Percutaneous coronary intervention (PCI) is increasingly used as a treatment option for unprotected left main coronary artery (ULMCA) lesions. We aimed to evaluate the long-term outcome of patients undergoing ULMCA PCI.
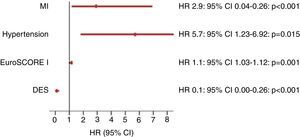
Methods and ResultsWe retrospectively analyzed 95 consecutive patients (median EuroSCORE I 2.9 [IQR 1.4;6.1]) who underwent ULMCA PCI between 1999 and 2006, included in a single-center prospective registry. The primary outcome was major adverse cardiovascular events (MACE) defined as all-cause death, myocardial infarction (MI) and target lesion revascularization (TLR) at five years. Forty patients (42.1%) were treated in the setting of acute coronary syndrome and 81 patients (85%) had at least one additional significant lesion (SYNTAX score 24.2±11.8). Single ULMCA PCI was performed in 33% (81.1% with drug-eluting stents) and complete functional revascularization was achieved in 79% of the patients. During the observation period, 20 patients died (21.1%), 6 (6.3%) had MI and 11 (11.6%) had TLR (total combined MACE 28.4%). Independent predictors of MACE were previous MI (HR 2.9 95% CI 1.23–6.92; p=0.015), hypertension (HR 5.7 95% CI 1.86–17.47; p=0.002) and the EuroSCORE I (HR 1.1 95% CI 1.03–1.12; p=0.001). Drug-eluting stent implantation was associated with a significantly lower MACE rate, even after propensity score adjustment (AUC=0.84; HR [corrected] 0.1; 95% CI 0.04–0.26; p<0.001).
ConclusionsUnprotected left main percutaneous coronary intervention, particularly using drug-eluting stents, can be considered a valid alternative to coronary artery bypass grafting, especially in high-risk surgical patients and with favorable anatomic features.
A intervenção coronária percutânea (ICP) tem sido cada vez mais adotada como uma opção terapêutica para as lesões do tronco comum não protegido (TCNP). O objetivo deste trabalho foi avaliar o prognóstico a longo-prazo de doentes submetidos a ICP do TCNP.
Métodos e resultadosAnálise retrospetiva de 95 doentes consecutivos (mediana do EuroSCORE-I 2.9 [IQR 1.4;6.1]) submetidos a ICP do TCNP entre 1999 e 2006, incluídos num registo prospetivo de centro único. O objetivo primário estudado foi a ocorrência combinada de morte de qualquer causa, enfarte agudo do miocárdio (EAM) e revascularização da lesão alvo (TLR) aos cinco anos de seguimento. Quarenta doentes (42,1%) foram tratados no contexto de uma síndroma coronária aguda e 81 doentes (85%) tinham pelo menos outra lesão significativa adicional (SYNTAX score 24,2±11,8). Angioplastia isolada do tronco comum foi efetuada em 33% dos casos (81,1% com stents revestidos por fármaco) e a revascularização foi funcionalmente completa em 79%. Durante o período estudado, 20 doentes morreram (21,1%), 6 (6,3%) tiveram EAM e 11 (11,6%) TLR (MACE total combinado 28,4%). Os preditores independentes de MACE foram: antecedentes de EAM (HR 2,9 IC95% 1,23-6,92; p=0,015), hipertensão arterial (HR 5,7 IC95% 1,86-17,47; p=0,002) e o EuroSCORE-I (HR 1,1 IC95% 1,03-1,12; p=0,001). A implantação de stent revestido por fármaco associou-se significativamente a menor taxa de MACE, mesmo após ajuste por propensity score (AUC=0,84): HR [corrigido] 0,1; IC95% 0,04-0,26; p < 0,001).
ConclusõesA intervenção coronária percutânea em lesões do tronco comum não protegido, utilizando principalmente stents revestidos por fármaco, pode ser considerada uma alternativa válida à revascularização cirúrgica, em especial em doentes de elevado risco cirúrgico e com características angiográficas favoráveis.
Coronary artery bypass grafting (CABG) is still the standard recommended treatment for unprotected left main coronary artery (ULMCA) lesions.1 Technical improvements in percutaneous intervention (PCI) and stent technology mean that it is increasingly considered as a treatment option for this high-risk patient subset.2 Several registries and randomized clinical trials have shown that percutaneous revascularization of ULMCA lesions is safe and effective, yielding results that are comparable to CABG, particularly when hard clinical endpoints are considered. In the PRECOMBAT study, PCI with sirolimus-eluting stents was non-inferior to CABG with respect to the primary composite endpoint of major adverse cardiac or cerebrovascular events at one year.3 In the subset of 705 patients with left main (LM) lesions (13% isolated LM) included in the randomized SYNTAX trial, all-cause death, cardiac death, myocardial infarction (MI) and the composite endpoint of all-cause death, stroke or MI were similar with both treatment strategies (PCI with first-generation paclitaxel-eluting stents vs. CABG) at four years, despite a significantly higher rate of repeat revascularization in the PCI group (23.5% vs. 14.6%; p=0.003), and a higher rate of stroke in patients randomized to CABG (14.6% vs. 4.3%; p=0.03). The overall results of the trial show that the majority of events occurred in patients with higher SYNTAX scores.4 Likewise, in the five-year outcome analysis of the MAIN-COMPARE registry, stenting resulted in similar rates of death and of the composite endpoint of death, Q-wave MI or stroke, but higher rates of target vessel revascularization were observed compared to CABG.5 The evidence thus suggests that PCI is a reasonable treatment alternative for this subset of coronary artery disease patients, although at the cost of a higher rate of target lesion revascularization.
Our aim was to evaluate and report the long-term (five-year) outcome of patients undergoing PCI of ULMCA disease in a high-volume PCI center.
MethodsStudy populationBetween January 1999 and December 2006, 8832 PCI procedures were undertaken at our institution. Of these, 95 (∼1%) had significant ULMCA luminal stenosis (defined as ≥50% diameter stenosis in the absence of patent grafts to the left anterior descending or circumflex artery) that was treated with stent implantation. In our institution all patients with ULMCA are candidates for surgical revascularization, except for emergent revascularization indicated by the clinical setting, refusal by the surgical team due to unacceptable surgical risk or patient preference. All patients were informed of the procedural risks and alternative treatments methods and subsequently provided written informed consent, unless unable to do so due to their clinical status.
Patients were included in the single-center Angiography and Coronary Revascularization Registry of Santa Cruz Hospital (ACROSS Registry), in which demographic, clinical, angiographic and procedure-related variables are prospectively collected using a dedicated lab-based computer database.
Revascularization proceduresAll patients underwent PCI with stent implantation using standard interventional techniques, according to the specific anatomic features in each case, and the type of stent used was at the physician's discretion. Antiplatelet therapy and periprocedural anticoagulation followed standard recommended regimens. After PCI, aspirin (100–150 mg once daily) was continued indefinitely. Clopidogrel (75 mg once daily) was prescribed for at least 12 months if the procedure was performed in the setting of an acute coronary syndrome. In stable patients, clopidogrel was recommended for at least one month after bare-metal stent implantation and for at least 12 months in patients treated with drug-eluting stents (DES). Treatment beyond this period was at the discretion of the physician. Overall, dual antiplatelet therapy was continued beyond 12 months in 44.4% of cases.
DefinitionsULMCA disease was defined as stenosis in the LM of at least 50% by visual assessment or left main equivalent (defined as >50% stenosis of the ostium of the left anterior descending artery or the left circumflex artery) and if there were no patent bypass grafts to the left anterior descending artery or left circumflex artery. Procedural success was defined as post-procedure TIMI grade 3 flow and residual stenosis <30%; clinical success of the intervention was defined as freedom from death or need for urgent revascularization within 24 hours of the index PCI. MI was adjudicated according to the universal definition of MI.6 Target lesion revascularization was defined as any repeat revascularization (PCI or CABG) for restenosis inside the implanted stent or within 5 mm distal or proximal to the stent edges. Chronic renal disease was defined as an estimated glomerular filtration rate <60 ml/min/1.73 m2.
EndpointsThe primary endpoint of the study was the occurrence of major adverse cardiovascular events (MACE), defined as all-cause death, any MI or any LM TLR within five years of the index PCI, whichever came first. Individual components of MACE were also analyzed and reported separately as secondary endpoints. Follow-up was performed by review of patients’ medical records and telephone interview and was available for the entire 95-patient cohort. Angiographic follow-up was not mandatory and was decided individually according to the physician's choice and the patient's clinical status. Elective control coronary angiography was performed within 6–9 months after the index PCI in 46.7% of cases.
Statistical analysisContinuous variables with normal distribution were expressed as mean and standard deviation. Normality was tested with the Kolmogorov-Smirnov test. Discrete variables were expressed as frequencies and percentages. Statistical comparison of baseline characteristics and outcomes was performed using the chi-square test or Fisher's exact test, as appropriate, for categorical variables and the Student's t test or the Mann-Whitney test for continuous variables. All the analyses were retrospective. Corrected risk estimates and identification of independent predictors of MACE were performed using a Cox proportional hazard regression model, including as covariates variables found to differ significantly in univariate analysis between patients with and without events. In order to minimize the effect of potential selection bias for implantation of DES, we used a propensity score-based correction by including the propensity variable in the regression model. The propensity model calibration was assessed by the Hosmer-Lemeshow goodness-of-fit test and receiver operating characteristic curve analysis (c-statistic). Two-tailed tests of significance are reported. For all comparisons, a p value of <0.05 was considered statistically significant. When appropriate, 95% confidence intervals were calculated. The statistical analysis was performed with SPSS™ version 19.0 (SPSS Inc., Chicago, Ill, USA).
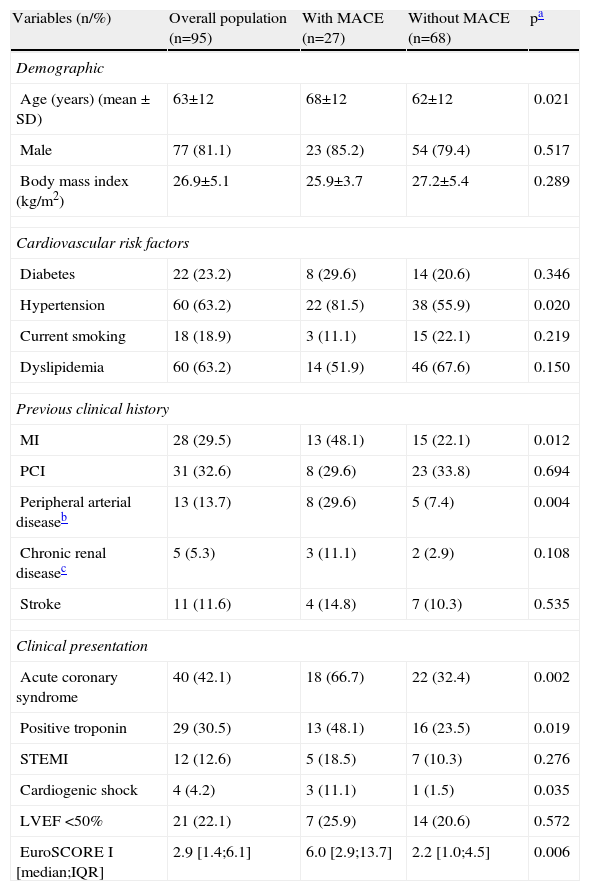
ResultsPopulation characteristics and clinical settingDuring the study period, a total of 95 patients underwent unprotected LMCA PCI. Baseline patient characteristics are summarized in Table 1. Briefly, mean age was 63±12 years (18.9% older than 75) and most were male (81%); there was a high prevalence of traditional cardiovascular risk factors and clinically overt cardiovascular disease, 29.5% with a previous history of MI and 39% with a previous revascularization procedure. Forty patients (42.1%) were treated in the setting of an acute coronary syndrome, 12 of them with ST-elevation MI. Overall, four patients had cardiogenic shock at presentation. Compared to patients that were free from MACE at five years|, patients in whom the primary endpoint occurred were older and had a higher prevalence of hypertension, peripheral arterial disease and previous MI. At presentation, patients with any MACE at five years were more likely to be enrolled in the context of an acute coronary syndrome, MI and cardiogenic shock.
Baseline characteristics of the total population and of patients with and without study-defined major adverse cardiovascular events.
| Variables (n/%) | Overall population (n=95) | With MACE (n=27) | Without MACE (n=68) | pa |
| Demographic | ||||
| Age (years) (mean ± SD) | 63±12 | 68±12 | 62±12 | 0.021 |
| Male | 77 (81.1) | 23 (85.2) | 54 (79.4) | 0.517 |
| Body mass index (kg/m2) | 26.9±5.1 | 25.9±3.7 | 27.2±5.4 | 0.289 |
| Cardiovascular risk factors | ||||
| Diabetes | 22 (23.2) | 8 (29.6) | 14 (20.6) | 0.346 |
| Hypertension | 60 (63.2) | 22 (81.5) | 38 (55.9) | 0.020 |
| Current smoking | 18 (18.9) | 3 (11.1) | 15 (22.1) | 0.219 |
| Dyslipidemia | 60 (63.2) | 14 (51.9) | 46 (67.6) | 0.150 |
| Previous clinical history | ||||
| MI | 28 (29.5) | 13 (48.1) | 15 (22.1) | 0.012 |
| PCI | 31 (32.6) | 8 (29.6) | 23 (33.8) | 0.694 |
| Peripheral arterial diseaseb | 13 (13.7) | 8 (29.6) | 5 (7.4) | 0.004 |
| Chronic renal diseasec | 5 (5.3) | 3 (11.1) | 2 (2.9) | 0.108 |
| Stroke | 11 (11.6) | 4 (14.8) | 7 (10.3) | 0.535 |
| Clinical presentation | ||||
| Acute coronary syndrome | 40 (42.1) | 18 (66.7) | 22 (32.4) | 0.002 |
| Positive troponin | 29 (30.5) | 13 (48.1) | 16 (23.5) | 0.019 |
| STEMI | 12 (12.6) | 5 (18.5) | 7 (10.3) | 0.276 |
| Cardiogenic shock | 4 (4.2) | 3 (11.1) | 1 (1.5) | 0.035 |
| LVEF <50% | 21 (22.1) | 7 (25.9) | 14 (20.6) | 0.572 |
| EuroSCORE I [median;IQR] | 2.9 [1.4;6.1] | 6.0 [2.9;13.7] | 2.2 [1.0;4.5] | 0.006 |
Peripheral arterial disease was defined as symptomatic carotid artery disease or asymptomatic stenosis ≥70%, documented lower limb obstructive atherosclerosis or any ischemic symptoms.
Chronic renal disease was defined as renal replacement therapy, previous kidney transplantation or estimated creatinine clearance ≤30 ml/min. IQR: interquartile range; LVEF: left ventricular ejection fraction; MACE: major adverse cardiovascular events; MI: myocardial infarction; PCI: percutaneous coronary intervention; SD: standard deviation; STEMI: ST-elevation myocardial infarction.
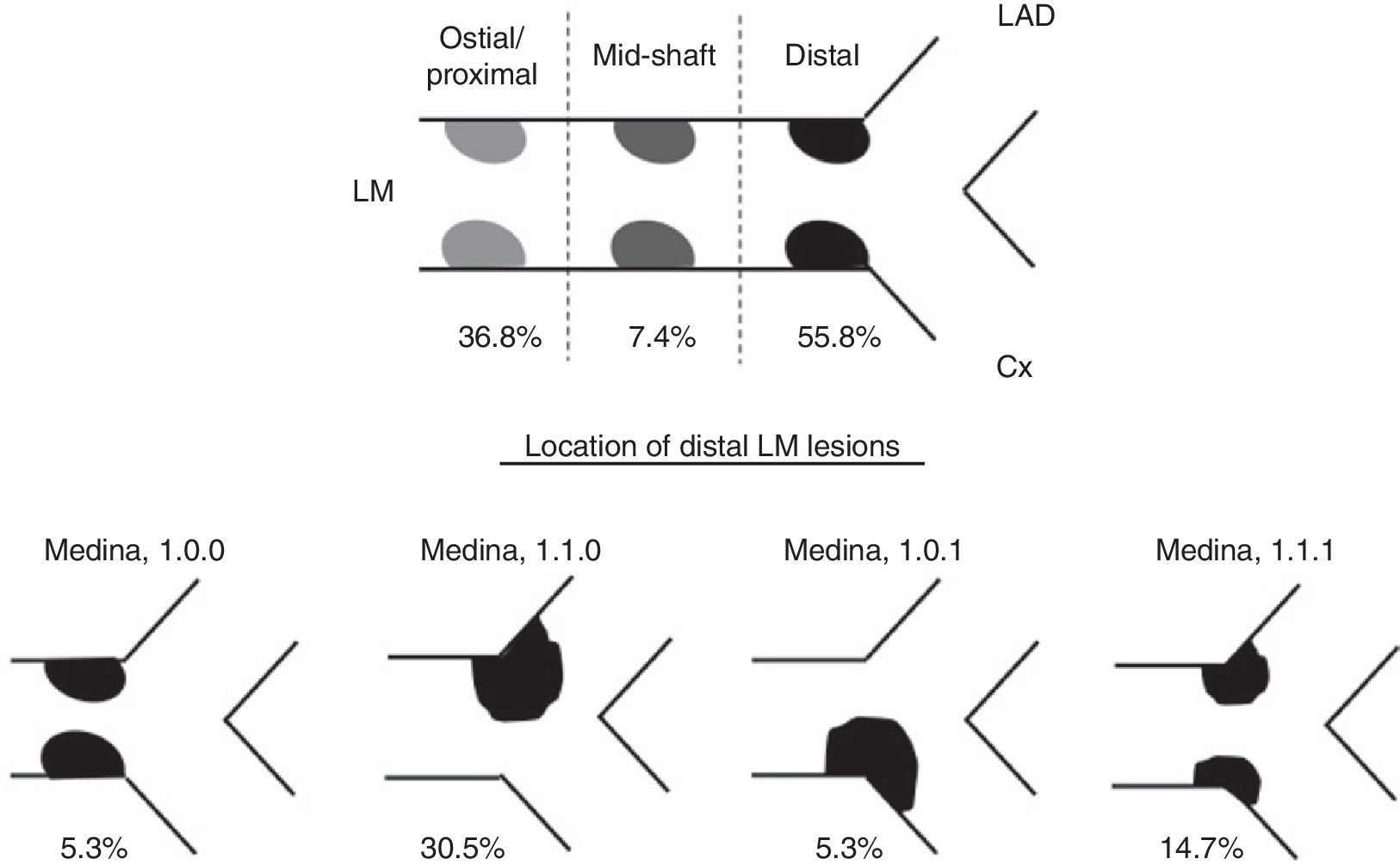
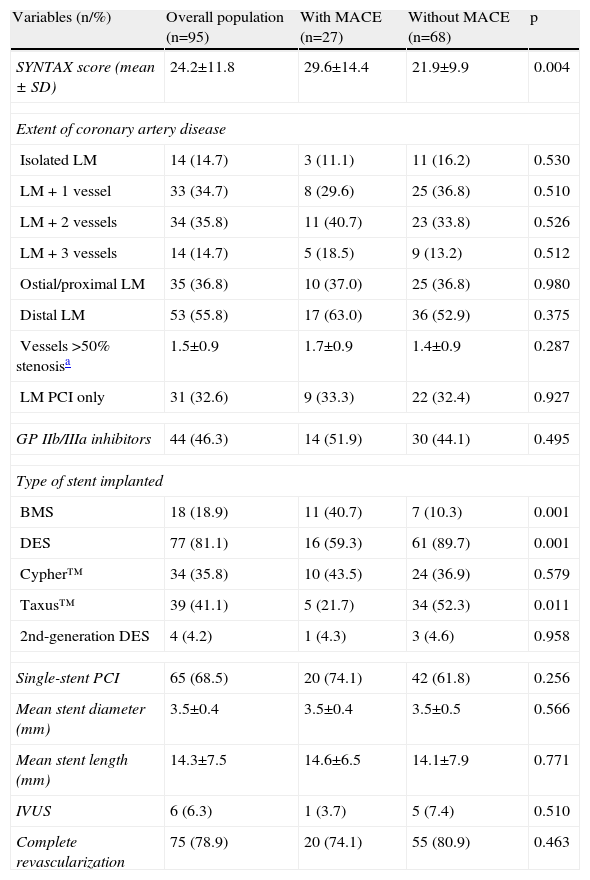
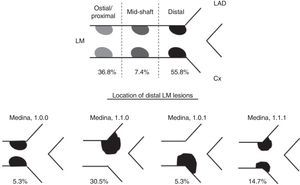
Angiographic and procedural characteristics are shown in Table 2. Only a small proportion of patients had isolated LM disease (14.7%) and mean SYNTAX score was 24.2±11.8. The anatomic features of LM disease are described in detail in Figure 1; 55.8% were distal LM lesions, most with ostial/proximal left anterior descending coronary artery involvement (Medina classification 1-1-0). Overall, a single-stent strategy was employed in 68.5% of the procedures and in approximately one-third of cases only the LM was treated. The implantation of a DES was the most frequent choice (81.1%), mostly using the Taxus™ stent (50.6% of overall DES). In nearly half of the patients (40.6%), glycoprotein IIb/IIIa inhibitors were administered during the procedure. PCI was guided by intravascular ultrasound in six cases (6.3% of the overall cohort), five of them in the group without MACE, although the difference was not statistically significant.
Angiographic and procedural characteristics.
| Variables (n/%) | Overall population (n=95) | With MACE (n=27) | Without MACE (n=68) | p |
| SYNTAX score (mean ± SD) | 24.2±11.8 | 29.6±14.4 | 21.9±9.9 | 0.004 |
| Extent of coronary artery disease | ||||
| Isolated LM | 14 (14.7) | 3 (11.1) | 11 (16.2) | 0.530 |
| LM + 1 vessel | 33 (34.7) | 8 (29.6) | 25 (36.8) | 0.510 |
| LM + 2 vessels | 34 (35.8) | 11 (40.7) | 23 (33.8) | 0.526 |
| LM + 3 vessels | 14 (14.7) | 5 (18.5) | 9 (13.2) | 0.512 |
| Ostial/proximal LM | 35 (36.8) | 10 (37.0) | 25 (36.8) | 0.980 |
| Distal LM | 53 (55.8) | 17 (63.0) | 36 (52.9) | 0.375 |
| Vessels >50% stenosisa | 1.5±0.9 | 1.7±0.9 | 1.4±0.9 | 0.287 |
| LM PCI only | 31 (32.6) | 9 (33.3) | 22 (32.4) | 0.927 |
| GP IIb/IIIa inhibitors | 44 (46.3) | 14 (51.9) | 30 (44.1) | 0.495 |
| Type of stent implanted | ||||
| BMS | 18 (18.9) | 11 (40.7) | 7 (10.3) | 0.001 |
| DES | 77 (81.1) | 16 (59.3) | 61 (89.7) | 0.001 |
| Cypher™ | 34 (35.8) | 10 (43.5) | 24 (36.9) | 0.579 |
| Taxus™ | 39 (41.1) | 5 (21.7) | 34 (52.3) | 0.011 |
| 2nd-generation DES | 4 (4.2) | 1 (4.3) | 3 (4.6) | 0.958 |
| Single-stent PCI | 65 (68.5) | 20 (74.1) | 42 (61.8) | 0.256 |
| Mean stent diameter (mm) | 3.5±0.4 | 3.5±0.4 | 3.5±0.5 | 0.566 |
| Mean stent length (mm) | 14.3±7.5 | 14.6±6.5 | 14.1±7.9 | 0.771 |
| IVUS | 6 (6.3) | 1 (3.7) | 5 (7.4) | 0.510 |
| Complete revascularization | 75 (78.9) | 20 (74.1) | 55 (80.9) | 0.463 |
BMS: bare-metal stent; DES: drug-eluting stent; GP: glycoprotein; IVUS: intravascular ultrasound; LM: left main; PCI: percutaneous coronary intervention; SD: standard deviation.
Importantly, patients in whom major events occurred had a higher SYNTAX score and were less often treated with DES, mainly with first-generation paclitaxel-eluting stents (Table 2).
Procedural success was 100% and protocol-defined clinical success was 96.8%. Three deaths occurred within the 24-hour post-procedure period, all in patients with an acute coronary syndrome at presentation, two of whom presented with cardiogenic shock. Total in-hospital mortality was entirely attributable to these three deaths (3.2% of the overall cohort).
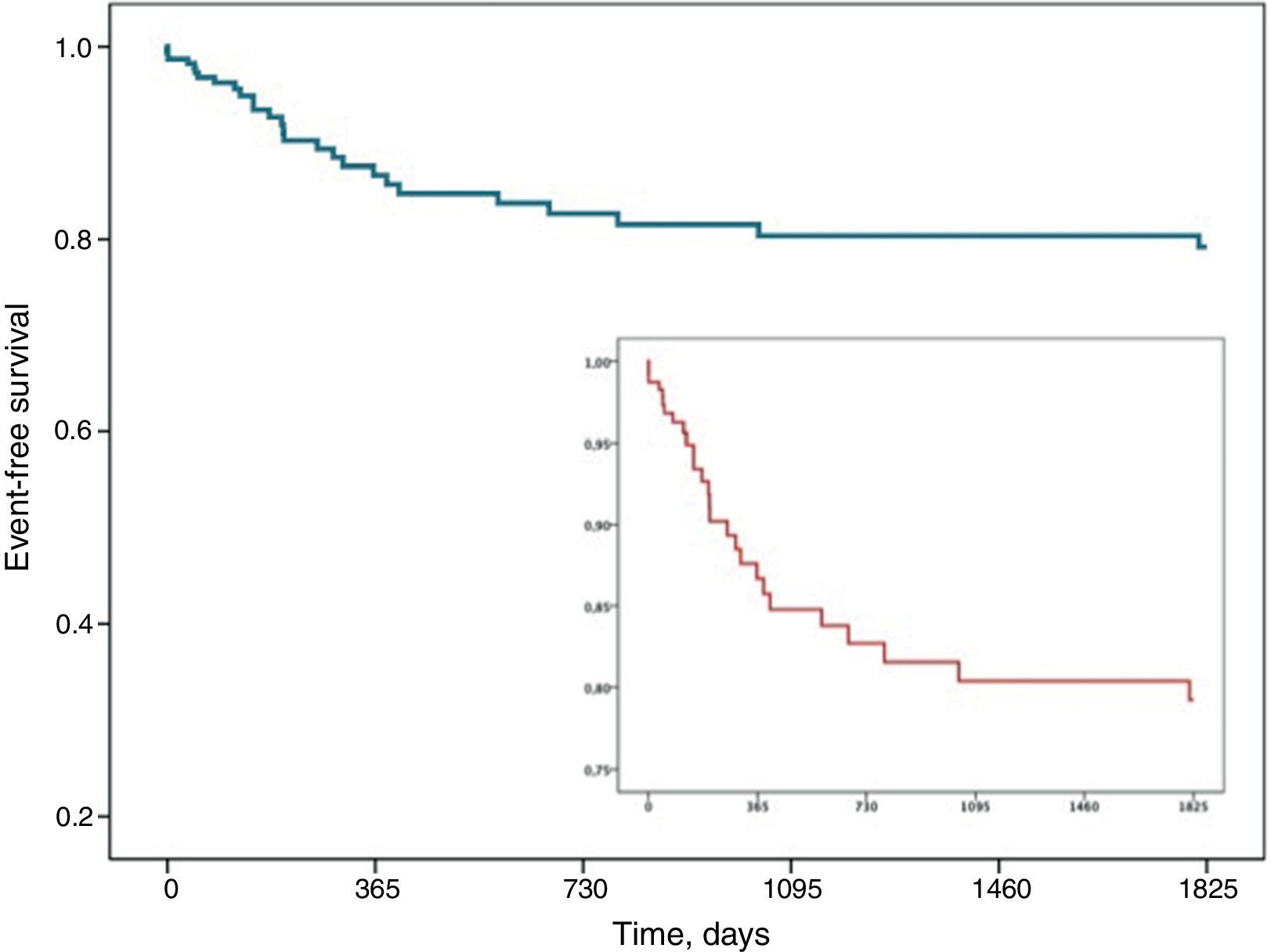
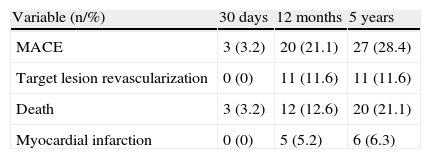
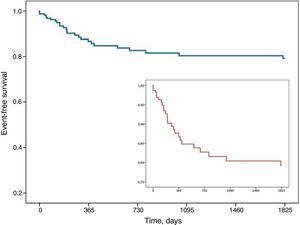
Primary and secondary endpoint analysisDuring the five-year observation period (which was available for all 95 patients), the cumulative MACE rate was 28.4%: 20 patients died (21.1%), six had new MI (6.3%) and 11 needed repeat LM TLR (11.6%). Most of the events occurred within a year of the index PCI, the median time between the procedure and the occurrence of any MACE being 200 (IQR 54;385) days (Figure 2). The distribution of the study endpoints at 30 days, 12 months and five years is represented in Table 3. Thirty-day mortality was numerically lower and compared favorably to the EuroSCORE I-predicted fatality rate: 3.2% vs. 6.0% (p=NS).
Cumulative distribution of the study endpoints at different time points during the five-year follow-up period.
| Variable (n/%) | 30 days | 12 months | 5 years |
| MACE | 3 (3.2) | 20 (21.1) | 27 (28.4) |
| Target lesion revascularization | 0 (0) | 11 (11.6) | 11 (11.6) |
| Death | 3 (3.2) | 12 (12.6) | 20 (21.1) |
| Myocardial infarction | 0 (0) | 5 (5.2) | 6 (6.3) |
MACE: major adverse cardiovascular events (all-cause death, recurrent myocardial infarction or left main target lesion revascularization).
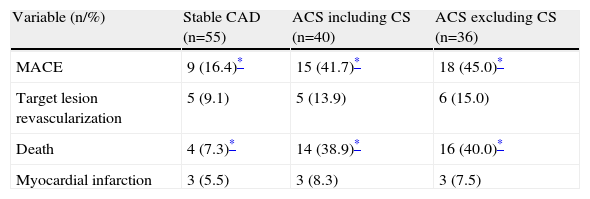
Given the high proportion of acute coronary syndromes, including a 12.6% prevalence of ST-elevation MI, in the overall population and considering the potential impact of this adverse clinical setting on outcome, we performed a separate analysis of MACE and its individual components in this patient subgroup. The results are summarized in Table 4.
Cumulative distribution of the study endpoints according to clinical presentation at five-year follow-up.
| Variable (n/%) | Stable CAD (n=55) | ACS including CS (n=40) | ACS excluding CS (n=36) |
| MACE | 9 (16.4)* | 15 (41.7)* | 18 (45.0)* |
| Target lesion revascularization | 5 (9.1) | 5 (13.9) | 6 (15.0) |
| Death | 4 (7.3)* | 14 (38.9)* | 16 (40.0)* |
| Myocardial infarction | 3 (5.5) | 3 (8.3) | 3 (7.5) |
ACS: acute coronary syndrome; CAD: coronary artery disease; CS: cardiogenic shock; MACE: major adverse cardiovascular events (all-cause death, recurrent myocardial infarction or left main target lesion revascularization).
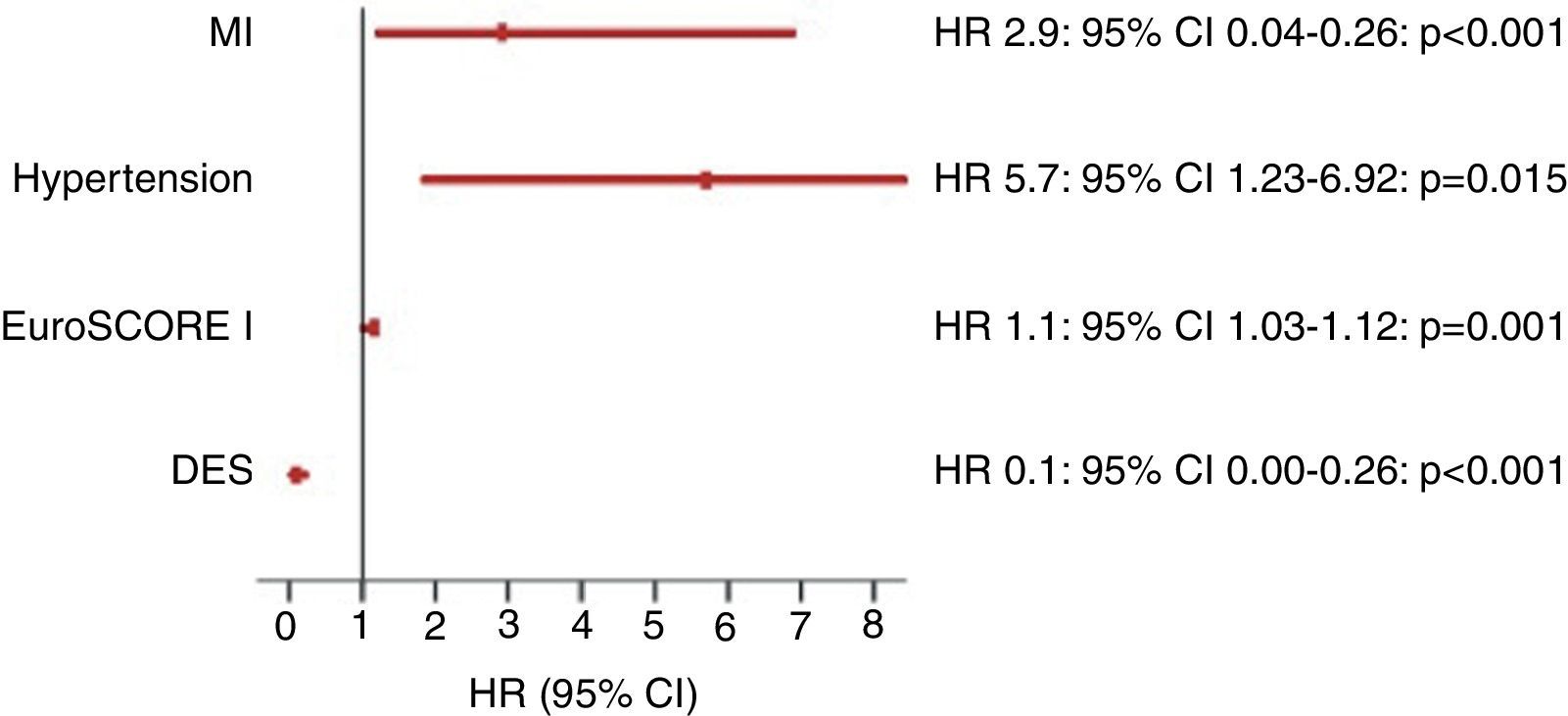
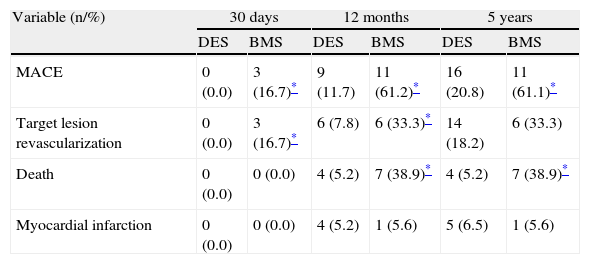
In the multivariate Cox regression model, the independent predictors of MACE at five years were EuroSCORE I, hypertension and a previous history of MI (Figure 3). Implantation of DES was associated with a significantly lower total MACE rate; the cumulative hazard ratio – after correction for the probability of receiving a DES by including the propensity variable in the regression model (Hosmer-Lemeshow goodness-of-fit: chi-square=11.32; p=0.1; c-statistic=0.83) – was 0.10 (95% CI 0.04–0.26; p<0.001). Table 5 shows the cumulative distribution of the study endpoints according to the type of stent implanted (DES vs. BMS) at different time points during the five-year follow-up period.
Cumulative distribution of the study endpoints according to type of stent implanted at different time points during the five-year follow-up period.
| Variable (n/%) | 30 days | 12 months | 5 years | |||
| DES | BMS | DES | BMS | DES | BMS | |
| MACE | 0 (0.0) | 3 (16.7)* | 9 (11.7) | 11 (61.2)* | 16 (20.8) | 11 (61.1)* |
| Target lesion revascularization | 0 (0.0) | 3 (16.7)* | 6 (7.8) | 6 (33.3)* | 14 (18.2) | 6 (33.3) |
| Death | 0 (0.0) | 0 (0.0) | 4 (5.2) | 7 (38.9)* | 4 (5.2) | 7 (38.9)* |
| Myocardial infarction | 0 (0.0) | 0 (0.0) | 4 (5.2) | 1 (5.6) | 5 (6.5) | 1 (5.6) |
BMS: bare-metal stent; DES: drug-eluting stent; MACE: major adverse cardiovascular events (all-cause death, recurrent myocardial infarction or left main target lesion revascularization).
In this observational study, the long-term prognosis (five years) of patients undergoing PCI of a ULMCA was reported. Both acute procedural and clinical success rates were high, indicating that the strategy is safe and effective when performed by experienced interventional cardiologists, in this case mostly using drug-eluting stents and a single-stent technique.
Although the choice of PCI strategy was at the operator's discretion, a single stent was used in nearly 70% of cases. In our study, more than half of the patients had distal LM involvement, with Medina classification 1.1.0 and 1.1.1 being the most prevalent disease patterns (Figure 1). This finding is consistent with data from previous trials and registries, including the SYNTAX trial.4,7 Evidence from early trials suggested that the outcome of patients treated for distal LM disease was worse than for those with aorto-ostial or mid-shaft lesions.8 However, subsequent studies have failed to demonstrate the superiority of a systematic double-stent approach to distal LM PCI.9,10
Total MACE rates in our cohort were within the range of those previously reported in randomized trials and registries.4,5 It should be noted that total mortality was higher and TLR was relatively low, especially considering the long follow-up period. The high mortality rate was most likely related to the overall worse clinical profile of the patients included in our analysis. Compared to the MAIN-COMPARE registry,5 our population was older and had higher rates of previous MI and chronic renal disease and more extensive coronary artery disease and, importantly, patients with ST-elevation MI and cardiogenic shock were not excluded. In our cohort, the proportion of troponin-positive acute coronary syndromes was ∼71%, compared to ∼8–9% of non-ST-elevation MI patients in the MAIN-COMPARE registry. The finding that early mortality was comparable to the EuroSCORE-predicted fatality rate at 30 days reinforces the observation that long-term mortality was most likely related to patient characteristics, rather than to procedure-related issues. When patients with cardiogenic shock were excluded from the analysis, mortality was 19.8% and when only troponin-negative (i.e., stable coronary artery disease and unstable angina) patients were included, mortality was 13.6%, which is comparable to similar published trials and registries.
On the other hand, in comparison to the PCI arm of the SYNTAX trial (23.5% at four years)4 and to the MAIN-COMPARE registry (16% at five years),5 TLR in our study was less frequent and occurred mostly during the first year after the index procedure, despite the low use of intravascular ultrasound-guided PCI. This is consistent with the fact that the mean SYNTAX score observed in our cohort was lower than that reported in the left main subset of PCI-treated patients of the SYNTAX trial (24.2±11.8 vs. 28.1±12.4),4 as well as with the high proportion of DES used. In addition, the low rate of systematic elective angiography during follow-up could provide further explanation for these observations: not only could cases of angiographic restenosis have been missed, but undiagnosed restenosis could actually have been responsible for some cases of cardiac death. Previous studies have suggested that cardiac death can be a manifestation of restenosis after LM PCI11,12 and indeed, in our study, total MACE and mortality rates were higher in BMS- than in DES-treated patients. Of the 11 TLR events, at least five were clinically driven (two of them non-ST-elevation MI), while three followed elective control angiography in asymptomatic patients. For the remaining three, revascularization details were not available, but vital status was known. In our view, these findings may argue in favor of routine follow-up angiography, as significant restenosis presented as an acute coronary syndrome in at least 18% of cases, at best.
The independent predictors of MACE at five years in our cohort – hypertension, previous MI and EuroSCORE I – have all been shown to be associated with worse prognosis in the setting of coronary disease. Elderly patients receiving ULMCA PCI are at high risk for major adverse events following the procedure.13 However, this was not evident in our study, possibly because important unmeasured comorbidity and the EuroSCORE offset the effect of age in the prediction model.
The implantation of DES was statistically associated with a highly significant lower MACE rate. Several studies have reported the survival benefit of ULMCA revascularization with DES, but the mechanism by which stent type affects the risk of death remains unclear.13,14 Palmerini et al. showed that DES use was associated with a significant decrease in adjusted two-year cardiac mortality rates, compared to patients treated with BMS.9 In our population the association between DES and lower mortality alone was consistently stronger than with reduced TLR. Notwithstanding the possibility, discussed above, that some cases of restenosis (more frequent in BMS-treated patients) may have presented clinically as fatal events, it cannot be firmly excluded that this observation is a spurious statistical association driven by the fact that fatal events (n=20) occurred more often than TLR events (n=11) and that a treatment bias is still present, despite adequate corrections and the good fitness of the regression model for the propensity variable (c-statistic=0.83).
LM disease is present in 3–10% of patients undergoing coronary angiography and is associated with high mortality. Despite the upgrade in the recommendation for PCI of ULMCA lesions, this strategy is usually reserved for patients with high burden of comorbidities and frequently for severely ill patients (under resuscitation and/or in cardiogenic shock), in whom surgical revascularization cannot be carried out with an acceptable risk.
In patients presenting with acute coronary syndromes, ULMCA lesions are associated with high mortality, especially in the setting of ST-elevation MI and/or hemodynamic or arrhythmic instability. For these, PCI may be the preferred revascularization strategy, being feasible and yielding reasonable outcomes.15,16
Technological improvements in interventional techniques, particularly the widespread use and availability of DES (which decrease stent restenosis and need for repeat revascularization), the development of both percutaneous and pharmacological adjunctive therapies such as thrombus aspiration and antiplatelet or anticoagulant therapy is contributing to increasingly consistent and satisfactory results.15,16 Nevertheless, and despite significant geographical variability, fewer than 5% of patients with significant ULMCA lesions are percutaneously treated, as shown by the CathPCI Registry.3 In the multinational all-comers DELTA registry,17 no difference was observed in the occurrence of death, cerebrovascular accidents, and MI between PCI with first-generation drug-eluting stents and CABG at a median follow-up of 3.5 years.
Another feasible alternative for the treatment of ULMCA lesions is hybrid coronary revascularization. Combining the advantages of the long-term durability of a left internal mammary artery-left anterior descending bypass with the less invasive option of PCI for lesions in other coronary arteries may reduce the possible complications of the two interventions in isolation.9
In view of the complexity of LM lesions, certain strategies can help improve both acute angiographic and long-term clinical success: performance of PCI in high-volume centers by operators with expertise in the management of complex anatomic lesions; routine use of intravascular ultrasound for procedural guidance, as it provides accurate assessment of lesion severity and can confirm optimal stent expansion and apposition; hemodynamic support, when appropriate; implantation of newer DES, which reduce stent thrombosis and restenosis; implantation of a single stent whenever possible; emphasis on compliance with dual antiplatelet therapy, especially after DES implantation; application of clinical and angiographic risk models such as the SYNTAX score to facilitate an individualized approach for each patient; and encouragement of collaborative and multidisciplinary discussion and patient selection within the “heart team”, which is crucial for clinical decision-making.18 Ongoing randomized trials such as NOBLE (Nordic-Baltic-British Left Main Revascularization) and EXCEL (Evaluation of Xience Prime Versus Coronary Artery Bypass Surgery for Effectiveness of Left Main Revascularization) will bring further insight into treatment options for ULMCA stenosis using contemporary devices and surgical techniques.
The present study has some limitations, among which we highlight those inherent to a retrospective non-randomized design and to the small number of patients included. Unknown confounders might have affected the results (despite the appropriate statistical adjustments) and the small population size renders the study underpowered to detect significant differences in outcome according to important baseline characteristics. Finally, some of the procedural characteristics, mainly those related to the PCI technique itself, were at the operator's discretion, making standardization difficult and assessment of the potential impact of the PCI strategy on outcome virtually impossible.
In conclusion, in this high-risk population, ULMCA PCI was safe and effective. Although the five-year event rate (especially mortality) was high (reflecting poor patient clinical status), early mortality compared favorably to the EuroSCORE I-predicted 30-day mortality. Overall, long-term clinical results are acceptable, and thus this strategy may be considered a valid alternative to CABG. The high rate of MACE in the first year, especially in BMS-treated patients, suggests the need for routine control angiography in all patients in whom a BMS is implanted, and whenever possible, that a DES should be used as first choice.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.