We present the case of a 47-year-old man with hypertension for over 20 years, referred to our hospital due to mild aortic dilatation detected on a transthoracic echocardiogram. On physical examination weak lower limb pulses and a blood pressure differential of >50 mmHg between arms and legs were detected. Complete interruption of the aortic arch below the left subclavian artery was diagnosed by computed tomography angiography. With this case we aim to draw attention to aortic coarctation and interrupted aortic arch as potential causes of hypertension and to highlight the importance of the physical examination in the diagnosis of secondary causes of hypertension.
Apresentamos o caso de um homem de 47 anos, com hipertensão arterial desde há mais de 20 anos, referenciado ao nosso hospital por dilatação ligeira da aorta ascendente detetada em ecocardiograma transtorácico. No exame físico constatou-se que os pulsos femorais eram pouco amplos e existia um diferencial de pressões superior a 50 mmHg entre os membros superiores e inferiores. Por angiotomografia computorizada do tórax diagnosticou-se uma interrupção completa do arco aórtico abaixo da artéria subclávia esquerda. Com este caso pretendemos relembrar a coartação da aorta e interrupção do arco aórtico como potenciais causas de hipertensão e realçar a importância do exame físico no diagnóstico de causas secundárias de hipertensão.
Hypertension is an increasingly important medical and public health issue, with an overall prevalence of 30–45% of the general population.1 Appropriate diagnosis and treatment are important in reducing hypertension-related morbidity, mortality and costs. A detailed medical history and a rigorous physical examination have a pivotal role in the accurate diagnosis of hypertension, particularly for the detection of underlying secondary causes.2
Aortic coarctation and interrupted aortic arch (IAA) are examples of rare potential secondary causes of hypertension in adults. These entities can be easily diagnosed on physical examination, by palpation of the brachial and femoral arterial pulses and blood pressure measurement in the four limbs. However, there are reports showing that the diagnosis is often missed and a significant number of asymptomatic subjects are probably not detected until adulthood.3
Case reportWe present the case of a 47-year-old male patient with a history of untreated high blood pressure since the age of 25. At 40 years old, he suffered an intracranial hemorrhage due to rupture of a right anterior choroidal artery aneurysm and underwent aneurysm clipping. He was then referred to an outpatient hypertension clinic for management and etiological study. Laboratory and imaging studies were performed with no apparent secondary causes of hypertension detected. With a presumed diagnosis of essential hypertension, the patient remained asymptomatic and with well-controlled blood pressure in the following years, taking irbesartan 300 mg plus hydrochlorothiazide 12.5 mg/day and amlodipine 5 mg/day.
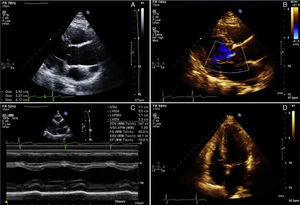
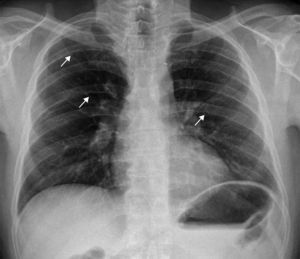
At the age of 47, he was referred to our hospital's outpatient cardiology clinic due to mild dilatation of the aortic root and ascending aorta detected on a transthoracic echocardiogram (Figure 1A). The aortic valve was tricuspid with mild central regurgitation, and the left ventricle presented normal dimensions, mild concentric hypertrophy and preserved systolic function (Figure 1B–D). Due to a poor suprasternal view, the aortic arch could not be observed. Blood pressure was 135/80 mmHg in both arms. Lower limb pulses were weakly palpable and blood pressure was significantly lower (80/60 mmHg), so aortic coarctation was considered. No cardiac, dorsal or abdominal murmurs were audible. On the 12-lead electrocardiogram he had incomplete right bundle branch block and left ventricular hypertrophy. Chest radiography showed normal cardiac silhouette and bilateral rib notching (Figure 2).
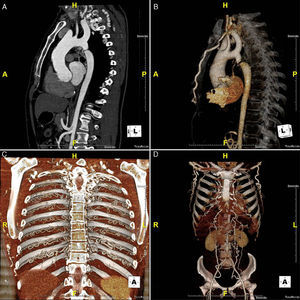
Multislice computed tomography angiography revealed an unexpected finding: complete interruption of the aortic arch 15 mm distal to the origin of the left subclavian artery (LSA) (Figure 3A and B). The ascending aorta was slightly dilated (42 mm) and the descending thoracic and abdominal aorta were hypoplastic (diameters of 16 mm and 11 mm, respectively). A massive collateral network, predominantly through the internal mammary and intercostal arteries, ensured circulation to the hypoplastic distal aorta (Figure 3C and D).
The patient was asymptomatic, with controlled hypertension and no symptoms of claudication, despite the distal aortic hypoplasia and pressure gradient between upper and lower limbs. The case was considered for surgical repair but, in view of the absence of symptoms, good blood pressure control and effective collateral circulation, a strategy of delayed intervention and close clinical surveillance was chosen.
DiscussionIAA is a rare congenital malformation that occurs in 3/1000000 live births, accounting for 1% of all congenital heart disease.4 It is defined as complete discontinuity of the aortic lumen between the ascending and descending portions of the thoracic aorta. IAA is commonly associated with additional cardiovascular anatomic defects, such as patent ductus arteriosus, ventricular septal defect, bicuspid aortic valve, subaortic stenosis, truncus arteriosus, aortopulmonary window and double outlet right ventricle. Rarely, IAA is an isolated finding without other associated congenital anomalies. A classification system introduced by Celoria and Patton in 19595 divides IAA into three types: type A – interruption distal to the LSA; type B – interruption between the left common carotid artery and the LSA; and type C – interruption between the brachiocephalic trunk and the left common carotid arteries. In infants, type B is the most common (53%), whereas in adults type A has been more often reported.
Almost all cases of IAA are diagnosed in early childhood or the neonatal period, and clinical presentation involves severe congestive heart failure. If left untreated, 90% of affected infants die in the first year of life,6 the majority in the first few days due to the spontaneous closure of the ductus arteriosus. Consequently, IAA is only very rarely diagnosed in adult patients, and few cases of persons having reached adulthood with IAA have been reported in the literature.4,6–10 Survival into adulthood relies on the development of an extensive collateral network, which is essential for the maintenance of distal flow and which is able to develop when there is a patent ductus arteriosus which closes gradually. It is also thought that in some cases the initial defect could be coarctation of the aorta, which evolves to complete obstruction of the lumen6; type A IAA and severe cases of aortic coarctation may show close anatomic and clinical similarities. Aortic coarctation occurs far more frequently and accounts for 8% of all congenital heart defects. In severe cases, progression of luminal stenosis to complete obstruction has been reported.3 In our patient, the morphology and location of the aortic obstruction distal to the left subclavian artery raises the possibility that an undiagnosed coarctation could have evolved into occlusion.
Clinical presentation of IAA in adults varies from absence of symptoms to hypertension, headache, malaise, differential blood pressure between arms and legs, claudication, limb swelling and congestive heart failure. Most patients have refractory hypertension since adolescence or early adulthood. However, some may reach adulthood asymptomatic or with mild hypertension. Less symptomatic patients are often diagnosed by chance or when the etiology of hypertension is being investigated.7 Aneurysmal dilatation of the ascending aorta or aortic valve regurgitation, particularly with bicuspid aortic valve, are other common findings in adults with IAA.
A careful physical examination provides the first clue to the diagnosis of IAA or aortic coarctation and is of utmost importance in all young adults with hypertension. Lower systolic blood pressure in the lower than in the upper limbs and/or a delay or decrease in amplitude of femoral pulses compared to brachial or carotid pulses should raise the suspicion of coarctation or interruption of the aorta. Unlike coarctation, in IAA there is no audible systolic murmur of blood flow across the constriction, because there is a complete interruption of flow between the proximal and distal parts of the aorta. However, continuous murmurs of the collateral vessels may be heard over the parasternal or scapular areas; occasionally, periscapular collaterals can be palpated. Notching on the underside of the ribs from collateral vessels may be apparent on chest radiography. The diagnosis of IAA must be confirmed with an imaging method, such as echocardiography, computed tomography, magnetic resonance imaging or conventional angiography.
The definitive treatment of IAA is surgical correction. Depending on the anatomy and location of the aortic interruption, surgical repair may be accomplished by extra-anatomic bypass, interposition of a tube graft or end-to-end anastomosis. The most frequently described surgical approach in adults is a single-stage repair by means of an extra-anatomic approach.8,9 A two-stage approach has also been described for treatment of patients with additional cardiovascular lesions or in order to minimize the risk of bleeding; however, a positive significant effect of staged operations on mortality and morbidity has not been proven.10 Conventional repair of IAA by end-to-end anastomosis, as for coarctation, is often a surgical challenge in adults, due to insufficient mobilization of the ascending and descending aorta and to the extensive collateral vessels that develop on the chest wall and inside the chest cavity.9 In our case, the most likely surgical approach would be interposition of a tube graft. However, at present it was decided to postpone surgery because the patient is completely asymptomatic and normotensive. A close clinical follow-up is being maintained.
Perhaps the most important message of this case report is that a careful physical examination has a pivotal role in the assessment of patients with hypertension. Palpation of the brachial and femoral arterial pulses and blood pressure measurement in the four limbs are essential for diagnosis of some forms of secondary hypertension. Our patient had had hypertension since the age of 25, but it was only investigated after he suffered an intracranial hemorrhage due to rupture of a cerebral aneurysm. Even then he was misdiagnosed as having essential hypertension, and the correct diagnosis was established only seven years later. A complete physical examination would have ensured the correct diagnosis was made much earlier.
Coarctation of the aorta and IAA can be easily diagnosed by physical examination. Nevertheless, reports and studies of aortic coarctation patients have shown that the diagnosis is often missed by the referring doctor and that, as a consequence, a significant number of asymptomatic subjects are probably not detected until adult life.3
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.