Coronary artery disease is the leading cause of mortality worldwide. Regular physical activity is part of a comprehensive management strategy for these patients. We investigated the parameters that influence physical activity in patients with a history of coronary revascularization.
MethodsWe included outpatients with a history of coronary revascularization at least six months prior to enrollment. Data on physical activity, demographics, and clinical characteristics were collected via a questionnaire.
ResultsA total of 202 consecutive outpatients (age 61.3±11.2 years, 73% male) were enrolled. One hundred and four (51%) patients had previous percutaneous coronary intervention, 67 (33%) had coronary bypass graft surgery, and 31 (15%) had both procedures. Only 46 patients (23%) engaged in regular physical activity. Patients were classified into two subgroups according to their physical activity. There were no significant differences between subgroups in terms of age, comorbid conditions or revascularization type. Multivariate regression analysis revealed that low education level (OR=3.26, 95% CI: 1.31-8.11, p=0.01), and lack of regular follow-up (OR=2.95, 95% CI: 1.01-8.61, p=0.04) were independent predictors of non-adherence to regular physical activity among study subjects.
ConclusionsRegular exercise rates were lower in outpatients with previous coronary revascularization. Education level and regular follow-up visits were associated with adherence to physical activity in these patients.
A doença coronária é a principal causa de mortalidade em todo o mundo. A atividade física regular constitui o suporte de uma estratégia de gestão abrangente para estes doentes. Investigamos os parâmetros que influenciam a atividade física nos doentes com história de revascularização coronária.
MétodosIncluímos doentes de ambulatório com história de revascularização coronária pelo menos seis meses anterior ao registo. Foram recolhidos, através de um questionário, dados sobre os hábitos de atividade física, sobre estatística e características clínicas.
ResultadosFoi registado um total de 202 doentes consecutivos de ambulatório (idade 61,3±11,2 anos, 73% homens). Cento e quatro (51%) doentes foram submetidos a intervenção coronária percutânea anterior, 67 (33%) doentes foram submetidos a cirurgia de revascularização do miocárdio e 31 (15%) foram submetidos a ambos procedimentos. De todos, 46 (23%) doentes praticavam atividade física regular. Os doentes foram classificados em dois subgrupos, de acordo com os seus hábitos de prática de atividade física. Não houve diferenças significativas relativamente à idade, às condições de comorbilidade ou ao tipo de revascularização entre os grupos. Na análise de regressão multivariada, concluiu-se que o baixo nível de instrução (OR=3,26, CI 95%: 1,31-8,11, p=0,01) e a ausência de consultas regulares de seguimento (OR=2,95, CI 95%: 1,01-8,61, p=0,04) foram fatores preditores independentes da não adesão à atividade física regular entre os indivíduos do estudo.
ConclusõesOs índices de atividade física regular foram inferiores nos doentes de ambulatório com revascularização coronária anterior. O nível de instrução e as consultas de seguimento regulares foram associados à adesão à atividade física nestes doentes.
Despite considerable progress in prevention, diagnosis and management strategies, coronary artery disease (CAD) is still the leading cause of death in developed countries.1 Three decades ago, it was believed that physical activity (PA) was hazardous in patients with CAD.2 Today, we know that it is well tolerated and safe, and that even severely symptomatic patients can benefit from exercise.3–5 It is strongly recommended that individuals with stable ischemic heart disease should engage in 30-60 min of moderate intensity aerobic activity on at least five and preferably seven days a week.6 Regular PA decreases neurohumoral activation, reduces sympathetic tone, increases vagal tone and improves myocardial perfusion.7,8 It also increases endothelial nitric oxide (NO) synthase expression and protein phosphorylation, raising nitric oxide levels. Additionally, exercise reduces the expression of inflammatory substances such as interleukin-6, interferon-gamma and toll-like receptor (TLR), as well as platelet aggregation.9
Clinically, PA helps to regulate blood pressure, control body weight and lipid profile, and decrease insulin resistance.10,11 Studies have shown that the favorable effects of exercise improve anaerobic threshold and aerobic capacity, functional status and quality of life.12 A meta-analysis of 51 randomized controlled trials showed that exercise training reduced the primary composite outcome of all-cause mortality or all-cause hospitalization by 27%.13
As a result of these complementary findings, exercise training has become a standard non-pharmacological treatment modality in the management of cardiovascular diseases.14 In recent European guidelines on cardiovascular disease prevention in clinical practice, regular aerobic exercise is recommended in patients with coronary disease to improve functional capacity and symptoms.15
Despite its widely known favorable effects, regular exercise is not prevalent among patients with CAD. Although there are many studies showing the beneficial effects of PA in primary and secondary prevention of cardiovascular disease, there is little information about patients’ adherence to exercise training and parameters that can improve adherence rates. In this study, we aimed to investigate factors which may influence regular PA in patients with a history of coronary revascularization.
MethodsStudy design and patient selectionThis was a prospective observational cohort study. A total of 202 consecutive outpatients with a history of coronary revascularization at least six months prior to enrollment were included. Patients in unstable condition, with communication difficulties, unwilling to participate, without history of coronary revascularization or with coronary revascularization less than six months prior to enrollment were excluded. The study was approved by the local ethics committee and patients gave their informed consent to participate.
Data collectionPatients’ demographic, social and clinical characteristics and data on PA were collected via a questionnaire designed by the study investigators. All patients were asked whether they performed regular exercise and of what type. The weekly frequency and the daily intensity of the exercise were noted. Patients’ history of CAD, revascularization type and details of the intervention were noted from medical records.
DefinitionsPA was defined as at least 30 minutes of jogging, running, aerobic exercise, cycling or swimming at least twice a week. Hypertension was defined as blood pressure >140/90 mmHg on two occasions during office measurements or use of antihypertensive treatment. Diabetes was defined as fasting blood glucose ≥126 mg/dl on two occasions or use of antidiabetic treatment. Hyperlipidemia was defined as low-density lipoprotein cholesterol >100 mg/dl or use of statins. A family history of CAD was defined as a history of CAD or sudden cardiac death in a first-degree relative before the age of 55 years for men and 65 years for women. Body mass index (BMI) was calculated by dividing weight in kg by height in m squared. A history of acute coronary syndrome was defined by detection of a rise in cardiac troponins together with symptoms of ischemia or ischemic changes on the electrocardiogram (ECG) from past medical records. The presence of atrial fibrillation was also determined from the ECG. Medical records were searched for history of cerebrovascular events. Chronic renal disease was defined as estimated glomerular filtration rate <90 ml/dl/1.73 m2 according to the Chronic Kidney Disease Epidemiology Collaboration formula or being on routine dialysis. Cardiac function was noted from echocardiographic measurement of left ventricular ejection fraction (EF) at least three months after coronary revascularization and heart failure was defined as EF <40%. Patients’ functional status was assessed according to New York Heart Association class. Severity of angina was defined according to the Canadian Cardiovascular Society grading.
Laboratory measurementsBlood samples were obtained from the antecubital vein after a 12-hour fasting period. A Coulter LH series analyzer (Beckman Coulter Inc., Hialeah, FL) was used to obtain a complete blood count. Plasma levels of triglycerides, high-density lipoprotein, low-density lipoprotein, glucose and creatinine were assessed using an automated chemistry analyzer (Abbott Aeroset, USA) using commercially available kits (Abbott, USA).
Statistical analysisSPSS 17.0 for Windows (SPSS Inc., Chicago, IL, USA) was used for the statistical analysis. Continuous variables were expressed as mean ± SD or median with interquartile range, and categorical variables were expressed as percentages and numbers. The chi-square test or Fisher's exact test was used to compare categorical variables. The normality of distributions of the parameters was assessed by the Shapiro-Wilk test. Continuous variables were compared using the independent samples t test for normally distributed variables, and the Mann-Whitney U test when the distribution was skewed. Univariate logistic regression analysis was used to assess the relationship between variables and absence of PA. Variables found to be statistically significant in the univariate analysis were then used in forward stepwise multivariate logistic regression analysis in order to determine independent predictors of absence of PA. The results of the regression analyses were presented as odd ratios (OR) and 95% confidence intervals (CI). A p value <0.05 was considered statistically significant.
ResultsThe mean age of patients who met the inclusion criteria was 61.3±11.2 years, with males comprising 73% of the cohort. Of the total population, 121 (60%) patients had hypertension, 59 (29%) had diabetes, 85 (42%) had previous infarction and 26 (13%) had heart failure; 104 (51%) patients had previous percutaneous coronary intervention (PCI), 67 (33%) had coronary bypass graft surgery (CABG), and 31 (15%) had both revascularization procedures. The median time after coronary artery revascularization was 60 months.
A total of 46 (23%) patients engaged in regular exercise, of which walking (83%, n=42) was the most common PA. Study patients exercised on a median of two days per week, with a median of one hour's exercise on each of these days.
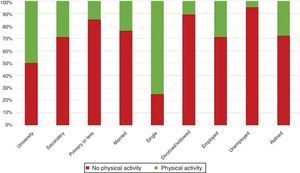
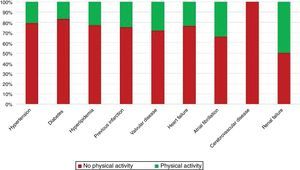
The PA status of the study population and their demographic and anthropometric characteristics are shown in Table 1 and their clinical characteristics, laboratory findings, and medications are summarized in Table 2. Patients’ PA status according to marital status, employment status and education level is shown in Figure 1 and according to comorbidities in Figure 2. There were no significant differences between the groups in terms of age, anthropometric characteristics, comorbidities, functional status, revascularization procedures or medications. Female gender, low education level, unemployment, low household income, implantation of bare-metal stents (vs. drug-eluting stents) and absence of regular follow-up visits were more common in the inactive group.
Demographic and anthropometric parameters of the study population comparing physically active and inactive groups.
| All patients (n=202) | Physical activity | p | ||
|---|---|---|---|---|
| Absent (n=156) | Present (n=46) | |||
| Age (years) | 61.3±11.2 | 61.5±11.2 | 60.6±11 | 0.62 |
| Female | 54 (27%) | 47 (30%) | 7 (15%) | 0.04 |
| BMI (kg/m2) | 26.8 (23.5-29.8) | 27.2 (24.7-30.1) | 26 (24.4-28.6) | 0.15 |
| WC (cm) | 100 (93-108) | 100 (94-108) | 98 (90-105) | 0.14 |
| Education | ||||
| University | 16 (8%) | 8 (5%) | 8 (17%) | 0.01 |
| Secondary | 82 (41%) | 59 (38%) | 23 (50%) | 0.13 |
| Primary or less | 104 (51%) | 89 (57%) | 15 (33%) | 0.004 |
| Marital status | ||||
| Married | 166 (82%) | 127 (81%) | 39 (85%) | 0.59 |
| Single | 4 (2%) | 1 (1%) | 3 (6%) | 0.03 |
| Divorced/widowed | 29 (14%) | 26 (17%) | 3 (6%) | 0.08 |
| Employment status | ||||
| Employed | 45 (22%) | 32 (20%) | 13 (28%) | 0.26 |
| Unemployed | 43 (21%) | 41 (26%) | 2 (4%) | 0.001 |
| Retired | 114 (56%) | 83 (53%) | 31 (67%) | 0.08 |
| Household income | ||||
| Low (<1000 TRY) | 92 (45%) | 78 (50%) | 14 (30%) | 0.01 |
| Medium (1000-4000 TRY) | 101 (50%) | 72 (46%) | 29 (63%) | 0.04 |
| High (>4000 TRY) | 9 (4%) | 6 (4%) | 3 (6%) | 0.42 |
| Family history of premature CAD | 93 (46%) | 68 (44%) | 25 (54%) | 0.19 |
| Smoking status | ||||
| Never | 43 (21%) | 36 (23%) | 7 (15%) | 0.25 |
| Former | 110 (54%) | 81 (52%) | 29 (63%) | 0.18 |
| Active | 44 (22%) | 35 (22%) | 9 (20%) | 0.67 |
BMI: body mass index; CAD: coronary artery disease; TRY: Turkish lira; WC: waist circumference.
Laboratory findings, clinical characteristics and medications of the study population comparing physically active and inactive groups.
| All patients (n=202) | Physical activity | p | ||
|---|---|---|---|---|
| Absent (n=156) | Present (n=46) | |||
| Comorbidities | ||||
| Hypertension | 121 (60%) | 96 (61%) | 25 (54%) | 0.32 |
| Diabetes | 59 (29%) | 49 (31%) | 10 (22%) | 0.2 |
| Hyperlipidemia | 148 (73%) | 115 (74%) | 33 (72%) | 0.79 |
| Previous infarction | 85 (42%) | 64 (41%) | 21 (46%) | 0.57 |
| Valvular disease | 11 (5%) | 8 (5%) | 3 (6%) | 0.71 |
| Heart failure | 26 (13%) | 22 (14%) | 4 (9%) | 0.33 |
| Atrial fibrillation | 9 (4%) | 6 (4%) | 3(6%) | 0.42 |
| Cerebrovascular disease | 4 (2%) | 4 (3%) | 0 (0%) | 0.57 |
| Renal failure | 2 (1%) | 1 (1%) | 1 (2%) | 0.4 |
| SBP (mmHg) | 120 (110-130) | 120 (110-130) | 120 (110-130) | 0.65 |
| DBP (mmHg) | 77.5 (70-80) | 75 (70-80) | 80 (70-80) | 0.8 |
| Fasting blood glucose (mg/dl) | 101.5 (90-131) | 102 (91-134.7) | 97.5 (88.7-117) | 0.12 |
| Total cholesterol (mg/dl) | 172 (142-207) | 170 (141.2-206.2) | 182 (154.7-217.7) | 0.16 |
| LDL-C (mg/dl) | 98.5 (73.7-123.2) | 95.5 (72-122.5) | 101 (81.7-127) | 0.29 |
| HDL-C (mg/dl) | 40 (34-47) | 40 (34-47) | 40 (34.7-46) | 0.77 |
| Triglycerides (mg/dl) | 154 (90.5-219.2) | 154 (88-205.7) | 161.5 (113-251.7) | 0.23 |
| Revascularization procedure | ||||
| PCI | 104 (51%) | 82 (53%) | 22 (48%) | 0.57 |
| CABG | 67 (33%) | 53 (34%) | 14 (30%) | 0.65 |
| PCI+CABG | 31 (15%) | 21 (13%) | 10 (22%) | 0.17 |
| Urgent revascularization | 80 (40%) | 61 (39%) | 19 (41%) | 0.78 |
| DES (vs. BMS) | 26 (19%) | 16 (15%) | 10 (33%) | 0.02 |
| Additional surgery (valve) | 5 (2%) | 3 (4%) | 2 (9%) | 0.59 |
| Complicated revascularization | 17 (8%) | 12 (8%) | 5 (11%) | 0.54 |
| Time after revascularization (months) | 60 (24-120) | 48 (24-120) | 94 (36-111) | 0.15 |
| Recurrent procedures | 63 (31%) | 47 (30%) | 16 (35%) | 0.54 |
| Dietary adherence | 88 (44%) | 63 (40%) | 25 (54%) | 0.09 |
| Regular follow-up | 131 (65%) | 93 (60%) | 38 (83%) | 0.004 |
| Functional status (NYHA ≥2) | 84 (42%) | 66 (42%) | 18 (39%) | 0.7 |
| Symptomatic CAD (CCS class ≥1) | 153 (76%) | 121 (78%) | 32 (70%) | 0.26 |
| Medications | ||||
| Aspirin | 183 (91%) | 141 (90%) | 42 (91%) | 1 |
| Beta-blocker | 174 (86%) | 138 (88%) | 36 (78%) | 0.07 |
| ACE inhibitor/ARB | 158 (78%) | 123 (79%) | 35 (76%) | 0.69 |
| Statin | 104 (51%) | 78 (50%) | 26 (56%) | 0.43 |
| Clopidogrel | 64 (32%) | 49 (31%) | 15 (33%) | 0.87 |
| Spironolactone | 28 (14%) | 23 (15%) | 5 (11%) | 0.5 |
| Nitrates | 36 (18%) | 28 (18%) | 8 (17%) | 0.93 |
| CCB | 27 (13%) | 23 (15%) | 4 (9%) | 0.28 |
| Other antianginal | 36 (18%) | 30 (19%) | 6 (13%) | 0.33 |
| Non-cardiac drug | 82 (41%) | 66 (42%) | 16 (35%) | 0.36 |
ACE: angiotensin-converting enzyme; ARB: angiotensin receptor blocker; BMS: bare-metal stent; CABG: coronary artery bypass grafting; CAD: coronary artery disease; CCB: calcium channel blocker; CCS: Canadian Cardiovascular Society; DBP: diastolic blood pressure; DES: drug-eluting stent; HDL-C: high-density lipoprotein cholesterol; LDL-C: low-density lipoprotein cholesterol; NYHA: New York Heart Association; PCI: percutaneous coronary intervention; SBP: systolic blood pressure.
The results of univariate and multivariate logistic regression analysis are listed in Table 3. In multivariate regression analysis, low education level (p=0.01, odds ratio [OR] 3.26, 95% confidence interval [CI]: 1.31-8.11), and lack of regular follow-up (p=0.04, OR 2.95, 95% CI: 1.01-8.61) were found to be independent predictors of absence of regular PA in study subjects after adjusting for other confounders.
Predictors of absence of regular physical activity according to logistic regression analysis.
| Variable | Univariate analysis | Multivariate analysis | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | |
| Age | 1 | 0.97-1.03 | 0.63 | |||
| Female gender | 2.4 | 1.0-5.75 | 0.049 | |||
| Low education level | 2.74 | 1.37-5.49 | 0.004 | 3.26 | 1.31-8.11 | 0.01 |
| Unemployment | 7.84 | 1.81-33.81 | 0.006 | |||
| Low household income | 2.28 | 1.13-4.61 | 0.02 | |||
| Widowed or separated | 2.86 | 0.82-9.94 | 0.09 | |||
| Active smoking | 1.18 | 0.52-2.7 | 0.67 | |||
| BMI | 1.06 | 0.97-1.15 | 0.14 | |||
| WC | 1.01 | 0.99-1.03 | 0.27 | |||
| Urgency of revascularization | 1.12 | 0.62-2.02 | 0.7 | |||
| Stent type (BMS vs. DES) | 2.75 | 1.08-6.95 | 0.03 | |||
| Comorbidity | 1.45 | 0.7-3.02 | 0.31 | |||
| Previous MI | 0.82 | 0.42-1.6 | 0.57 | |||
| Heart failure | 1.72 | 0.56-5.28 | 0.34 | |||
| Multiple comorbidities | 1.41 | 0.73-2.73 | 0.3 | |||
| Complication of revascularization | 0.95 | 0.73-1.23 | 0.7 | |||
| Time after revascularization | 0.99 | 0.99-1.0 | 0.19 | |||
| Recurrent procedures | 0.99 | 0.66-1.49 | 0.98 | |||
| Lack of dietary adherence | 1.75 | 0.9-3.4 | 0.09 | |||
| Lack of regular follow-up | 3.21 | 1.4-7.35 | 0.006 | 2.95 | 1.01-8.61 | 0.04 |
| Functional status (NYHA ≥2) | 1.14 | 0.58-2.23 | 0.7 | |||
| Symptomatic CAD | 1.51 | 0.72-3.14 | 0.26 | |||
BMI: body mass index; BMS: bare-metal stent; CAD: coronary artery disease; CI: confidence interval; DES: drug-eluting stent; MI: myocardial infarction; NYHA: New York Heart Association class; OR: odds ratio; WC: waist circumference.
The present study examined the parameters that influence PA in patients with a history of coronary revascularization. Low education level and lack of regular follow-up were identified as independent predictors of absence of regular PA.
In our study, the majority of the patient population were inactive. In the inactive group, female gender, low education level, unemployment, and low household income were common, while follow-up visit rates were lower. In patients with a history of previous PCI, bare-metal stents were more commonly used in the inactive group than in the active group.
Physical inactivity is a modifiable risk factor.16 Current guidelines recommend a minimum of 30-60 min of moderate PA four to five times a week, coupled with an increase in daily lifestyle activities, in order to prevent heart attack and death among patients with coronary heart disease.17 PA has been associated with a 25-30% reduction in CAD-related mortality, attributed to improvements in major risk factors and reduction of inflammation.9,18 In addition to mortality reduction, PA reduces recurrent of ischemia and improves quality of life.19 Kavanagh et al. reported that high aerobic capacity was associated with lower mortality rates in patients with CAD who had well-controlled diabetes.20,21
Despite these beneficial effects of PA, many studies including patients with CAD have found that most patients do not comply with recommendations for regular PA.22 Less than 25% of patients on cardiac rehabilitation programs do regular exercise and during follow-up most fail to complete the program.19 Recommendations for PA in patients with coronary revascularization are mainly made by physicians following the patients, and these proposals tend not to be detailed, due to their heavy workload. In some countries these programs are determined by some individual based training programs. Despite these efforts, adherence rates of cardiac rehabilitation programs are reported to be 41%.23
It is clear that the most important aspect of PA in patients with CAD is compliance, and so it is important to investigate parameters that influence dropout rates from recommended PA.
Patients with chronic diseases are able to improve their condition with adequate information and education and PA improves quality of life, as shown in previous studies.24,25 Social, economic and cultural factors play a role in the maintenance of sedentary life styles.26
Patient adherence is determined by multiple factors such as education level, employment status and household income. In our study women were generally inactive, only seven (12% of women in the study population) being physically active. Stewart et al. showed that advanced age, male gender and obesity were associated with less PA.27 In their study, most women were housewives and reported more PA because of housework.27 In our study, the majority of females were housewives, but they were significantly less active than men; we did not define housework as PA. It should also be noted that women account for only a small number of subjects in studies on PA and cardiac rehabilitation.9,28 Another study reported that obese patients were less likely to complete exercise programs, but found no difference between female and male patients, as well as the interesting result that young patients were more likely to drop out of the exercise program.29 In agreement with our study, Reid et al. found that males were more active than females and that educational level was associated with PA.30
Most studies on PA have been performed on the general population, but CAD patients differ in various aspects.27 Patients with CAD may experience more adverse events when they perform intense exercise,15 and are more likely to feel symptoms that cause premature interruption of exercise.7,27 Mood disorders that could affect PA adherence are also more frequent in patients with CAD.27
The results of our study indicate that socioeconomic status also affects adherence to regular PA.27 In previous studies, lower socioeconomic status and educational level were associated with increased morbidity and mortality in patients with CAD.31–33 Educational level and employment status were particularly associated with CAD.34 The WISE trial showed that low household income, smoking, higher BMI and greater waist circumference were associated with lower PA.35
Some trials have shown that patients treated by CABG are more active than those treated by PCI, however we found no difference in PA between types of coronary intervention. A possible explanation may be that CABG patients are encouraged to exercise by doctors and nurses to reduce pulmonary complications after surgery. Interestingly, we found that patients receiving drug-eluting stents were more active than those receiving bare-metal stents.
During hospital stay, encouragement to perform PA should be part of patient management. Educational programs can be prepared for patients with CAD and their relatives, and the value of cardiac rehabilitation should be emphasized at each hospital visit in order to raise awareness of the importance of PA.
The present study has some limitations, of which the most important is the use of self-reporting instead of objective measures to characterize adherence to exercise. The study was conducted in a single tertiary center, and so the patients may not represent real-world populations. Cognitive status and physical factors that may have affected PA were not assessed.
ConclusionRegular PA is inadequate in outpatients with a history of previous coronary revascularization. Education level and regular follow-up visits can potentially influence PA adherence. Educational programs or telephone contact should be used to achieve more physically active lifestyles in these patients.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.