To describe the progression of aerobic exercise intensity in patients on a cardiac rehabilitation (CR) program.
MethodsWe conducted a retrospective analysis of a random sample of patients referred for CR after acute coronary syndrome between 2008 and 2016. The weekly peak exercise intensity achieved during aerobic exercise was estimated by treadmill speed and grade at peak effort and the corresponding perception of effort was assessed using the Borg scale. Initial exercise intensity was prescribed as 60-80% of reserve heart rate plus resting heart rate, and was modified according to perceived exertion. Peak heart rate/intensity and perceived exertion index were used as variables to characterize the response to the intensity achieved. Variables were compared at different time points: T1 (1st week), T2 (4th week) and T3 (8th week).
ResultsOf the total of 868, 238 patients were randomly selected. At peak heart rate during the session, exercise intensity (in metabolic equivalents) was: T1: 7.2±2.0, T2: 9.0±2.2, and T3: 9.4±2.2 (p<0.01). The peak heart rate/intensity index was T1: 16.8±5.4, T2: 13.4±3.6 and T3: 13.1±3.8 (p<0.01) and the perceived exertion index was T1: 1.8±0.6; T2: 1.4±0.5; T3: 1.4±0.5 (p<0.01).
ConclusionsIncreasing exercise intensity during CR, associated with lower perception of effort and lower heart rate necessary to achieve such intensity, leads to significant improvement in functional capacity.
Descrever a progressão da intensidade do exercício físico aeróbio em doentes submetidos a um programa de reabilitação cardíaca.
Material e métodosRealizamos uma análise retrospetiva numa amostra aleatória de doentes referenciados para um programa de reabilitação cardíaca na sequência de um evento coronário, entre 2008 e 2016. Estimamos a intensidade máxima do exercício, atingida semanalmente, pela velocidade e inclinação do tapete no pico do esforço na fase de esforço máximo, registando-se também o valor na escala de Borg correspondente. A prescrição inicial da intensidade de exercício foi feita com base na fórmula 60 a 80% da frequência cardíaca de reserva mais a frequência cardíaca de repouso e a progressão respeitou a perceção de esforço. Definimos as variáveis frequência cardíaca pico/intensidade e índice perceção de esforço para melhor indexar as respostas à intensidade atingida. Comparamos as variáveis em três momentos: T1 – 1.ª semana, T2 – 4.ª semana e T3 – 8.ª semana.
ResultadosSelecionamos aleatoriamente 238 dos 868 doentes referenciados para o programa de reabilitação cardíaca. No pico de esforço, a intensidade do exercício atingida (METS) melhorou (T1: 7,2±2,0 versus T2: 9,0±2,2 versus T3: 9,4±2,2; p<0,01). A relação frequência cardíaca pico/intensidade diminuiu (T1: 16,8±5,4 versus T2: 13,4±3,6 versus T3: 13,1±3,8; bpm/MET; p<0,01). O índice de perceção de esforço também diminuiu (T1: 1,8±0,6 versus T2: 1,4±0,5 versus T3: 1,4±0,5; p<0,01).
ConclusõesO aumento na intensidade do exercício ao longo do programa de reabilitação cardíaca, associado à diminuição da perceção de esforço e da frequência cardíaca necessária para o atingir, traduz uma melhoria significativa na capacidade funcional.
The advent of cardiac rehabilitation (CR) has helped reduce the risk of cardiovascular mortality and improved health-related quality of life in coronary patients.1
There is strong evidence that moderate- to high-intensity exercise in cardiac patients is safe and should be delivered in a moderate-intensity long-duration exercise scheme.2
However, exercise intensity prescription remains a major issue in CR, as it affects both improvement in exercise capacity and the risk of adverse events during treatment.3
Current guidelines for CR strongly recommend exercise testing (ET) as a key component of the initial patient assessment and as a tool for exercise prescription.4 When this is not available, alternative standardized approaches to prescribing exercise intensity (e.g. resting heart rate [HR] plus 20-30 bpm) may be used but, since they do not consider individual chronotropic response to exercise, benefits of exercise may be limited.4
Cardiopulmonary testing is the gold standard for functional evaluation, but cost, resource and time constraints hinder widespread use. Therefore, indirect methods of estimating intensity, such as percentage of maximal HR (MHR), percentage of HR reserve (HRR), or subjective rating of effort (using Borg scales), are commonly used in most CR programs.4
Indirect methods based on HR assume a linear relationship between HR and both oxygen uptake (VO2) and increase in work rate during incremental exercise.5 Most commonly used indirect methods include percentage of HRR and percentage of MHR. HRR is defined as the difference between baseline and peak HR values. A target HR of 40-80% of HRR plus resting HR has been proposed for cardiac patients.6 Alternatively, the target HR can be set as a percentage of MHR, with recommended exercise intensities ranging from 50% to 85% of MHR, which is equivalent to 40-80% peak VO2.7,8
Finally, the rating of perceived exertion (RPE) is commonly employed in CR, and is particularly valuable in situations in which HR response is unpredictable or difficult to interpret, such as atrial fibrillation, beta-blocker therapy, chronotropic incompetence or pacemaker implantation. The original Borg scale rates perceived effort on a scale from 6 to 20.9
The current consensus on exercise prescription in CR is that minimum training intensity should be around 60% MHR, 50% HRR, or 12-13 on the Borg scale, and maximum intensity should be around 85% MHR, 80% HRR, or 15-16 on the Borg scale.4
Nevertheless, optimum initial exercise intensity prescription in CR patients is still the subject of debate, and there is even less information available on progression in intensity of exercise during CR. Therefore, there is a need for additional studies that focus on this question.
The aim of our study was to describe progression of aerobic exercise intensity in patients on a CR program.
MethodsParticipantsWe performed a retrospective analysis using random digit sampling to generate a sample of patients consecutively referred for CR after acute coronary syndrome between January 2008 and December 2016. Sociodemographic and clinical data were obtained from medical records. Patients with atrial fibrillation (paroxysmal, persistent or permanent) or implantable devices (pacemakers, implantable cardioverter-defibrillators or cardiac resynchronization therapy devices) were excluded.
InterventionThe program consisted of twice-weekly exercise sessions comprising 25 min treadmill training and 10 min stationary cycling, followed by 1-2 series of 15-20 repetitions of resistance exercises. The total program duration ranged from 4 to 12 weeks.
Target HR during exercise sessions was calculated using baseline ET. Initial exercise intensity was set at 60-80% of HRR above resting HR. Increases in intensity over the course of the program were calculated according to both HR response and RPE (11-13 on the Borg scale). HR was continuously monitored during sessions using electrocardiographic telemetry and recorded every 5 min along with the Borg score.
The weekly peak exercise intensity achieved during aerobic exercise was estimated by the speed and grade of the treadmill at peak effort (selected as the stage of the training session at which the highest HR was achieved, as long as the patient was not holding the handrails). The American College of Sports Medicine (ACSM) formulas10 VO2=((speed×0.1)+(speed×1.8×grade)+3.5)/3.5 when walking and VO2=((speed×0.2)+(speed×0.9×grade)+3.5)/3.5 when running were used to estimate level of metabolic equivalents (METs).
Peak HR achieved during exercise sessions was used to estimate the percentage of HRR and of MHR while the patients were training, compared to initial and final ET results. For better understanding of progression during the CR program, peak HR/intensity and RPE on the Borg scale per increase in METS were used as variables to characterize the variation in HR and response to the intensity achieved, respectively.
Statistical analysisContinuous variables were expressed as mean and standard deviation and categorical variables were expressed as proportions. Repeated measures analysis of variance tests were used to compare variables at different time points: T1 (1st week), T2 (4th week) and T3 (8th week).
Subgroup analysis was performed to compare patients whose participation in the CR program ended by eight weeks with those who continued participating beyond that point.
Sample size was calculated using the formula n=2(z1-α/2+z1-β)2/((μ0-μ1)/σ)11 which, for a significance level of 0.05 and power of 80%, using 5 bpm as minimal clinical difference and 20 bpm as standard deviation, meant a total sample of 250 individuals was needed. IBM SPSS® version 20 was used for statistical analysis and random sampling.
The use of patient data for research purposes was approved by our institution's ethics committee and written informed consent was obtained from all patients entering the CR program.
ResultsA sample of 250 patients were randomly selected from a total of 868. Twelve were excluded because of incomplete relevant data in their clinical records. Of the final 238, 84.1% were men and mean age was 53.6±9.5 years. The sample was not significantly different from the general population of patients referred for CR in terms of gender – 85.3% male (p>0.05) – or age – 54.6±10.0 years (p>0.05).
Concerning cardiovascular disease, most patients (82.7%) had undergone percutaneous coronary intervention, 11.4% had received medical treatment only and 5.9% were referred following coronary artery bypass graft surgery. The majority (63.9%) had single-vessel disease, 22.7% two-vessel disease, 8.8% three-vessel disease, and in 4.6% no significant coronary artery occlusion was detected. The first echocardiographic assessment following acute coronary syndrome showed 62.1% had preserved left ventricular systolic function, 22.4% had mild left ventricular dysfunction, 9.9% moderate and 5.6% severe dysfunction. Regarding previous medical history, 10.2% had a history of coronary disease (acute myocardial infarction, unstable angina, or significant coronary artery stenosis), 40.8% had a history of hypertension and 18.2% a history of diabetes.
A subset of patients attended shorter programs (<8 rather than ≥8 weeks), either because they had achieved the goals of rehabilitation or for financial or professional reasons. Patients were therefore divided into subgroups: subgroup 1 (SG1, n=98) – those who completed less than eight weeks; and subgroup 2 (SG2, n=140) – those who completed eight weeks or more. The subgroups did not differ significantly regarding gender (SG1: 84.7% male vs. SG2: 84.3% male; p>0.05), but SG1 were significantly younger than SG2 (SG1: 51.3±9.8 years vs. SG2: 55.2±9.0 years; p<0.01).
Mean functional capacity of 8.8±2.3 METs and mean HRR of 63.8±19.0 bpm were estimated on baseline ET. There was a significant improvement in both functional capacity at ET performed after program completion (10.9±2.1 METs; p<0.001) and HRR (71.5±20.1 bpm; p<0.001).
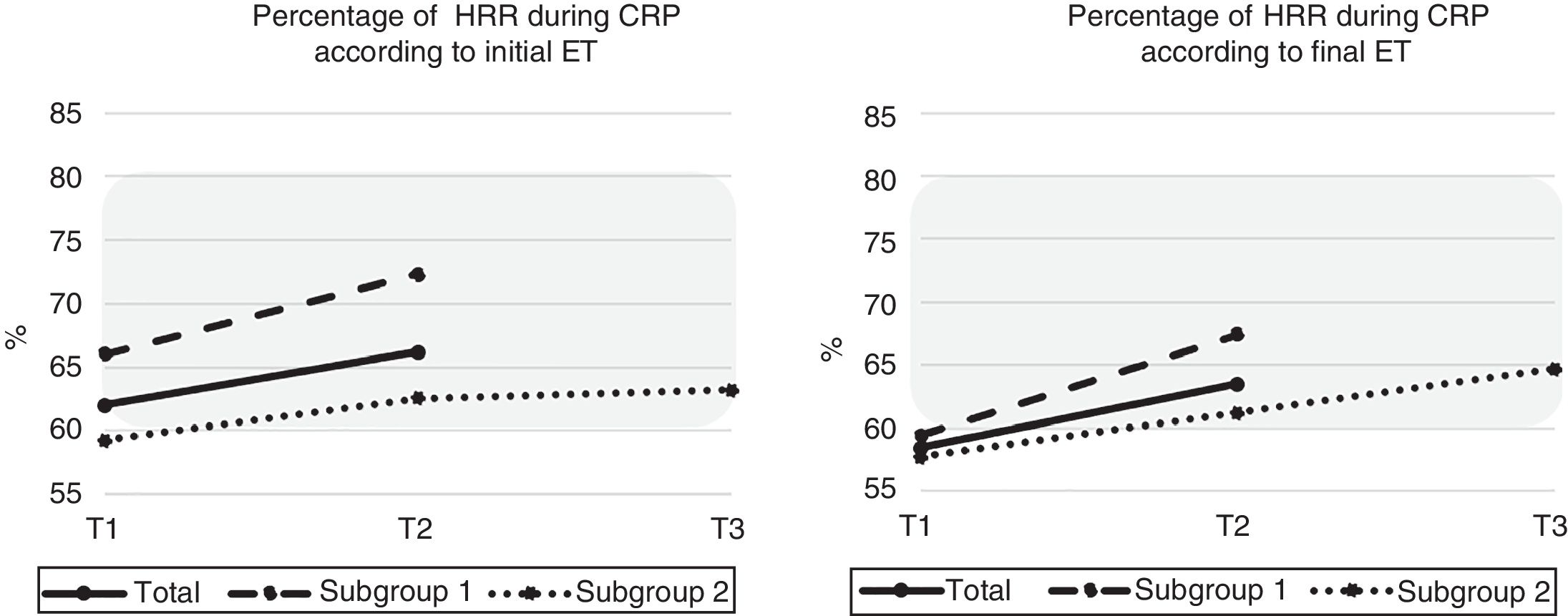
At peak HR during the session, exercise intensity (in METs) was T1: 7.2±2.0, T2: 9.0±2.2 and T3: 9.4±2.2 (p<0.01). Also at peak HR, percentage HRR of baseline ET achieved was: T1: 62.0%, T2: 66.2% and T3: 63.2% (p=0.26). When ET after program completion was used to calculate HRR, percentage HRR achieved was: T1: 58.4%, T2: 63.5% and T3: 64.7% (p<0.01). To further investigate HR variation during CR, subgroup analysis showed that SG1 at peak HR achieved a percentage HRR of T1: 66.0%, T2: 72.3% (p<0.01), regarding baseline ET HRR, while the corresponding figures in SG2 were: T1: 59.1%, T2: 62.5% and T3: 63.2% (p=0.26). Considering the final ET HRR test results, peak HR achieved in SG1 was: T1: 59.3% and T2: 67.4% (p<0.01) and in SG2 it was: T1: 57.8%, T2: 61.2% and T3: 64.7% (p<0.05) (Figure 1).
Percentage of heart rate reserve (HRR) achieved at peak heart rate (HR) during cardiac rehabilitation at T1 (1st week), T2 (4th week) and T3 (8th week), according to HRR calculated at initial exercise testing (ET) (left) and final ET (right) for the total sample (solid line), subgroup 1 (dashed line) and subgroup 2 (dotted line). The shaded area corresponds to the target HR established during aerobic exercise. CRP: C-reactive protein.
In the alternative method, considering percentage of MHR as determined by baseline ET, HR achieved was: T1: 83.7%, T2: 86.1% and T3: 88.0%, (p<0.001). With regard to the MHR of the final ET, the HR achieved was: T1: 79.7%, T2: 81.9% and T3: 83.7% (p<0.001). These results were also confirmed in the subgroup analysis: according to first ET, SG1 achieved percentage MHR of: T1: 83.6% and T2: 86.3% (p<0.01); the corresponding figures for SG2 were: T1: 83.8%, T2: 85.9% and T3: 88.1% (p<0.001). When ET was used after program completion, HR achieved by SG1 was: T1: 79.3% and T2: 82.1% (p<0.01), while SG2 achieved HR of T1: 80.0%, T2: 81.7% and T3: 83.7% (p<0.001).
The corresponding Borg scores were: T1: 12.2±0.92, T2: 12.1±0.93 and T3: 12.0±0.94 (p<0.05). In the subgroup analysis, the Borg scores of SG1 at peak exercise intensity were: T1: 12.0±0.82 and T2: 11.8±0.93 (p<0.05), while those of SG2 were: T1: 12.3±0.97, T2: 12.1±0.91 and T3: 12.0±0.94 (p<0.05).
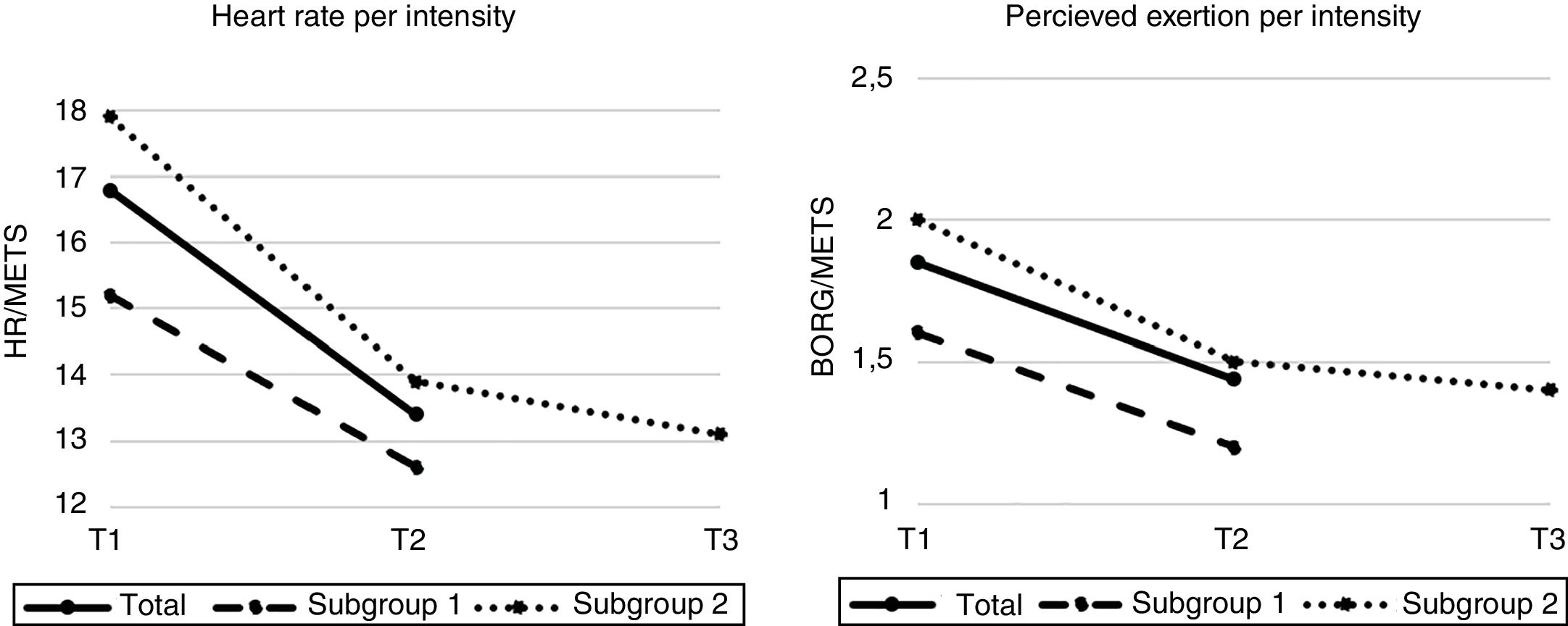
For the total sample, the peak HR/intensity index decreased significantly (T1: 16.8±5.4, T2: 13.4±3.6 and T3: 13.1±3.8; p<0.001). In the subgroup analysis, peak HR/intensity in SG1 was: T1: 15.2±4.2 and T2: 12.6±3.0 (p<0.001), with similar figures in SG2: T1: 17.9±5.8, T2: 13.9±3.9 and T3: 13.1±3.8 (p<0.001) (Figure 2).
(Left) Heart rate (HR) per exercise intensity expressed in beats per minute (bpm)/metabolic equivalents (METs) during cardiac rehabilitation at T1 (1st week), T2 (4th week) and T3 (8th week) for the total sample (solid line), subgroup 1 (dashed line) and subgroup 2 (dotted line); (right) rating of perceived effort (RPE) per exercise intensity expressed as Borg RPE score/METs during the same period.
The Borg/intensity index was: T1: 1.85±0.6, T2: 1.44±0.5 and T3: 1.40±0.5 (p<0.001) in the total sample. In SG1 this index was: T1: 1.6±0.6 and T2: 1.2±0.4 (p<0.001), while in SG2 it was: T1: 2.0±0.7, T2: 1.5±0.5 and T3: 1.4±0.5 (p<0.001) (Figure 2).
Regarding chronotropic medication in our sample, 84.3% were on beta-blockers at the start of the program and 7.7% started beta-blocker therapy during the CR program. Analysis of dose changes in the same period showed that 41.8% increased, 39.1% maintained and 19.1% decreased dosage. We further analyzed the progression of exercise intensity in these three subgroups of patients (ID – increased dose; MD – maintained dose; DD – decreased dose) and concluded that all three showed similar results, with significantly increased intensity achieved at peak exercise (ID: T1: 6.7±1.7 vs. T2: 8.8±2.1 vs. T3: 9.9±2.1; p<0.01, MD: T1: 7.2±2.0 vs. T2: 9.3±2.2 vs. T3: 9.8±2.2; p<0.01, DD: T1: 6.5±2.6 vs. T2: 8.8±3.1 vs. T3: 8.4±2.6; p<0.01); and significantly decreased peak HR/intensity index (ID: T1: 18.0±4.9 vs. T2: 13.9±3.2 vs. T3: 12.2±3.0; bpm/MET; p<0.01, MD: T1: 16.3±5.3 vs. T2: 12.9±4.0 vs. T3: 13.2±3.9; bpm/MET; p<0.01, DD: T1: 16.5±5.8 vs. T2: 13.4±5.1 vs. T3: 13.6±5.8; bpm/MET; p=0.02); and RPE index across the board (ID: T1: 2.0±0.6 vs. T2: 1.5±0.4 vs. T3: 1.3±0.3; p<0.01) (MD: T1: 1.8±0.6 vs. T2: 1.4±0.5 vs. T3: 1.3±0.4; p<0.01, DD: T1: 2.0±0.8 vs. T2: 1.6±0.8 vs. T3: 1.6±0.8; p<0.01).
DiscussionThese results show that functional capacity improves significantly during a CR program based on moderate intensity aerobic exercise, as has been widely described in the literature.12 We also showed an increase in HRR, which is a prognostic factor in cardiac disease, reflecting chronotropic variability and overall neurohumoral response.13
However, there is high intra- and inter-individual variability in physiological responses to exercise and effort perception.14 Our study showed that perception of effort is a key component to guide progression during exercise sessions, especially in coronary disease patients, in whom HR response to exercise may be unpredictable and difficult to interpret, because of beta-blocker therapy, atrial fibrillation, chronotropic incompetence or pacemaker implantation.15,16
Exercise prescription using percentage of HRR to guide target HR, usually 60-80%, appears to be appropriate, since most patients in our study remained within this range at peak exercise, although at the lower end, and their exercise capacity improved significantly. When using percentage of MHR, patients appear to reach values of 80-85%, which is at the upper end of the recommended range, meaning these criteria are not interchangeable.4 Which method is superior remains to be determined, although studies have shown that percentage of HHR seems to correlate more strongly with the physiological use of energy for maximal effort attainment, as it takes the baseline level into account.4
Comparing ET results at baseline and at the end of CR in terms of percentage of HRR and MHR achieved, we found similar values, which indicates that exercise prescription for the later non-supervised phase, based on the initial ET and progression during the CR program, may be sufficient to guide progression of exercise intensity.
We also used a relatively conservative RPE range of 11-13, corresponding to a ‘fairly easy’ to a ‘fairly hard’ perception of effort, which may have limited increases in intensity and peak HR achieved during the sessions to some extent. Additional studies using a higher limit of the Borg RPE score, in a controlled environment with close monitoring, could enable higher intensities to be achieved and boost functional benefit without an increase in exercise-related risk.
Decrease in both HR and RPE per unit increase in exercise intensity is an indicator of functional, neurohumoral and cardiovascular improvement.17 Of note, the main improvements in these parameters were seen in the first four weeks of treatment in those on a longer CR program, with less visible change after this period, which may indicate that most physiological adaptations to exercise occur earlier in the CR program and that there might be a need to incorporate variations or even new types of higher-intensity aerobic exercise in CR after the first month, especially in older patients.
We should also acknowledge that this group was mainly composed of male patients, most of whom were referred for CR following an acute coronary event with percutaneous coronary intervention, with one- or two-vessel disease, preserved or mildly impaired left ventricular systolic function, and no previous medical history of significant coronary disease. This profile may limit the overall generalizability of the results to patients with more severe or prolonged heart disease.
Importantly, the ACSM's formulas for estimating exercise intensity10 specify whether subjects are running or walking and that they are not holding the treadmill handrails, as these aspects of ET can affect the intensity achieved and could result in inappropriate exercise intensity prescription if not considered.
This is a study with a large sample of coronary patients, with a well-structured supervised exercise intervention, using exercise prescription based on prior ET, in which variables such as HR, perceived exertion, and intensity of exercise were collected in a standardized manner.
Among the main limitations of this analysis are that it was retrospective, there was high variability in number of sessions completed, cardiopulmonary testing was not available, and there were no data on adverse effects related to the intervention.
ConclusionsIncreased exercise intensity during CR leads to significant improvement in functional capacity.
Initial exercise intensity prescription based on HRR and progression in intensity according to perceived exertion appears to be capable of safely and effectively achieving this functional improvement.
However, there also appears to be room for improvement, as peak HR during sessions was below the calculated upper limit for HRR, and a higher RPE score might be allowed in low-risk patients at peak effort. This may help bring about a change from range-based to threshold-based prescription of aerobic exercise intensity.
Finally, there may be a need to further diversify the supervised exercise intervention in coronary patients, especially after the first four weeks of treatment, in order to maximize gains in functional capacity during the CR program.
Conflicts of interestThe authors have no conflicts of interest to declare.