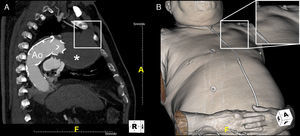
We present the case of a 76-year-old Caucasian man with a type 1 endoleak at the proximal edge of a thoracic stent-graft (Talent™ 38 mm×114 mm) detected four years after endovascular treatment of a large symptomatic saccular aneurysm in the distal aortic arch. The patient refused any interventional treatment for the endoleak and remained on medical therapy with no evolving symptoms. Surveillance cardiac tomography (CT) showed the aneurysm continuing to expand, extending towards the chest wall and causing erosion of the ribs (Figure 1).
ECG-gated cardiac computed tomography of our patient showing the natural history of a left untreated type 1 endoleak (arrowhead) at the proximal edge of a stent-graft in the aortic arch (Ao). Upper panel (A1–C1) presents three-dimensional reconstructions (volume-rendering technique); lower panel (A2–C2) presents the corresponding images in the axial plane (maximum intensity projection). Over time (from A to C), the aneurysmal sac (*) continued to be pressurized and expanded towards the chest wall, ultimately causing erosion of the second left rib (box).
After two years, the patient caught influenza with intense cough and suddenly noticed a pulsatile lump in his left chest wall. A new CT revealed the aneurysm expanding through the first left intercostal space, reaching the chest wall surface (Figure 2).
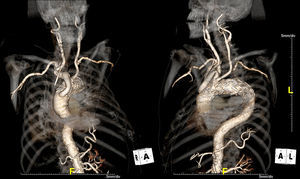
Facing extremely high risk of rupture and death, the patient accepted treatment and underwent a hybrid technique with extra-anatomic ascending aorta-to-brachiocephalic bypass (without cardiopulmonary bypass) and endovascular insertion of an additional stent-graft (Valiant™ 42 mm×150 mm) in the ascending aorta-aortic arch transition (Figure 3). The procedure was successful with complete endoleak exclusion and no major post-procedure complications. The patient was discharged home but died two months later. The exact cause of death remains to be elucidated (there was no autopsy).
Performed hybrid technique in three-dimensional reconstructions: surgical extra-anatomic ascending aorta-to-brachiocephalic bypass (the patient presented a common origin of the brachiocephalic trunk and left common carotid artery) followed by endovascular insertion of an additional prosthesis in the ascending aorta-aortic arch transition.
In endovascular repair of aortic arch aneurysms an adequate landing zone is often difficult to ensure, predisposing to type I endoleaks. Endovascular or surgical intervention should be promptly offered to achieve optimal outcomes. When left untreated, the aneurysmal sac continues to be pressurized with continuing expansion and high risk of rupture.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.