We report the case of a 40-year-old man with known Marfan syndrome who presented with severe aortic valve regurgitation secondary to significant aortic root dilatation. To rule out coronary artery disease and to evaluate the rest of the thoracic aorta before surgery, cardiac computed tomography (CT) was performed. A brief review of the literature shows how cardiac CT can, in selected cases, rule out coronary artery disease before non-coronary cardiothoracic surgery.
Descrevemos o caso de um doente de 40 anos de idade com Síndrome de Marfan, que apresenta regurgitação valvular aórtica grave, secundária a dilatação severa da raiz aórtica. Para excluir a presença de doença coronária e estudar os restantes segmentos aórticos antes da cirurgia, foi realizada uma angioTC cardíaca.Uma breve revisão da literatura demonstra como, em determinados contextos, a angioTC cardíaca pode ter vantagens na exclusão de doença coronária antes de cirurgia cardio-torácica não coronária.
We report the case of a 40-year-old man with no known cardiovascular risk factors who was diagnosed with Marfan syndrome at the age of 32. His medical history included gastroesophageal reflux syndrome and previous ophthalmic surgery for lens dislocation and orthopedic surgery on the tibial-tarsal joints. He was being medicated with bisoprolol and pantoprazole.
For the previous six months he had presented worsening exercise dyspnea and had marked limitation in activity due to symptoms (NYHA class II–III).
The echocardiogram showed severe aortic valve regurgitation secondary to significant aortic root dilatation (64 mm diameter at the Valsalva sinus) and left ventricular dilatation, but with normal systolic function.
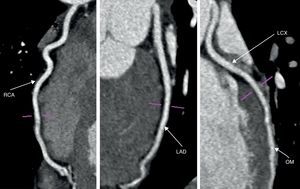
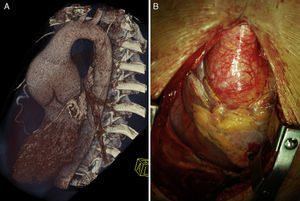
To exclude coronary artery disease and simultaneously to evaluate the rest of the thoracic aorta, cardiac computed tomography (CT) was performed (including the thoracic aorta). This exam ruled out coronary artery disease (Figure 1) and confirmed the presence of significant aortic root dilatation (70 mm), the rest of the aorta being normal (Figure 2).
The patient was referred for surgery, with no need for invasive catheterization. He underwent a Bentall procedure with implantation of an aortic conduit and a prosthetic aortic valve (29 mm St. Jude). There were no complications after surgery, the echocardiogram showing the prosthetic aortic valve with normal motion and the conduit functioning correctly. The patient was discharged six days later and warfarin was added to his medication.
At 6-month follow-up the patient was asymptomatic and free from cardiovascular events.
DiscussionMarfan syndrome is the most common inherited multisystemic disorder of connective tissue, with a reported incidence of 2-3 per 10000 population, without gender, racial, or ethnic predilection.1 Its cardiovascular features were first outlined by McKusick in 19552; according to the current diagnostic criteria major cardiovascular manifestations include dilatation of the ascending aorta, with or without dissection.3
In the presence of ascending aorta dilatation, prophylactic surgery is recommended when the diameter of the ascending aorta at the aortic sinuses reaches 4.5 cm, or in some cases even less (when there is a family history of aortic dissection, in the presence of rapid aortic dilatation or severe aortic valve regurgitation, or when a valve-sparing operation is possible).1,4
In the case reported, the presence of severe aortic root dilatation (>60 mm) with associated aortic valve regurgitation was a clear indication for surgery.
Although the patient had no angina, obstructive coronary artery disease was ruled out prior to aortic surgery. This evaluation should be performed in asymptomatic male patients over the age of 40 or postmenopausal women, and is also indicated for patients with previous coronary artery disease, symptoms of left ventricular dysfunction, presumed ischemic mitral regurgitation or one or more cardiovascular risk factor.4
Traditionally, the study of coronary artery anatomy is performed through invasive angiography. However, this can also be safely done with cardiac CT5,6 taking advantage of the high negative predictive value of this exam6; this is one indication for which cardiac CT can replace invasive angiography.7
This approach can be applied to a high percentage of patients when study of coronary artery anatomy is indicated prior to valvular or aortic surgery, as it is more convenient and less invasive than invasive coronary angiography. Furthermore, some patient subsets may derive greater benefit from this approach, when there is higher iatrogenic potential (such as in the presence of aortic dissection or aortic valve thrombus/vegetations) or when coronary catheterization would be difficult (such as in the presence of aortic root dilatation or anomalous coronary artery origin). In these cases, cardiac CT, avoiding the need for potential prolonged invasive cardiac catheterization, reduces not only radiation and contrast doses, but also the risk of complications. Among the latter, aortic dissection has been described as a rare (0.04%) but serious complication of cardiac catheterization and was found to be associated with the use of non-conventional catheters.8
The risk of contrast-induced nephropathy should be weighed when coronary angiography is considered. Since there are no differences in the contrast dose used in coronary angiography performed invasively or by cardiac CT,9 this risk should be similar with both techniques.
In the case reported, there were two risk factors for complications with invasive coronary angiography: the presence of aortic root dilatation and severe aortic valve regurgitation. This favored the choice of cardiac CT to study the cardiac anatomy, which was safe, ruled out coronary artery disease and simultaneously provided detailed anatomy of the thoracic aorta.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.