A 46-year-old man with longstanding constitutional symptoms was admitted with sepsis and acute respiratory failure. He had undergone hematopoietic stem cell transplantation (HSCT) and was under immunosuppressive therapy due to graft-versus-host disease (GVHD).
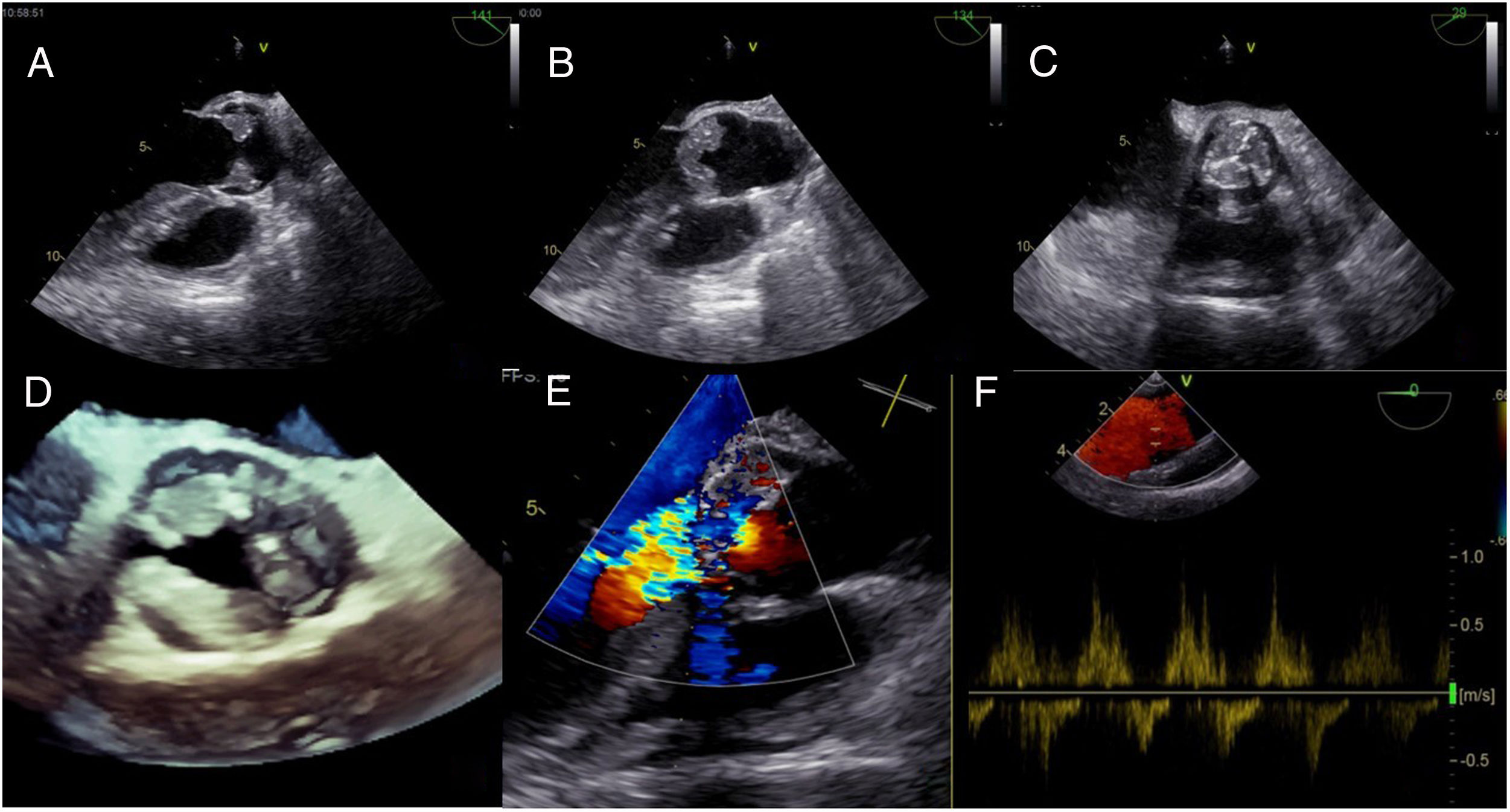
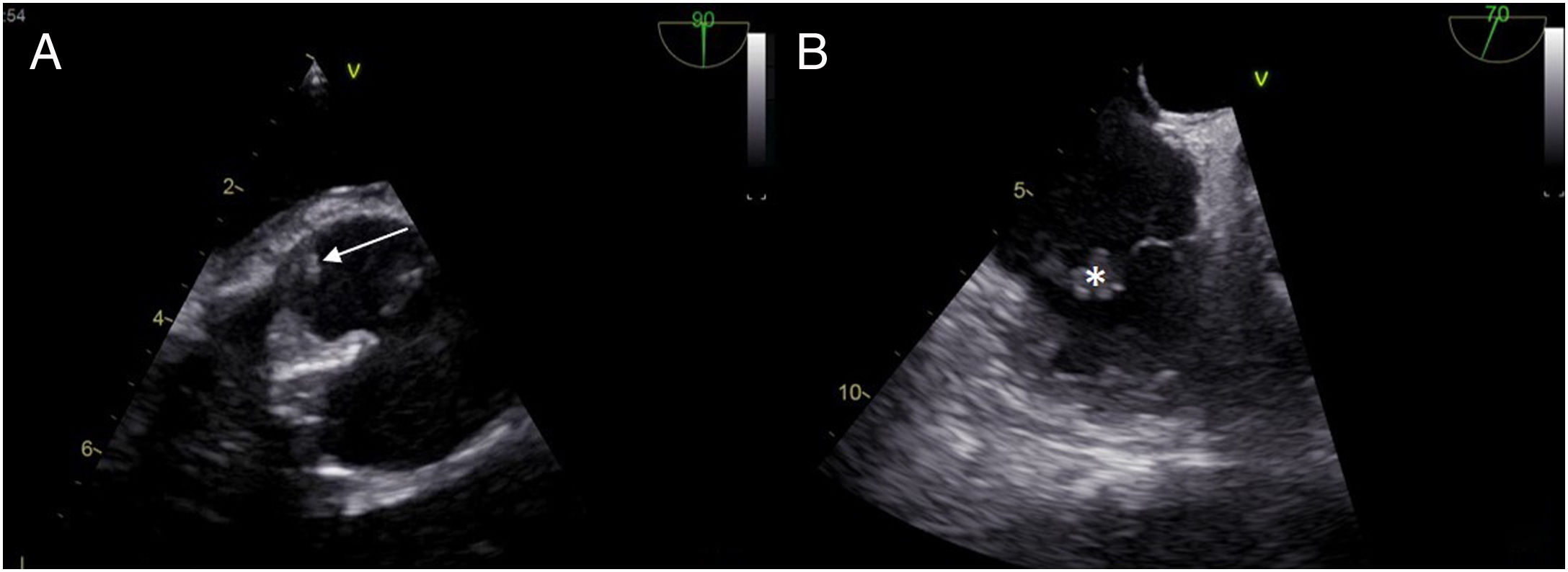
Lung nocardiosis was diagnosed and he was put on imipenem and trimethoprim-sulfamethoxazole. Despite effective treatment, the patient presented recurrent fever. Transesophageal echocardiography documented exuberant multinodular vegetations involving all cusps of the aortic valve (maximum width 10 mm×12 mm) (Figure 1A and B and Video 1), in a pattern resembling the Mercedes-Benz symbol (Figure 1C and D), causing severe aortic regurgitation (Figure 1E and F; Video 2). Vegetations were also seen in the non-coronary sinus of Valsalva (Figure 2A, arrow) and on the tricuspid valve (Figure 2B, asterisk). Aortic valve replacement was performed and no vegetations were found on the tricuspid valve. Blood cultures were persistently negative, as were microbiological analysis of the surgical specimen and serology for atypical agents. The patient eventually died due to neurological complications.
Infective endocarditis (IE) has been reported infrequently in HSCT recipients; GVHD is a risk factor. Although uncommon, Nocardia sp. was considered the most likely causative agent in view of the clinical context and imaging. The fastidious growth pattern of this bacterium and previous antibiotic therapy could explain the negative results of microbiological exams. Multimodality echocardiography, including transthoracic and transesophageal echocardiography and three-dimensional imaging, plays a central role in the diagnosis of IE, especially in complex infections. It offers a virtual preoperative perspective of the disease process that is crucial to surgical planning and patient outcome.
Conflicts of interestThe authors have no conflicts of interest to declare.