We report the case of a 69-year-old man, a former smoker with hypertension, who underwent emergent coronary angiography after an anterior ST-segment elevation myocardial infarction (STEMI). Pre-treatment with aspirin, clopidogrel and un-fractioned heparin (UFH) was administered. Coronary angiography revealed a large contrast filling defect at the distal segment of aneurysmatic left main coronary artery (LMCA) (Figure 1A-1B, Online-Video 1). An intravascular ultrasound (IVUS) was performed to assess the intracoronary mass, showing a large LMCA thrombosis without underlying coronary plaques (Figure 1C-1D).
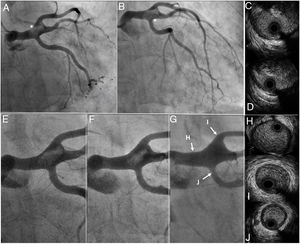
Baseline and follow-up angiographies and intravascular ultrasound.
(A, B) Baseline coronary angiography showed a coronary mass in distal left main coronary artery (white asterisks); Online-Video 1.
(C-D) Baseline intravascular ultrasound showed a large intraluminal mass, presenting a variable gray scale with speckling, suggestive of thrombus.
(E-G) Progressive and complete thrombus dissolution on coronary angiographies; Online-Video 2-4.
(H-J) Final intravascular ultrasound demonstrated the absence of thrombus and atherosclerotic disease.
Intracoronary half-dose of tenecteplase and abciximab was administered. After initial management, an aggressive in-hospital antithrombotic strategy with aspirin, ticagrelor and intravenous UFH was followed. A total of three serial coronary angiographies were performed over the next two weeks, showing a progressing reduction of thrombus burden until there was complete dissolution (Figure 1E, 1F, 1G, Online-Video 2-4). Finally, IVUS reconfirmed the absence of coronary parietal disease (Figure 1H-1J). Patient was discharged under aspirin, clopidogrel and acenocumarol for one month, followed by aspirin and acenocumarol. Twelve months later, the patient remained asymptomatic without bleeding events.
Restoring coronary flow and avoiding distal embolization are the two major goals in STEMI. Nevertheless, the management of massive coronary thrombosis in aneurysmatic arteries is challenging due to the high risk of non-reflow and embolization associated with coronary manipulation, in addition to the risk of in-stent thrombosis and/or restenosis due to a probable scaffold malapposition in the future. We note that our case shows that an aggressive antithrombotic regimen could represent a successful strategy in these patients if coronary flow is preserved, even in LMCA thrombosis.
Conflicts of interestThe authors have no conflicts of interest to declare.