We describe the case of a 61-year-old man who presented with chest pain and ST-segment elevation in the anterior precordial leads (V1–V5) due to proximal occlusion of the right ventricular branch of a codominant right coronary artery. Primary coronary angioplasty and stenting of this branch was performed resulting in resolution of the chest pain and ST-segment elevation. Our description illustrates a case of isolated right ventricular infarction as an uncommon but important differential diagnosis of anterior ST-segment elevation. In addition, it highlights the value of careful review of the angiographic images in this context, as the culprit lesion may be a right ventricular branch occlusion. To the best of our knowledge, this is the first reported case of primary percutaneous coronary intervention treatment of a right ventricular branch occlusion causing isolated acute right ventricular myocardial infarction and anterior ST-segment elevation.
Descreve-se o caso de um homem de 61 anos que se apresentou com dor torácica típica e supradesnivelamento do segmento ST nas derivações precordiais (V1-V5). A coronariografia de urgência revelou a oclusão proximal de um ramo ventricular da artéria coronária direita. Foi realizada angioplastia primária deste ramo com implantação de stent metálico convencional, resultando na resolução da dor torácica e da elevação ST. A presente descrição ilustra um caso de enfarte isolado do ventrículo direito como um diagnóstico diferencial pouco comum mas importante de elevação ST nas derivações precordiais. O presente caso realça ainda a importância de uma cuidadosa revisão das imagens angiográficas neste contexto, uma vez que a lesão culpada pode ser a oclusão de um ramo ventricular direito. Segundo a nossa pesquisa, o presente caso trata-se da primeira descrição de intervenção coronária percutânea primária de um ramo ventricular direito causando enfarte isolado do ventrículo directo e elevação ST nas derivações precordiais.
The presence of ST-segment elevation in the anterior precordial leads in patients with acute coronary syndromes usually indicates left anterior descending coronary artery occlusion. However, anterior ST-segment elevation has also been described in right coronary artery (RCA) occlusion and is thought to signify right ventricular myocardial infarction (RVMI). We describe a case of isolated RVMI presenting with anterior ST-segment elevation due to proximal occlusion of a right ventricular branch that was treated by primary angioplasty.
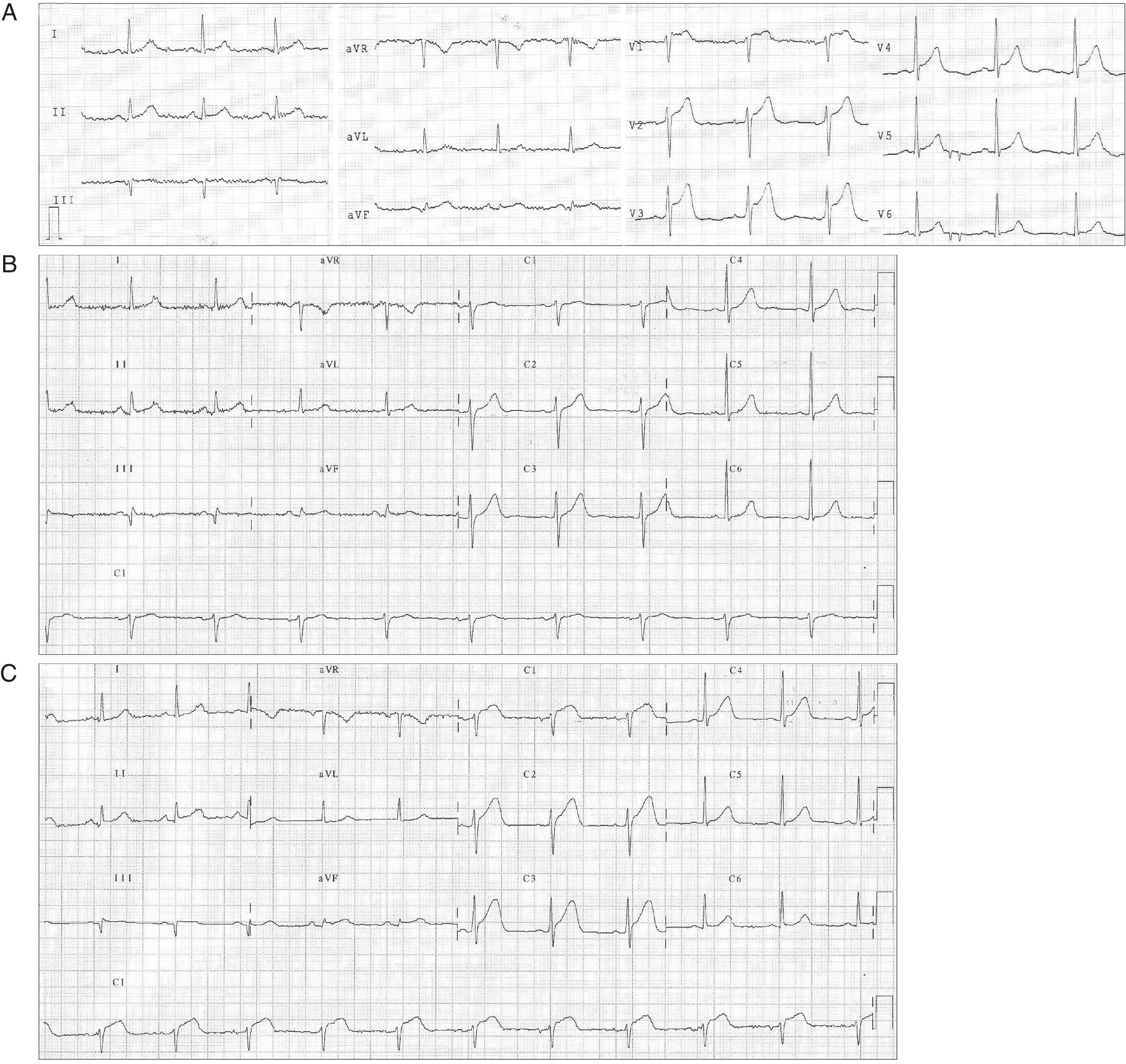
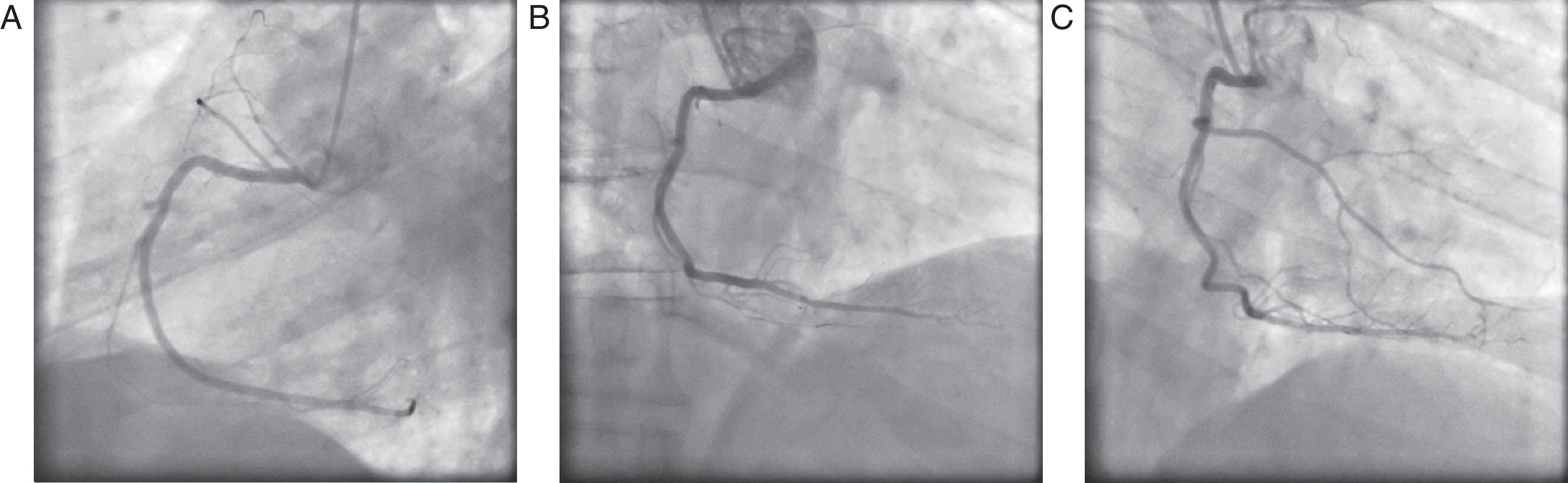
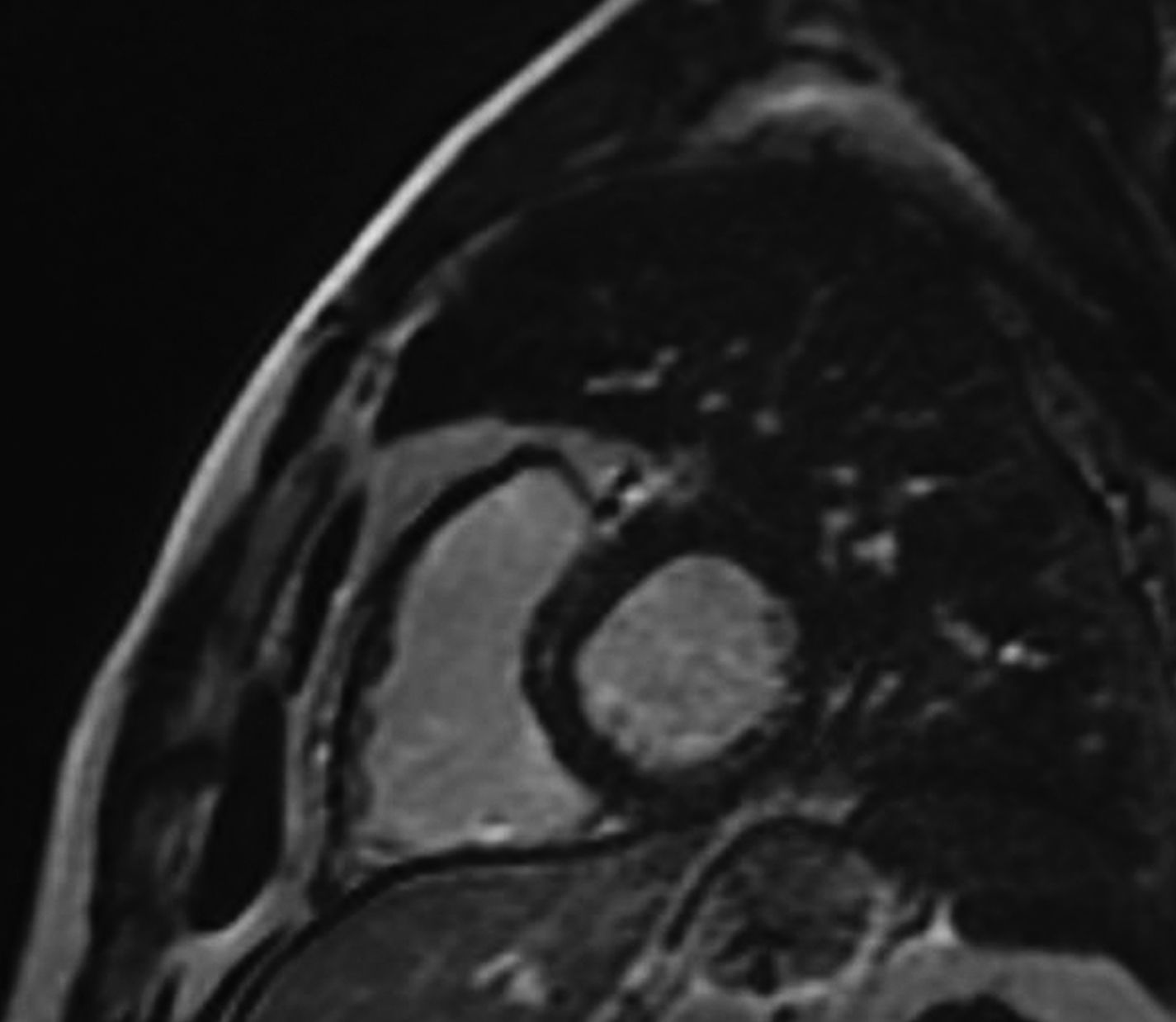
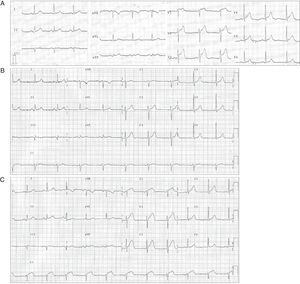
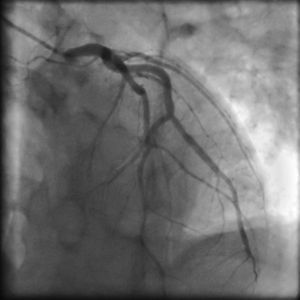
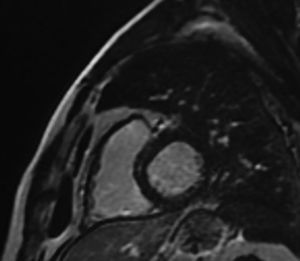
Case reportA 61-year-old man with no history of cardiac disease presented to a community hospital reporting typical chest pain 3hours in duration with more severe intensity in the last 30minutes. The initial standard 12-lead electrocardiogram (ECG) showed ST-segment elevation in leads V1–V5 and slight ST-segment elevation in the inferior leads (Fig. 1A). The patient was given 5000U of unfractionated heparin IV, 600mg clopidogrel oral loading dose and 300mg oral aspirin, and was transferred to our hospital for urgent catheterization. He arrived at our cath lab hemodynamically stable, with persistent chest pain. Coronary angiography, performed four and a half hours after symptom onset, showed a normal left coronary artery (Fig. 2) and patent main vessel of the codominant RCA. Left ventriculography was normal. Careful review of the coronary angiogram revealed proximal occlusion of the right ventricular (RV) branch of the RCA (Fig. 3A and B). The RV branch occlusion was managed with balloon dilation and stenting (2.0mm×12.0mm bare-metal stent at 16atm, Multi-Link Mini Vision®, Abbott Vascular, USA), resulting in resolution of the chest pain and ST-segment elevation (Figs. 1B and 3C). One hour after the procedure the patient experienced a new episode of chest discomfort and ST-segment changes similar to the initial ECG (re-elevation in leads V1–V4 and slight elevation in leads II, III, and aVF) (Fig. 1C). Emergency coronary angiography demonstrated acute stent thrombosis, which was probably related to previous inadequate stent covering of the proximal portion of the coronary plaque. Abciximab infusion was initiated, thrombus aspiration was performed and another proximal and overlapped bare-metal stent (2.25mm×12.0mm at 12atm, Multi-Link Mini Vision®, Abbott Vascular, USA) was implanted, again resulting in resolution of chest pain and ST-segment elevation. The peak troponin I level was 5.2ng/ml. The patient recovered without sequelae and was asymptomatic and fully active one month later. Contrast-enhanced magnetic resonance imaging (MRI) performed 30 days after presentation showed normal left ventricular function and normal right ventricular size and motion. No area of delayed hyperenhancement was visualized (Fig. 4).
(A) Initial ECG showing ST-segment elevation in the anterior precordial leads. (B) Post-coronary angioplasty ECG showing normal sinus rhythm with resolution of ST-segment elevation and no anterior Q waves. (C) Acute stent thrombosis causing new ST-segment elevation in leads V1–V4 and slight ST-segment elevation in leads II, III, and aVF.
Isolated RVMI is uncommon, with autopsy series indicating that it occurs in less than 3% of all patients with myocardial infarction.1 It has been described essentially in two anatomical contexts: occlusion of a nondominant RCA,2 and loss of large RV branches during coronary angioplasty of the RCA.3 There have been few reports of anterior ST-segment elevation caused by isolated RVMI due to RV branch occlusion in the absence of percutaneous coronary intervention.4
Although it is usually considered that occlusion of a small nondominant right coronary artery is not associated with significant consequences, there are reports of cases presenting with sudden cardiac death.5 Importantly, there are also reports of sudden cardiac death in which autopsy confirmed the occlusion of a branch of the RCA causing isolated RVMI.6 Our case, to the best of our knowledge, is the first one reported of primary percutaneous coronary intervention treatment of an RV branch occlusion causing isolated acute RVMI and anterior ST-segment elevation. Acute stent thrombosis with recurrence of chest pain and anterior ST-segment re-elevation was successfully managed percutaneously. Revision of images of the first intervention showed that the proximal portion of the unstable coronary plaque was not covered by the stent. Another stent was implanted, proximal and overlapped to the previous one, to cover all the unstable plaque. Minimal myocardial necrosis was demonstrated by troponin assay and follow-up contrast-enhanced MRI showed no areas of delayed hyperenhancement in the right or left ventricles.
When isolated RVMI occurs, the ECG may show an acute anterior ST-segment elevation pattern (leads V1 through V5) and right ST-segment elevation (leads V3R through V6R, which were not performed in our case). However, isolated ST-segment elevation due to RVMI is uncommon in clinical practice. Since RVMI usually occurs with simultaneous left ventricular inferior infarction, the electrical current of injury from the left ventricle dominates the RV electrical forces. The typical ECG changes in this setting are ST-segment elevation in the inferior leads with concomitant ST-segment depression in the precordial leads if the left ventricular posterior wall is involved.7
Certain electrocardiographic features have been suggested which may help differentiate ST-segment elevation secondary to isolated RVMI from left anterior descending artery territory infarction. However, these features are not pathognomonic and it may be impossible to make this distinction on the basis of electrocardiography alone. The absence of Q-wave development in the anterior precordial leads has been reported as favoring the diagnosis of RVMI,7 as was observed in our case. Nevertheless, other suggested features such as progressive reduction in ST-segment elevation across the precordial leads7 were not seen in this case. In addition, an electrocardiographic criterion described by Lopez-Sendon et al.8 in the differential diagnosis of RVMI and anteroseptal MI is the relationship between ST-segment elevation in V4R–V3. In most patients with RVMI, ST-segment elevation in V4R is higher than that found in V1–V3.
ConclusionOur description clearly illustrates a case of isolated RVMI as an uncommon but important differential diagnosis of anterior ST-segment elevation and highlights the value of careful review of angiographic images, as the culprit lesion may be an RV branch occlusion. Primary percutaneous intervention of these branch vessels is possible and enables complete resolution of chest pain and ST-segment changes, minimization of the damage to the RV myocardium, and avoidance of malignant arrhythmias.
Conflicts of interestThe authors have no conflicts of interest to declare.