Non-occlusion of the internal mammary artery side branches may cause ischemia due to flow diversion after coronary artery bypass grafting.
The authors present the case of a 67-year-old man with recurrent angina after undergoing myocardial revascularization with a left internal mammary artery to left anterior descending bypass. He presented with impaired anterior wall myocardial perfusion in the setting of a patent left internal mammary artery side branch. Effective percutaneous treatment was carried out through coil embolization, with improved flow and clinical symptoms, confirmed through ischemia testing.
Coronary steal through a patent mammary artery side branch is a controversial phenomenon and this type of intervention should be considered only in carefully selected patients.
A não oclusão de ramos laterais da artéria mamária interna após cirurgia de revascularização miocárdica pode causar isquemia devido ao desvio do fluxo coronário.
Os autores apresentam o caso de um homem de 67 anos de idade, com angina recorrente após revascularização miocárdica com bypass da artéria mamária interna esquerda para a artéria descendente anterior. O doente apresentava redução da perfusão miocárdica na parede anterior na presença de um ramo patente da artéria mamária interna. Foi realizada de forma eficaz a embolização percutânea com coils deste ramo com melhoria do fluxo e dos sintomas clínicos, dados confirmados com testes de avaliação de isquemia.
O roubo coronário através de ramos laterais patentes da artéria mamária ainda é um fenómeno controverso e este tipo de intervenção deve ser apenas considerada no tratamento de pacientes bem selecionados.
Coronary steal due to an unligated side branch of the internal mammary artery (IMA) is a rare but important condition that can cause ischemia in patients after coronary artery bypass surgery. Although this is a known phenomenon, it is not always easy to relate it to the patient's symptoms.
We describe the case of a patient with significant ischemia in whom an unligated side branch was successfully treated by coil embolization. This intervention can be a useful option and should be considered in the management of symptomatic patients with patent IMA side branches.
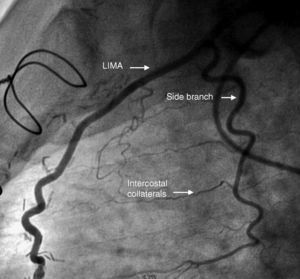
Case reportThe authors present the case of a 67-year-old man who had undergone coronary artery bypass grafting after an acute myocardial infarction over four years previously, due to an ostial lesion in the left anterior descending (LAD) artery, with a left internal mammary artery (LIMA) to LAD bypass. One year after the procedure he was admitted to the cardiac intensive care unit for unstable angina. He underwent coronary angiography, which revealed an 80% stenosis in the bypass anastomosis, and angioplasty with a drug-eluting stent was successfully performed. The angiogram also showed a branch arising from a very proximal segment of the LIMA, not occluded during the surgery and supplying the whole lateral chest wall via numerous intercostal collaterals (Figure 1). Due to the bypass stenosis the clinical importance of the patency of this vessel was not appreciated. After this angioplasty he presented with early-onset recurrent angina, and performed a treadmill stress test that was symptomatic and electrically positive for ischemia. Repeated coronary angiography showed the graft and the stent to be patent, without evolution of the native disease.
After discharge the patient remained highly symptomatic despite optimal medical therapy.
Dobutamine stress echocardiography showed inducible ischemia in the anterior wall distribution. These findings led to a diagnosis of a probable steal phenomenon due a patent IMA side branch. Percutaneous coil embolization of this branch was performed. The left internal mammary artery was selectively cannulated with a Heartrail catheter inside a 6-F femoral guiding catheter via the right femoral artery and a microcatheter was advanced over the guidewire into the side branch. Following removal of the guidewire, detachable embolization coils (Tornado®, Cook Medical, 4/2 mm, 4/2 mm and 3/2 mm) were placed in the side branch.
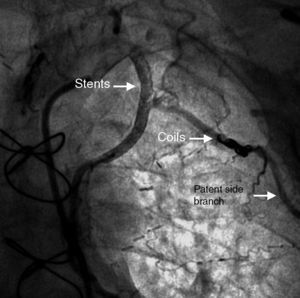
The coils were attached to a delivery wire and were released in the appropriate position. During the procedure, a dissection was detected in the proximal region of the LIMA and two biolimus and bioabsorbable polymer stents (Biomatrix 3 mm × 24 mm and 3 mm × 28 mm distal and proximal, juxtaposed) were implanted, covering the entire dissected segment. Control angiography at the end of the procedure showed the side branch still patent but with compromised flow (Figure 2)
At one-month follow-up, the patient reported clinical improvement and increased functional capacity. He underwent treadmill stress testing and repeated dobutamine stress echocardiography four months after the procedure, which showed no evidence of ischemia.
DiscussionAlthough the use of LIMA to LAD grafts as a means of revascularization is routine and effective, it is not a risk-free procedure. There can be various reasons for ischemic symptoms in patients who have undergone coronary artery bypass surgery, including incomplete revascularization at the time of surgery, progression of atheromatous disease or graft occlusion. A rare cause of recurrent symptoms can be an anomalous or persistent chest wall branch causing flow “steal”.
The hemodynamic importance of these branches is still unclear, since many patients have them, but few lead to symptoms. LIMA side branches to the chest wall have been identified both preoperatively and postoperatively in 10–20% of patients.1 Although a number of studies have reported successful occlusion of the side branches to relieve angina,2–5 this phenomenon has been confirmed in some studies that aimed to obtain hemodynamic data, but rejected in others.6–8
A major argument is that LIMA side branch steal is supposedly a systolic flow diversion and not a true coronary flow steal. The arterial flow to the chest wall is predominantly systolic and out of phase with the predominantly diastolic coronary circulation.9 It has been shown that the limited functional flow reserve of the in situ IMA minimizes the possibility of significant flow steal from patent IMA graft collaterals, even after muscular vasodilatation.6 Indeed no study measuring coronary velocities in post-CABG patients has suggested that IMA side branches are of clinical significance unless there are unusual hemodynamic circumstances.8 This leads many authors to argue that complete LIMA harvesting is not mandatory7 and that occlusion is unwarranted unless it can be shown to increase LIMA flow or objectively reduce myocardial ischemia.10
Nevertheless, as previously stated, many reports of clinical improvement following LIMA occlusion contradict these pathophysiological studies.
Major factors contributing to IMA side branch steal may include technical errors or anatomic factors which reduce IMA run-off and possibly divert it into large side branches with lower resistance.11
Several methods of occlusion of the side branches have been described, including embolization, the use of gelatin sponge particles and the combined use of drug-eluting and covered stents. Surgical ligation both via an open route and by video-assisted thoracoscopic surgery has been successfully performed. Recently, the use of vascular plugs (originally developed for closing arteriovenous fistulae) for occluding such side branches has also been described.5 In our patient we used platinum coils, which are easily detected radiographically, feature synthetic fibers that promote thrombogenicity, and are ideally suited for tapering vessel situations. Although in the case described transcutaneous closure was complicated by dissection of the LIMA, coil deployment can be regarded as safe, with early mobilization and lower morbidity and mortality compared to reoperation.3
Given the above controversies and the different possible technical approaches with their inherent limitations, the decision to close these side branches and the way it is performed should be carefully weighed. It should only be considered when a correlation between the patency of the side branch and the patient's symptoms is indisputable.
ConclusionThe physiological significance of IMA side branches has been clinically and experimentally questioned. Occlusion of these branches is not recommended without objective evidence of ischemia but in our case anterior wall myocardial perfusion was clearly impaired in the setting of a patent LIMA-LAD graft and an anomalous side branch, with clinical improvement after intervention. Coronary steal due to an unligated side branch of the LIMA is rare but should be borne in mind as a possible and treatable cause of ischemia after coronary artery bypass surgery.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.