evidence of pulmonary dissection. The patient is now on the waiting list for pulmonary endarterectomy.
The authors have no conflicts of interest to declare.