To present the report on the trends in percutaneous coronary activity data in Portugal from the last decade (from 2014 to 2023).
MethodsData were extracted from the Portuguese National Registry of Interventional Cardiology (RNCI) and the numbers in recent years were compared and complemented by information from the 2023 European Society of Cardiology Atlas in Interventional Cardiology (IC) survey, which was administered to the director of every IC department. Linear regression analysis was used to assess trends in activity over time.
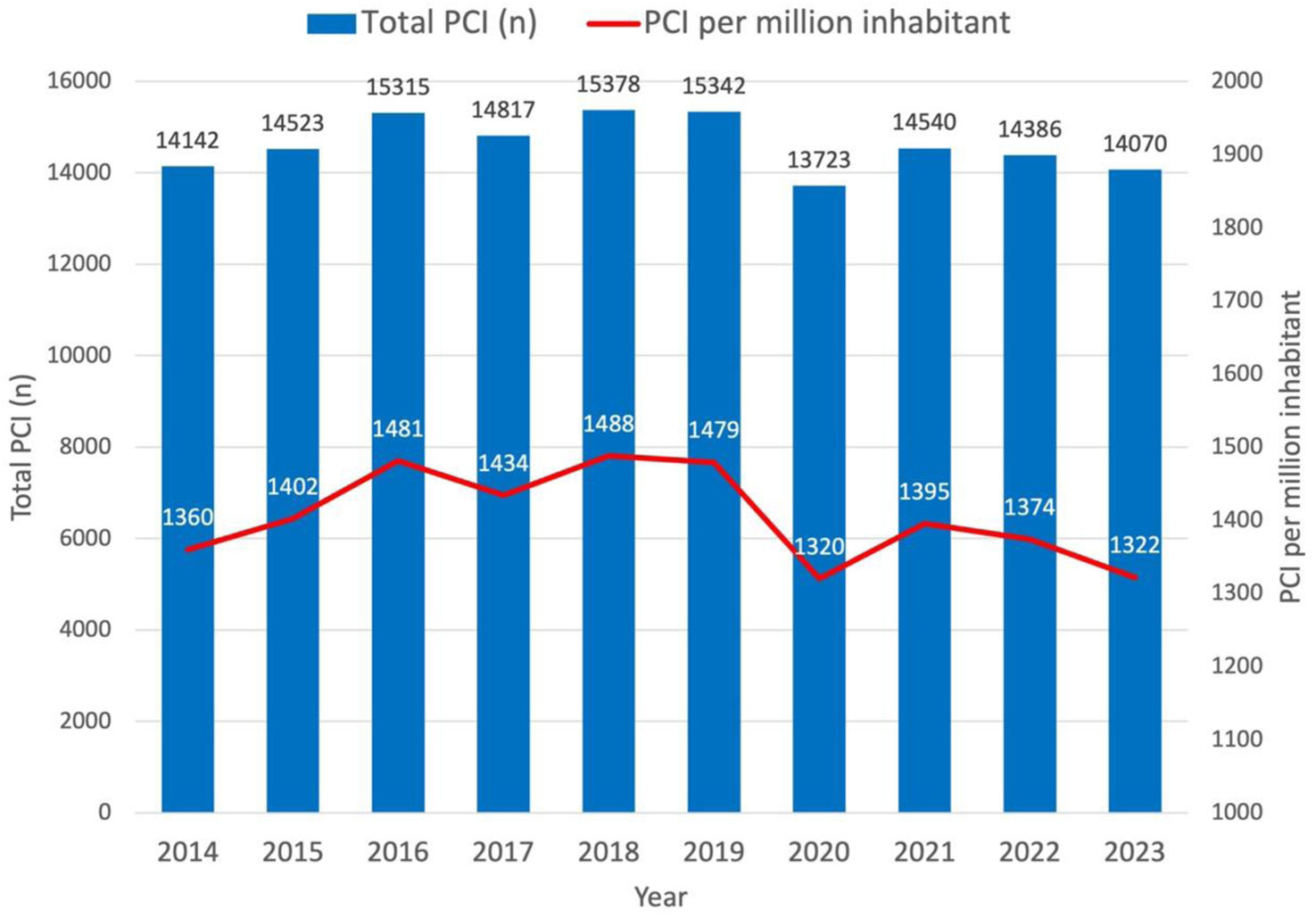
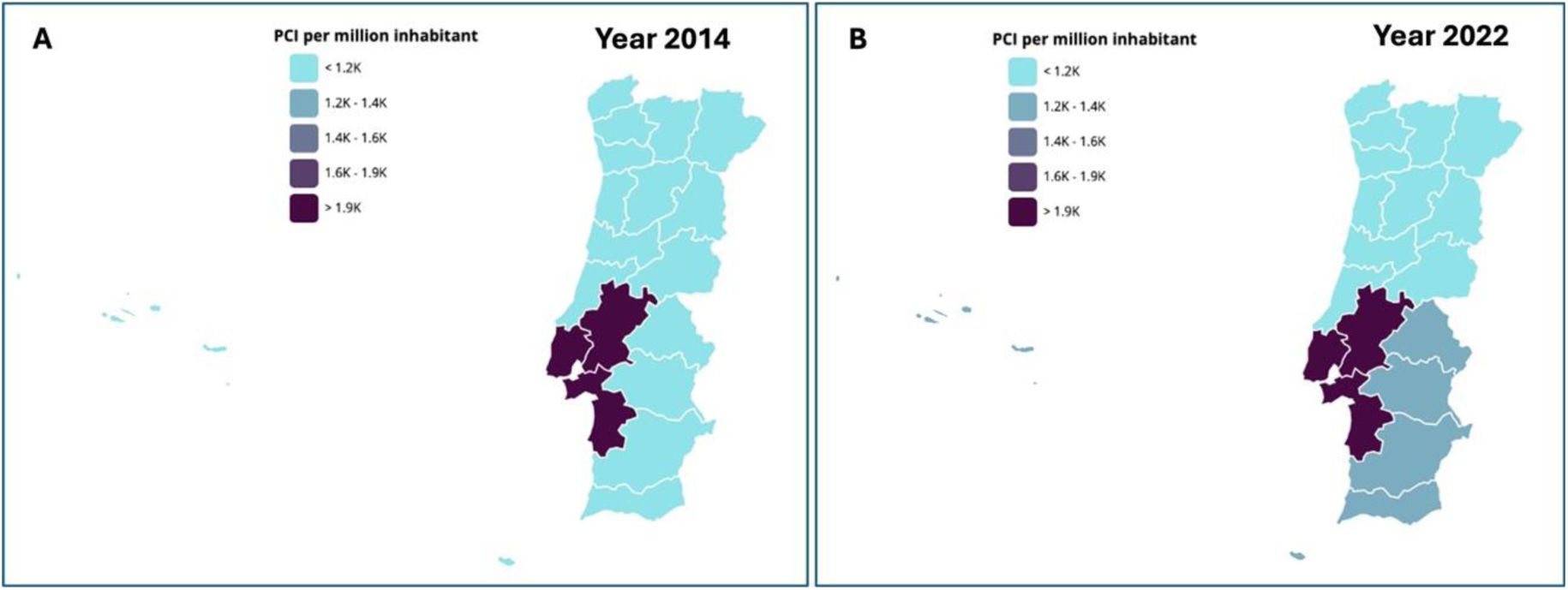
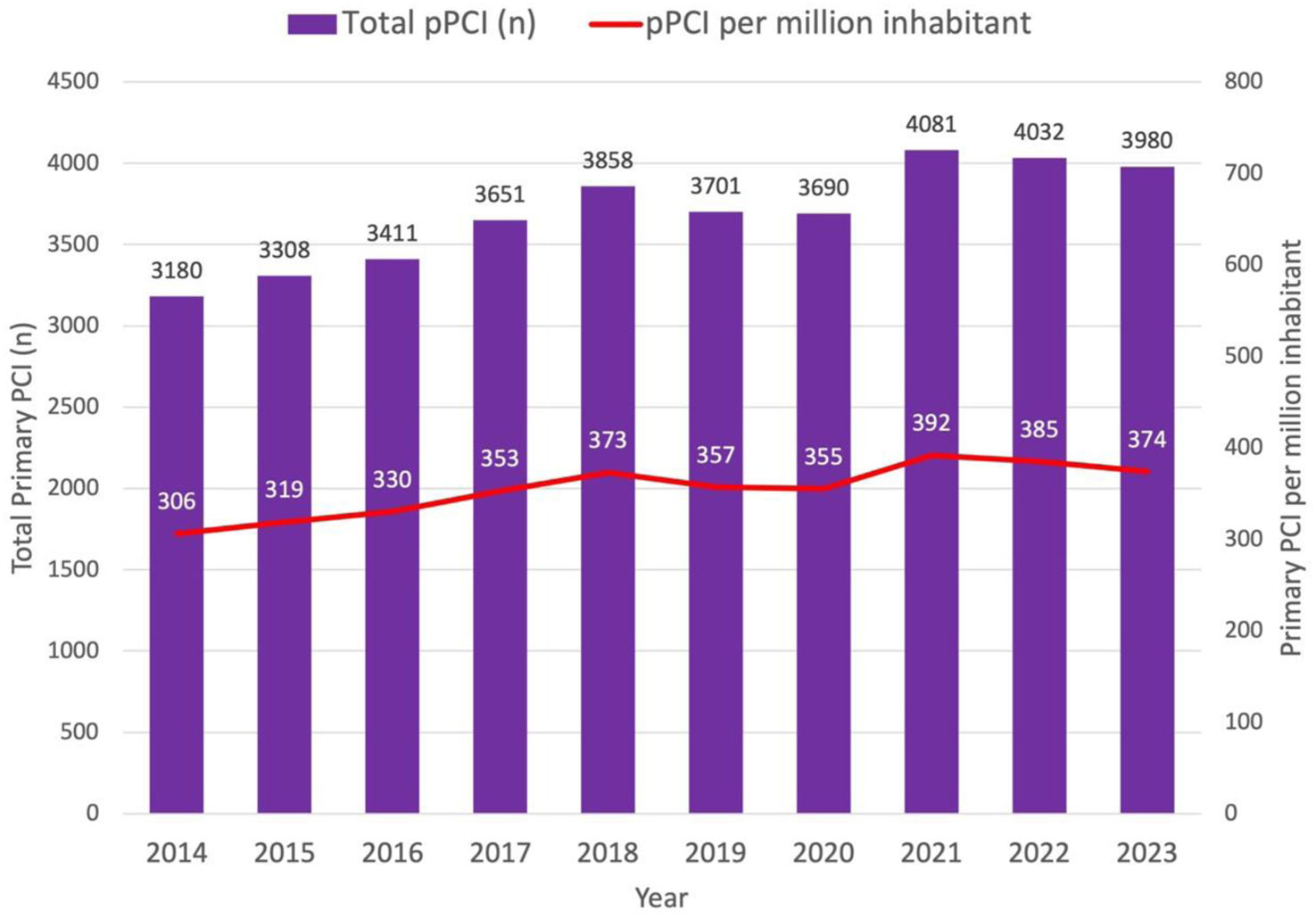
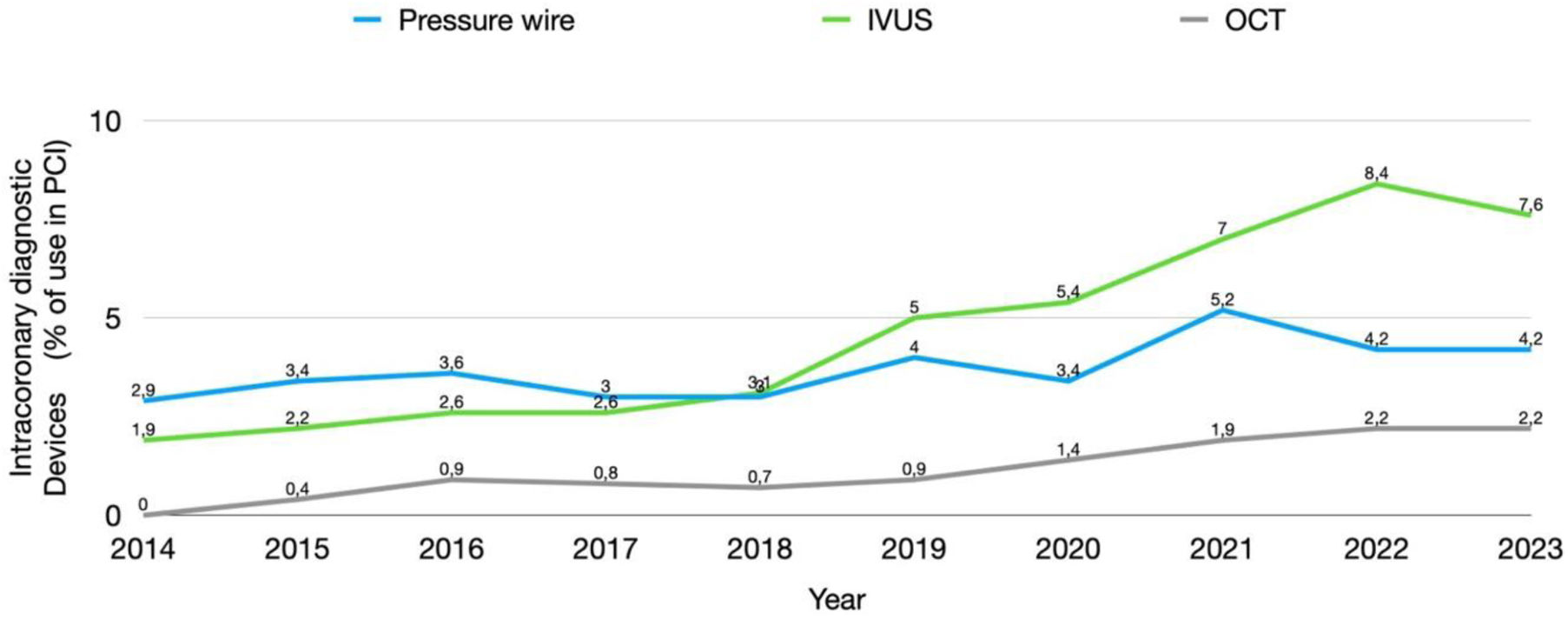
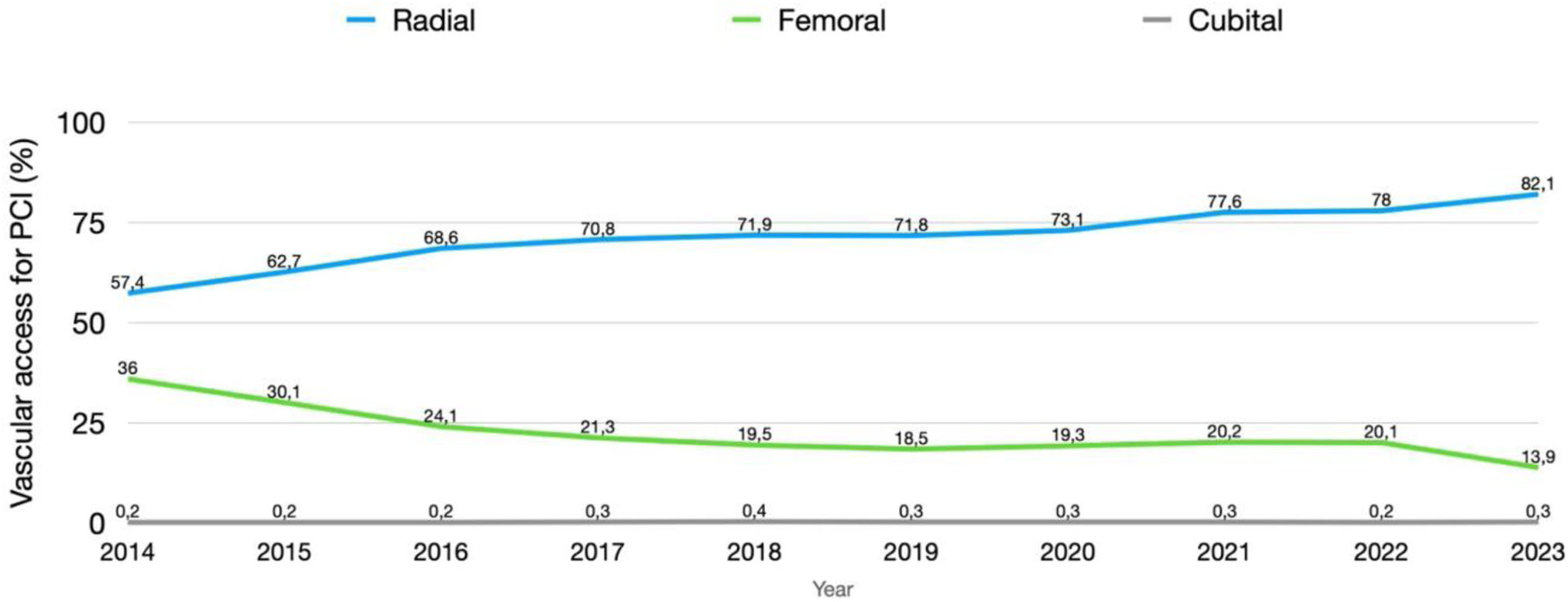
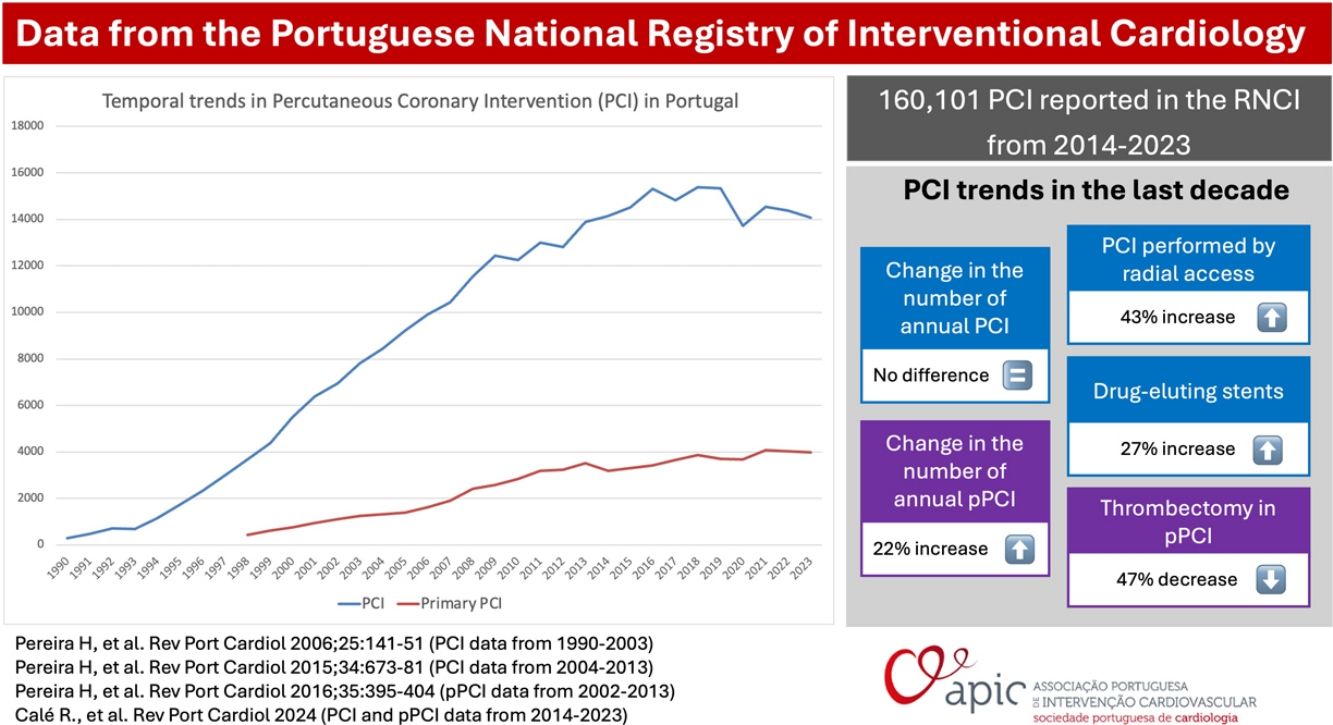
ResultsFrom 2014 to 2023, there were 160101 percutaneous coronary interventions reported in the RNCI. The number of annual PCI in the last decade remained constant (1360/million inhabitants in 2014 to 1322/million in 2023; R2=0.039, p=0.276). Importantly, there was a 22% increase in primary PCI (306/million inhabitants in 2014 to 374/million inhabitants in 2023; R2=0.759, p<0.001) and there was a decrease in the geographical disparities in primary PCI across Portugal. The following PCI trends were noted: a 43% increase in PCI performed by radial access (57.4% in 2014 to 82.1% in 2023; R2=0.908, p<0.001), a 27% increase in drug-eluting stents (78.4% in 2014 to 99.2% of all PCI with stents in 2023; R2=0.638, p=0.003), and a 47% decrease of thrombectomy in primary PCI (35.0% in 2014 to 18.6% in 2023; R2=0.649, p=0.003). There was a slight increase in the use of intracoronary diagnostic devices during PCI, with intravascular imaging and physiological assessments reaching 7.6% and 4.2%, respectively, in 2023.
ConclusionThe RNCI was able to depict changes in our practice along the study period. The annual PCI volume per million inhabitants remained stable, driven by an increase in primary PCI offset by a decrease in chronic coronary syndrome indications. The geographical asymmetries were markedly reduced due to the expansion on PCI capable centers, enabling a progress towards a more universal access to percutaneous coronary techniques.
Apresentar o relatório de atividade do Registo Nacional da Cardiologia de Intervenção (RNCI) com os dados da angiografia e intervenção coronária percutânea em Portugal na última década (de 2014 a 2023).
MétodosOs dados foram baseados no RNCI e os números dos últimos anos foram comparados e complementados com a informação do Atlas ESC em Cardiologia de Intervenção (CI) de 2023, com um questionário que foi aplicado aos responsáveis de cada departamento de Cardiologia de Intervenção. Foi utilizada uma análise de regressão linear para avaliar as tendências de atividade ao longo do tempo.
ResultadosDe 2014 a 2023, foram reportadas 160.101 intervenções coronárias percutâneas (ICP) no RNCI. O número anual de ICP na última década manteve-se constante (1360/milhão de habitantes em 2014 para 1322/milhão em 2023; R2=0,039, p=0,276). Por outro lado, verificou-se um aumento de 22% nas ICP primárias (306/milhão de habitantes em 2014 para 374/milhão de habitantes em 2023; R2=0,759, p<0,001) e uma redução das disparidades geográficas na penetração da ICP primária em todo o território nacional. As seguintes tendências em ICP foram observadas: um aumento de 43% nas ICP realizadas por acesso radial (57,4% em 2014 para 82,1% em 2023; R2=0,908, p<0,001), um aumento de 27% no uso de stents farmacológicos (78,4% em 2014 para 99,2% de todas as ICP com stents em 2023; R2=0,638, p=0,003) e uma redução de 47% na trombectomia durante ICP primária (35,0% em 2014 para 18,6% em 2023; R2=0,649, p=0,003). Verificou-se um ligeiro aumento na utilização de dispositivos de diagnóstico intracoronário durante a ICP, com a imagiologia intravascular e as avaliações fisiológicas a atingirem 7,6% e 4,2%, respetivamente, em 2023.
ConclusãoO RNCI reflete as mudanças na nossa prática ao longo do período do estudo. O volume anual de ICP por milhão de habitantes manteve-se estável devido ao aumento da ICP primária, equilibrado pela diminuição das indicações por síndrome coronária crónica. As assimetrias geográficas foram significativamente reduzidas graças à expansão dos centros com capacidade para realizar ICP, traduzindo-se num acesso mais universal à intervenção percutânea coronária.
The Portuguese National Registry of Interventional Cardiology (RNCI) is a multicentric prospective voluntary registry that includes all consecutive percutaneous coronary intervention procedures since it was created in 20021 by the Portuguese Society of Cardiology (SPC).
The RNCI is headquartered at the National Center for Data Collection in Cardiology (CNCDC) and aims to continuously collect all activity within the scope of Interventional Cardiology occurring in all cardiac catheterization laboratories (cath labs) nationwide from public and private centers in mainland Portugal and the islands. It is the responsibility of Portuguese Association of Interventional Cardiology (APIC) to design, implement, develop, monitor, and support the RNCI.
To unify and standardize the collection, storage, and exchange of clinical data between our RNCI and other countries within Europe, the clinical data was collected based on the European Data Standards for Clinical Cardiology Practice (CARDS) developed by the European Society of Cardiology (ESC).2 The primary goal of these standards is to improve the quality and consistency of clinical data, facilitating research, clinical practice, and evidence-based decision making.
Previous studies have documented the activity trends in National Interventional Cardiology during the periods 1992–2003 and 2004–2013, indicating a progressive increase in procedural volume over these years.3,4 A more specific analysis of primary angioplasty data from 2002 to 2013 showed that the rate per million inhabitants tripled during these years.5
ObjectivesWe aim to present the most recent results of the RNCI activity over the past ten years (2014–2023) as a continuity of the previously published data. The results of the present analysis will be discussed and compared with previous years and with data from other European registries.6,7
MethodsThe data collection for the RNCI is a process that involves the initial systematic collection of data at each catheterization laboratory (cath lab) by healthcare professionals, who are doctors, nurses, or technicians working in their respective units. This collection includes all percutaneous coronary intervention (PCI) procedures. Periodically, these data are sent to a centralized database in an anonymized format. In 2023, the data were extracted from 28 national cath labs, 20 public (one of them began activity and started submitting data in 2023) and eight private one (Supplementary Table 1), distribuged geographically as per Supplementary Figure 1.
To assess the representativeness of gathered data and ensure they reflect the reality of the entire population, the RNCI figures for the year 2022 were compared with the information from the ESC Atlas in Interventional Cardiology (IC) survey 2023 (Supplementary Table 2 – data from procedures and resources for coronary intervention section), performed in the same year, with data sent by each cathlab in Portugal. This survey gathers information from 26 hospitals, of which 19 are public and seven are private.
In 2022, data collection from diagnostic procedures began. The data from diagnostic procedures from 2022 in the RNCI were also compared with the information from the ESC Atlas in IC survey for the same year.
Statistical analysisContinuous variables were presented as mean±standard deviation, and a comparison between variables was performed with an independent t-Student test. Categorical variables were presented by numbers (n) and percentages (%) and a comparison between groups was performed using Qui-square test or Fisher's exact test, when appropriate.
The percentage difference of activity or devices used between the last and the first year was calculated using the following formula: % increase=100×(final absolute number−initial absolute number/initial).
Linear regression analysis was used to assess trends over time. The results are presented as the adjusted R-squared (R2).
All reported p values were 2-sided and a p value <0.05 was considered statistically significant.
Statistical analysis was performed with IBM SPSS Statistics 29.0.2.0 (IBM Corp, Armonk, NY, USA).
ResultsOver the past decade, all public IC centers have submitted their data to the RNCI. In 2014, there were 19 participating centers, with the addition of Centro Hospitalar Baixo Vouga in 2023, bringing the total to 20 centers. As for private centers, the number of exporting centers has been increasing over the years, with eight private centers exporting data in 2023 (Supplementary Table 1).
Coronary angiographyAccording to the ESC Atlas in IC survey, 32519 diagnostic catheterization procedures were performed in 2022; the percentage of PCI relative to the number of diagnostic procedures was 43%. According to the RNCI, 23427 coronary angiographies were recorded in 2022, representing 72% of the total diagnostic procedures performed that year.
Percutaneous coronary interventionIn 2014, a total of 14142 PCI were performed across the whole of continental Portugal and the islands, amounting to 1360 per million inhabitants. The numbers of PCI have remained constant over the past decade (R2=0.039, p=0.276), totaling 14070 PCI in 2023 (1322 per million inhabitants).
In 2022, PCI was performed in 14386 cases. These figures are consistent with those reported by the ESC Atlas in IC survey (Supplementary Table 2), demonstrating a high level of representativeness of the registry in relation to the total number of procedures performed annually in Portugal. By analyzing Figure 1, it is noticeable that there was a slight reduction in the total number of PCI in the year 2020 during the Covid-19 pandemic period (−10.6% compared to the year of 2019), which was followed by a recovery in the subsequent years.
In Figure 2, regional disparities in the use of PCI per million inhabitants are evident. Tagus Valley and Lisbon has the highest numbers of PCI per million inhabitants in Portugal, with the numbers remaining stable from 2014 (2113 PCI/million inhabitants) to 2022 (2061 PCI/million inhabitants). The Southern region and islands saw the most significant growth in PCI over the past decade (from 940 to 1254 PCI/million inhabitants). The rates of PCI remained stable in Northern and Central regions at close to 1100 PCI per million inhabitants.
Primary percuntaneous coronary interventionFigure 3 illustrates the progression of primary angioplasty (pPCI) in Portugal from 2014 to 2023, presented in both absolute numbers and pPCI per million inhabitants. We observed a slight increase in the number of pPCI per million inhabitants over the years, with an incremental rate of 22% from 306 per million inhabitants in 2014 to 374 per million inhabitants in 2023 (R2=0.759, p<0.001). In 2022, we collected 4032 pPCI in the RNCI (385 pPCI per million inhabitants), representing 92% of the pPCI collected by the ESC Atlas in IC survey.
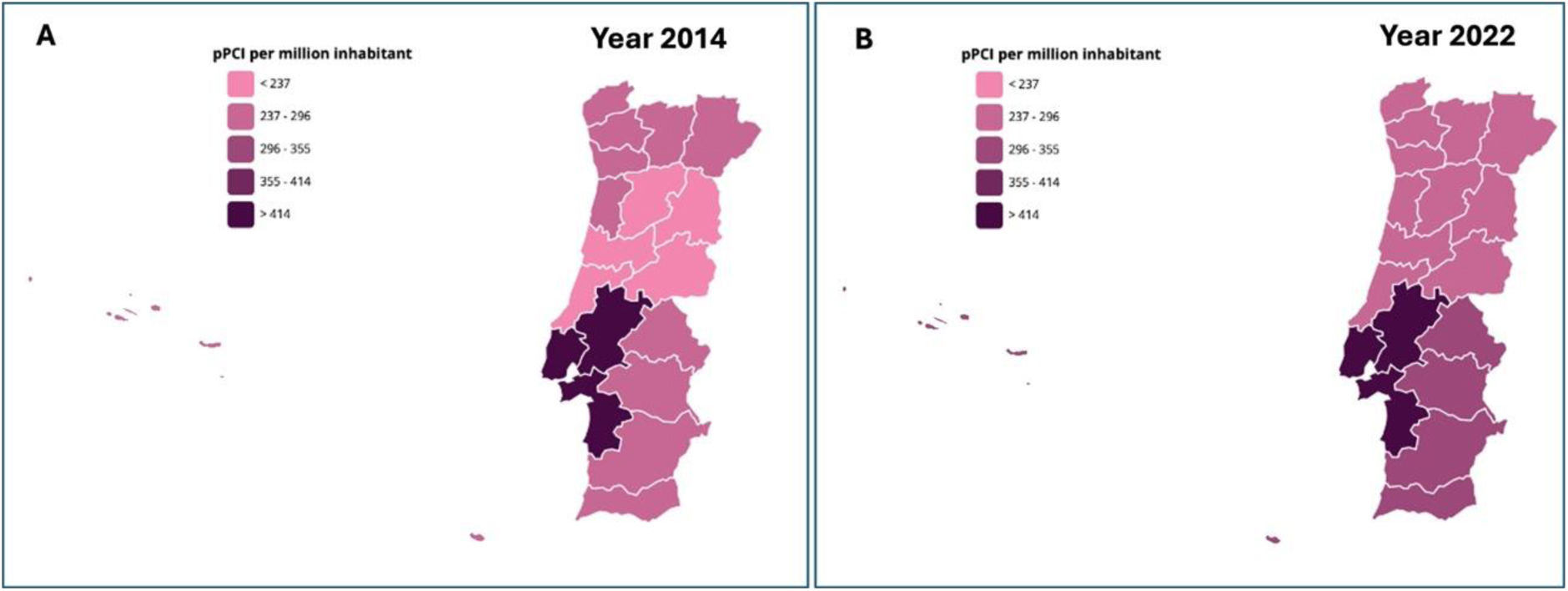
In 2014, the Central region had the lowest rate of primary PCI, with 178 pPCI per million inhabitants (Figure 4A). By 2022, this region had seen significant improvement, nearing the values of the Northern region at 296 pPCI per million inhabitants (Figure 4B). The region with the highest pPCI values over the last decade has been Tagus Valley and Lisbon (525 per million inhabitants in 2022). In the Southern region, an increase in pPCI numbers was also observed from 2014 to 2022 (272–392 per million inhabitant).
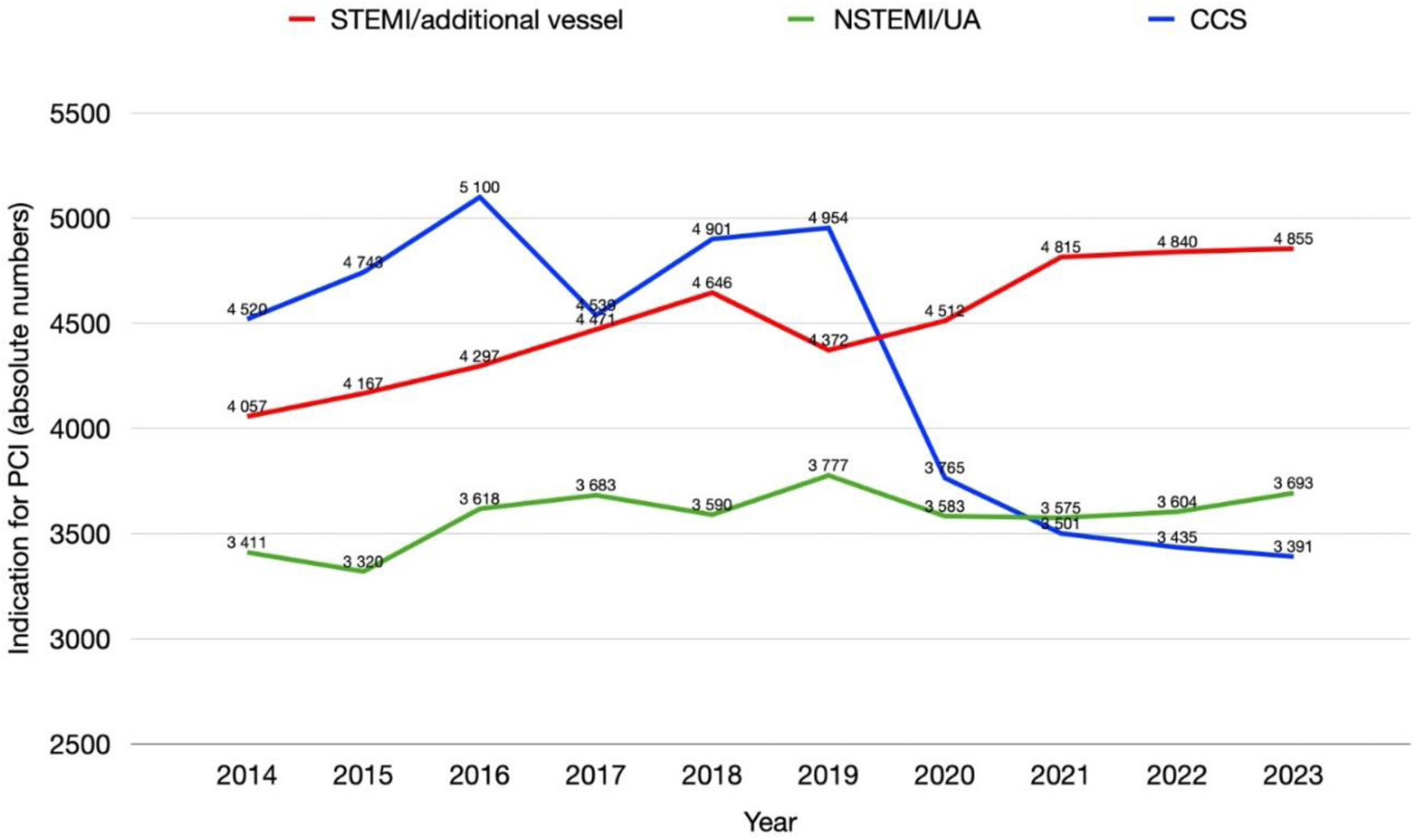
In the last decade, there has been a slight overall increase in the absolute number of PCI conducted in the context of acute coronary syndromes, primarily due to a rise in procedures related to ST-elevation myocardial infarction (R2=0.837, p<0.001). In contrast, the number of PCIs performed for non-ST acute coronary syndromes has remained stable (R2=0.250, p=0.100). Notably, a significant change was observed during the COVID-19 pandemic and subsequent years, marked by a reduction in the number of PCIs performed for chronic coronary syndromes (R2=0.581, p=0.006) (Figure 5).
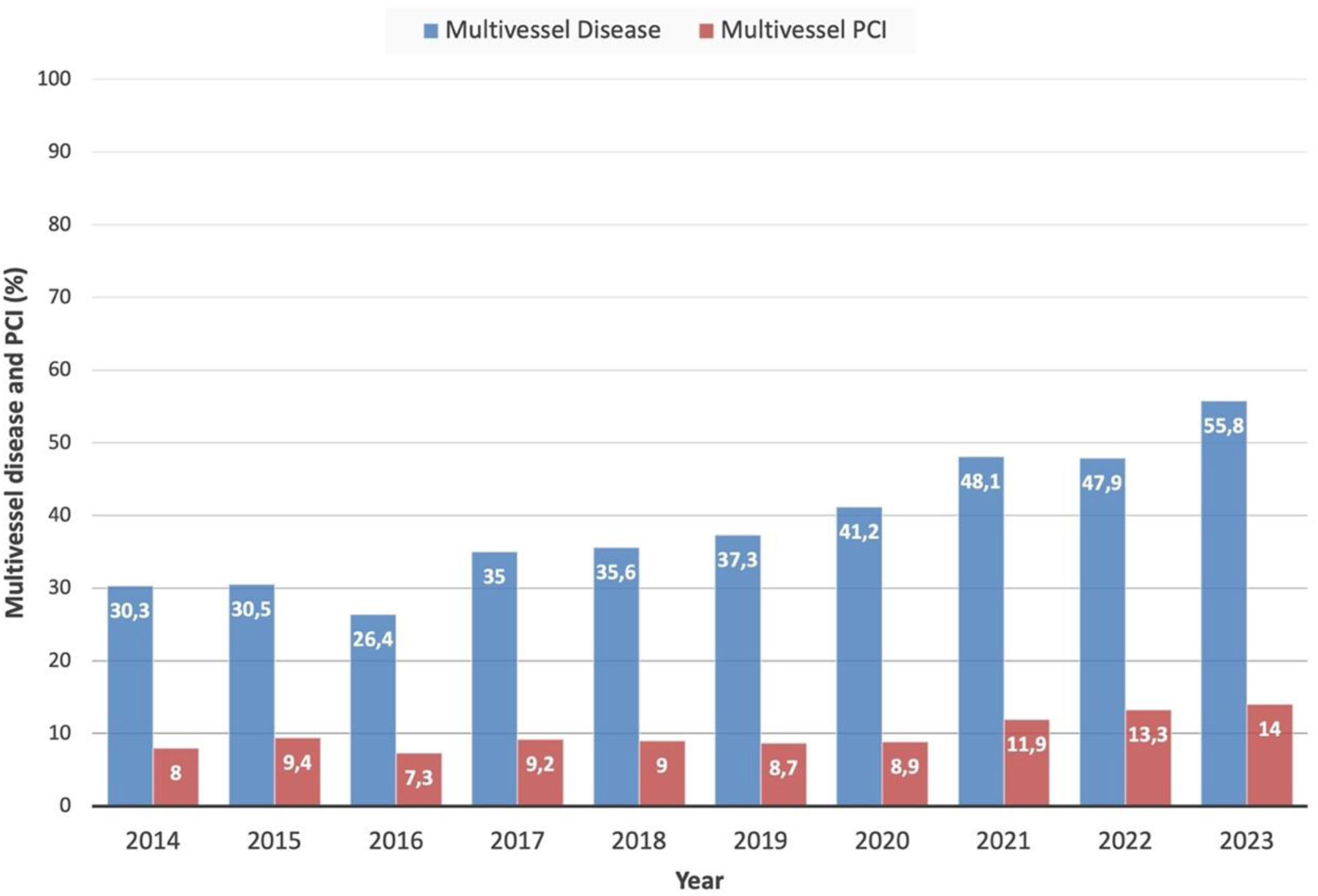
Complex percutaneous coronary interventionOver the past decade, there has been an increase in multivessel disease in patients treated with PCI (Figure 6), accounting for 30.3% of intervention cases in 2014 compared to 55.8% in 2023 (R2=0.875, p<0.001). Although, the number of procedures involving multivessel PCI has increased over the years (R2=0.651, p=0.003), the percentage of its utilization in the same procedure remains low, averaging 9.5% overall years. The number of PCI for additional vessels that were deferred to a second procedure is unknown.
Over the years, the average use of angioplasty in complex anatomies registered in the RNCI were: 7.7% in bifurcations, 2.8% in left main, 1.0% in chronic total occlusions, and 3.7% in stent restenosis.
In 2022, according to data from the RNCI, PCI was used in complex anatomies as follows: 5.6% in bifurcations (n=595/10554), 3.6% in left main (n=480/13252), 1.7% in chronic total occlusions (n=230/13252) and 3.5% in stent restenosis (n=462/13252). In the ESC Atlas IC survey, PCI was used for complex anatomies in 5.7% (594/10331) for chronic total occlusions, 5.1% (629/12307) for unprotected left main, 7.4% (713/9611) for in-stent restenosis.
StentsStents were used on average in 91.8% of cases, with a significant increase in the use of drug-eluting stents (DES) in the last decade (78.4% in 2014 to 99.2% of all PCI with stents in 2023; R2=0.638, p=0.003), approaching almost 100% in recent years. In 2014, bioresorbable vascular scaffold (BVS) were used in 1% of angioplasties with a peak use in 2015 with 1.3% of cases, followed by a decrease in the following years. From 2018 to 2022, there are no records of use of BVS.
In 2022, stents were used in 88.5% of coronary angioplasties and according to data from the ESC Atlas IC survey PCI performed with the use of any drug-eluting balloon was 6.3%. No BVS was reported in this survey.
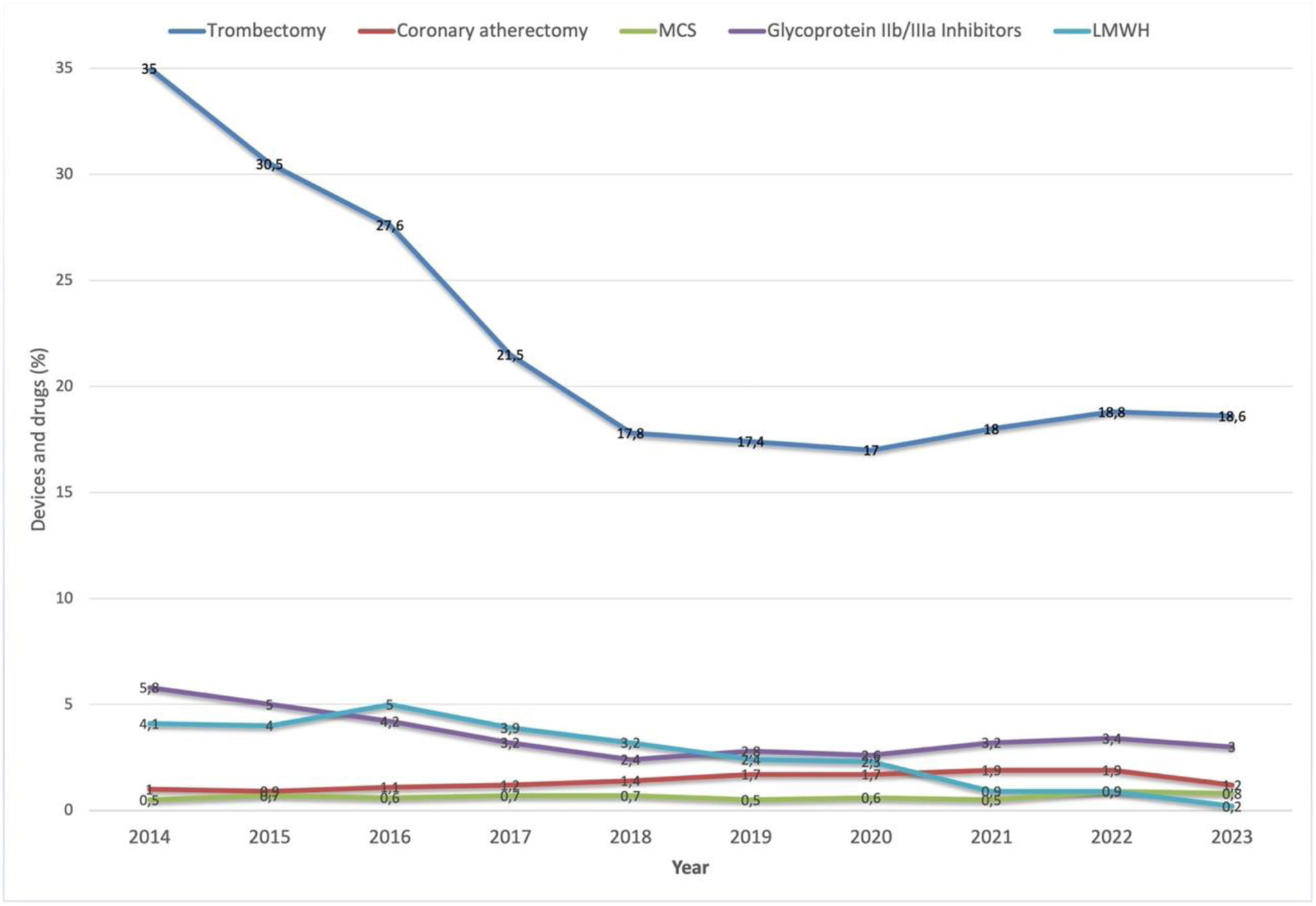
Other coronary intervention devicesManual thrombectomy in primary angioplasty has declined significantly over the past decade from 35.0% in 2014 to 18.6% in 2023 (R2=0.649, p=0.003; Figure 7).
The rate of rotational atherectomy has remained <2% over the years. Although its application remains limited to a small proportion of PCI procedures performed annually, there has been a consistent upward trend in its use over the past decade, increasing from 1.0% in 2014 to 1.9% in both 2021 and 2022 (R2=0.452, p=0.021; Figure 7). In 2022, the percentage of atherectomy use in the RNCI was 1.9%, similar to the results reported in the ESC Atlas in IC survey (2.1%).
Left ventricular mechanical support devices were used in less than 1% of PCI (Figure 7); 0.9% were reported in 2022 according to the RNCI and 1.0% according to the survey. Their usage has remained stable over the years (R2=0.074, p=0.234).
Intracoronary diagnostic devicesThe use of a pressure wire during PCI has seen a modest increase over the past decade (R2=0.430, p=0.024), reaching a plateau in recent years at around 4.2%. In contrast, there has been a more marked growth in the use of intravascular ultrasound imaging both as a diagnostic tool and as a guide for angioplasty, with usage rates varying from 1.9% in 2014 to 7.6% in 2023 (R2=0.907, p<0.001; Figure 8).
In the ESC Atlas in IC survey, in 2022, the PCI use rates with adjunctive intracoronary imaging techniques and physiology measurements were 7.8% and 5.7%, respectively. Additionally, the use of adjunctive intracoronary physiology measurements in procedures (coronary angiography and PCI) was 4.8%.
Antithrombotic treatment during percutaneous coronary interventionRegarding the drugs used during PCI, glycoprotein IIb/IIIa inhibitors have been used less frequently (R2=0.446, p=0.021); the highest usage rate was recorded in 2014 (5.8%) and the lowest in 2018 (2.4%) – see Figure 7.
Regarding the anticoagulant used during PCI, unfractionated heparin is the most used. The use of low molecular weight heparins are minimal, averaging approximately 3.0%, and has declined in recent years from 4.1% in 2014 to 0.2% in 2023 (R2=0.867, p<0.001; Figure 7). There are no records of bivalirudin being use in the period of the study.
Vascular access for percutaneous interventionRadial access has become the preferred access for PCI over the past decade, with rates progressively increasing to a peak of 82.1% in 2023 (R2=0.908, p<0.001; Figure 9). The use of femoral access has evolved in the opposite direction, progressively decreasing over the past few years. The use of cubital access is minimal, with an average utilization rate of 0.3% over the past decade. In the year 2022, the number of coronary angiographies performed via radial access was 90.8%. In the ESC Atlas in IC survey, PCI performed via trans-radial access was 86.1%.
DiscussionThe RNCI is a comprehensive and powerful tool to study the national development of interventional cardiology practices, their regional trends, and benchmarking each cath lab in Portugal. These data are crucial for healthcare professionals and policymakers in their process of decision making, thereby driving initiatives aimed at reducing disparities in cardiovascular disease burden.
The registry, initiated in 2002 by SPC President Ricardo Seabra-Gomes and expanded in 2013 under APIC President Helder Pereira to include all public centers, has evolved through multiple revisions, the latest in 2022 led by a Taskforce coordinated by Rui Campante Teles.4 It now collects consecutive PCI data from 28 public and private centers.
When comparing the total number of PCI and primary PCI in 2022, from two different sources, the RNCI and data from the ESC Atlas in IC survey sent to all coordinators of national public and private cath labs, the numbers are very similar (102% and 92%, respectively). The representiveness of the presented figures is reinforced by the fact that data from consecutive coronary interventional procedures were received from all public centers nationwide and most private centers; most data were sent automatically and digitally.
Regarding coronary angiographies, the data are not as representative as for PCI. Currently, the RNCI have approximately three-quarters of all diagnostic procedures from 2022, when compared to the 2022 ESC Atlas IC survey. Routine transfer for diagnostic procedure data started later and is currently in a phase of progressive implementation.
It is important to have data on coronary diagnostic procedures for several reasons. It is the only way to assess whether patients with acute myocardial infarction proposed for invasive strategy are being treated with angioplasty versus medical or surgical therapy. Additionally, it enables us to evaluate the percentage use of invasive diagnostic methods such as physiological assessments for diagnosing functionally significant coronary artery disease (CAD).
Regarding PCI, the observed growth at the beginning of the 21st century reached a plateau in the last decade. From 2004 to 2008, growth was at 37%, compared to 20% between 2009 and 2013, and a decrease of 0.5% from 2014 to 2023.4 There was a slight reduction in the number of PCI in 2020 due to the lockdown period of the COVID-19 pandemic (−10.6% compared to the year of 2019), explained by the temporary suspension of some elective activities and redeployment of cardiovascular resources to the care of Covid-19 patients. The reduction in PCI is similar to preliminary results from the ESC Atlas project, which reported a median PCI change of −9.0% between 2019 and 2020 across 31 ESC members.6
In the subsequent years, the total number of PCI were similar to numbers from 2014.
Similarly to the COURAGE8 study published in 2007, the ISCHEMIA trial,9 published in 2020, did also not affect the total number of PCIs performed nationwide. However, it may have contributed to the observed reduction in PCIs for chronic coronary syndromes beginning that year and which persisting over the following years. If this reduction were solely attributable to the Covid-19 pandemic, a recovery in the volume of procedures for this specific context would have been expected in the subsequent years; however, this recovery was not observed.
The 1322 PCI per million inhabitants performed in 2023 were similar to 1333 PCI per million inhabitants performed ten years earlier, in 2013. Both figures are markedly lower than the median of 2186 PCI procedures per million inhabitants reported for ESC member countries (IQR 1383–2494) reported in the 2023 ESC Atlas Project,10 as well as Spain, with 1573 PCI per million inhabitants in 2022.7
Data on primary PCI indicate a more attenuated growth in the last decade, a 22% increase from 2014 to 2023, compared to a 62% increase from 2004 to 2013, but still, in 2023, the rate stood at only 374 pPCI per million inhabitants, significantly below the median of 498.5 (IQR 420.2–636.3) pPCI procedures per million inhabitants in ESC member countries as reported by 2023 ESC Atlas survey10; and the target of 600 pPCI per million inhabitants per year recommended by the European Association of Percutaneous Cardiovascular Interventions.11 The figures are close the median of 311.8 (IQR 37.0–650.1) pPCI procedures per million inhabitants observed in middle-income countries, yet remain considerably below the rates in high-income countries (533.7; IQR 429.8–661.0).6 Despite the robust growth over the last 20 years, aligning with trends in Southern European countries, which often report values significantly lower than 600 pPCI per million inhabitants, the rates of pPCI in Portugal remain lower than those reported in Spain, which had 452 per million inhabitants in 2022.7
Despite all the efforts in the last decade, such as community campaign actions and improvement of interinstitutional cooperation, the numbers are still below the European average and those of our neighbor, Spain. This strongly indicates that there are still areas for improvement in the coming years.
Several factors contribute to Portugal's lower rates of pPCI compared to Northern European countries and Spain, including differences in disease prevalence, the availability of healthcare resources, and levels of healthcare literacy among the population. Regional disparities and demographic factors within Portugal, such as urban-rural divides and population density, impact the equitable distribution and accessibility of healthcare services, including primary angioplasty. This report demonstrates these disparities, with the Central region showing lower pPCI rates per million inhabitants. However, these regional asymmetries have diminished over the past decade. The Tagus Valley and Lisbon region, with the highest pPCI rates, reported 473 per million inhabitants in 2014 and 525 per million inhabitants in 2022. The Central region, which had the lowest rate of 178 per million inhabitants in 2014, improved to 296 per million inhabitants in 2022, approaching the Northern region's values. The pPCI numbers in the Central region may improve further in the coming years with the recent opening of a new cath lab in the interior central region (Guarda district) at the beginning of 2024. The Southern region and islands also showed growth from 272 per million inhabitants in 2014 to 392 per million inhabitants in 2022. The improved rates in the Central region may be attributed to the opening of new cath labs, particularly at the Leiria Hospital Center. In the South, population growth due to the influx of non-resident foreigners and tourism may have contributed to the increase in pPCI rates.
Regarding the complex procedures, despite operators having more experience in treating complex disease, the number of procedures involving bifurcations (7.7%), the left main coronary artery (2.8%), chronic occlusions (1.0%), and restenosis (3.7%) has remained low over the years. These low numbers may be underestimated compared to the actual figures due to the potential influence of missing data in the database entries at each local cath lab. This statement is supported by the slightly higher numbers of complex PCI reported in the ESC Atlas in IC survey, although these are still below 10%. While operators are increasingly skilled in managing complex coronary disease, the low percentage of PCIs in complex anatomies, could reflects both strategic decisions in patient care due to anticipated technical challenges and recent scientific data reporting privileging a more conservative approach for stable coronary disease as there are a higher risk associated with procedures in these anatomical settings and a higher risk of target lesion failure on the long-term. This may influence the decision-making process, leading to conservative management approaches or alternative treatment strategies, such as cardiac bypass surgery. On the other hand, the reported low percentages may also be influenced by missing or incomplete data in the RNCI or in the survey, which could underestimate the actual prevalence of these procedures. The level of detail collected in the RNCI may be insufficient to capture specific aspects of procedural complexity, such as PCI in the setting of complex calcified coronary disease or the use of advanced techniques, such as lithotripsy.
Stents remain the primary treatment for obstructive CAD, with DES being increasingly favored in recent years, eliminating conventional bare-metal stents. BVS were utilized in a minority of cases from 2014 to 2017; however, following the publication of the three-year follow-up of ABSORB III trial,12 which highlighted a heightened risk of stent thrombosis with BVS compared to conventional DES, their use was discontinued in 2018.
Registry data do not include information on the utilization of drug-coated balloons. Survey data suggest their occasional use as a substitution for stents, albeit in a limited proportion of cases. Nevertheless, extracting these specifics from the RNCI is challenging.
Regarding other adjunctive coronary intervention devices, the last decade has seen a significant decrease in the use of manual thrombectomy in primary angioplasty, as a result of the findings from the TASTE13,14 and TOTAL15 trials, which found no significant differences in 30-day mortality and major adverse cardiovascular events in the routine use of thrombus aspiration before PCI as compared with PCI alone. Additionally, the TOTAL trial even indicated an increased risk of stroke in patients undergoing the technique.15 These results led to a revision of clinical guidelines. Currently, routine use of thrombus aspiration is not recommended and the technique should be reserved for specific cases, such as in situations with large amounts of visible thrombus.16
The use of image-guided angioplasty has slightly increased over the past decade, though it remains lower than in Spain, where imaging techniques (IVUS and OCT) were used in 14.7% of PCIs in 2022.17 The use of physiology has also gradually increased over the years; however, in the past year, it showed no growth, in contrast to Spain, where the use of physiology rose by 6.3% in 2022 compared to 2021.17 Despite the increasing body of evidence supporting the use of imaging and physiological assessments to guide PCI, several barriers continue to hinder the widespread adoption of these technologies in national cath labs. A significant barrier is the perception of time constraints; integrating intravascular imaging or physiological assessments may prolong the duration of interventions, thereby potentially reducing the number of procedures that can be performed within a given timeframe. Additionally, the lack of adequate training or expertise and the associated costs of these technologies further hinders their adoption. To enhance the utilization of these cost-benefit devices, there is a need to integrate them into cath lab workflows and to provide education to healthcare professionals of all categories.
Regarding vascular access for PCI, the radial approach has gained prominence over the past decade, becoming the preferred access route for most procedures.18 This shift coincided with a decline in the use of femoral access. In the last decade, randomized studies that compared radial access with femoral access, such as the RIVAL,19 RIFLE-STEACS20 and MATRIX21 trials, have reinforced the importance of prioritizing radial access as the default approach, as it is considered safer with a lower risk of vascular and hemorrhagic complications and hard end points during follow-up.
ConclusionThe RNCI achieved robustness in the data on intervention procedures, but there is still room for improvement regarding the data on diagnostic procedures and complex angioplasty, including the use of adjuntive devices to diagnose and treat coronary disese.
In the last 10 years, IC reached a plateau in terms of the number of PCIs performed per year. In contrast, there has been a steady increase in primary PCI and a reduction in geographical asymmetries, although it remains below the median of European countries. In several instances, national IC has followed clinical evidence, with increased utilization of radial access and DES, and a reduced use of manual thrombectomy in primary angioplasty. In other fields, such as intravascular imaging and physiology, there is potential for improvement in the following years.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
We would like to thank Maria Fátima Loureiro, who was the biostatistician at the National Center for Data Collection in Cardiology (CNCDC) at the time of the study, for her collaboration in processing the data from the Portuguese National Registry of Interventional Cardiology. Additionally, we extend our gratitude to all healthcare professionals who diligently record data in the registry at their respective centers.