Atrial fibrillation (AF) is widely recognized as an adverse prognostic factor during acute myocardial infarction, although the impact of AF type – new-onset (nAF) or pre-existing (pAF) – is still controversial.
ObjectivesTo identify the clinical differences and prognosis of nAF and pAF during acute coronary syndromes (ACS).
MethodsWe performed a retrospective observational cohort study including 1373 consecutive patients (mean age 64 years, 77.3% male) admitted to a single center over a three-year period, with a six-month follow-up.
ResultsAF rhythm was identified in 14.5% patients, of whom 71.4% presented nAF and 28.6% pAF. When AF types were compared, patients with nAF more frequently presented with ST-elevation ACS (p=0.003). Patients with pAF, in turn, were older (p=0.032), had greater left atrial diameter (p=0.001) and were less likely to have significant coronary lesions (p=0.034). Regarding therapeutic strategy, nAF patients were more often treated by rhythm control during hospital stay (p<0.001) and were less often anticoagulated at discharge (p=0.001). Compared with the population without AF, nAF was a predictor of death during hospital stay in univariate (p<0.001) and multivariate analysis (OR 2.67, p=0.047), but pAF was not. During follow-up, pAF was associated with higher mortality (p=0.014), while nAF patients presented only a trend towards worse prognosis.
ConclusionsAF during the acute phase of ACS appears to have a negative prognostic impact only in patients with nAF and not in those with pAF.
A fibrilhação auricular (FA) é um reconhecido fator de mau prognóstico no enfarte agudo do miocárdio, no entanto, o impacto do tipo de FA, de novo (FAn) ou pré-existente (FAp), é ainda controverso.
ObjetivosIdentificar as diferenças clínicas e o prognóstico da FAn e da FAp nas síndromes coronárias agudas (SCA).
MétodosEstudo retrospetivo observacional de coorte, incluindo 1373 doentes consecutivos (idade média 64 anos, 77,3% homens) com SCA, admitidos num hospital, ao longo de três anos, com follow-up de seis meses.
ResultadosA FA foi identificada em 14,5% doentes, dos quais 71,4% tinham FAn e 28,6% FAp. Comparando os tipos de FA, verificou-se que os doentes com FAn apresentaram mais frequentemente SCA com elevação do segmento ST (p=0,003). Por sua vez, a FAp foi mais comum em doentes idosos (p=0,032), com diâmetro superior da aurícula esquerda (p=0,001) e ausência de doença coronária (p=0,034). Quanto à estratégia terapêutica, os doentes com FAn foram mais vezes submetidos a controlo de ritmo durante o internamento (p<0,001), mas menos hipocoagulados à alta (p=0,001). Quando comparada com a população sem FA, a FAn foi preditora de morte hospitalar na análise univariada (p<0,001) e multivariada (OR 2,67, p=0,047), enquanto a FAp não. Já no follow-up, a FAp associou-se a maior mortalidade (p=0,014), enquanto os doentes com FAn apresentaram apenas uma tendência para um pior prognóstico.
ConclusõesO impacto prognóstico negativo da FA na fase aguda das SCA parece ocorrer apenas nos doentes que apresentam FAn e não naqueles com FAp.
Atrial fibrillation (AF) frequently complicates the clinical course of acute myocardial infarction (AMI), with a reported incidence between 6 and 21%.1 Although this arrhythmia is a well-established independent predictor of mortality in the short and long term after AMI,2–4 the impact of the specific AF type – new-onset or pre-existing – may be different. Few published studies have been conducted regarding this question and the results are conflicting.2,5–11 In a recent meta-analysis, Angeli et al.12 showed that AF in the setting of AMI was associated with a two-fold higher risk of in-hospital mortality, but the risk of death was 87% higher in patients with new-onset AF than in those with permanent AF.
The primary aim of this study was to identify the clinical differences and prognostic impact of AF type during acute coronary syndromes (ACS).
MethodsThis was a retrospective observational cohort study with a six-month follow-up. All patients (n=1373; mean age 64 years, 77.3% male) consecutively admitted to the coronary care unit of a single center with a diagnosis of ACS between July 2009 and June 2012 were included.
Diagnoses of ACS and AF were made according to the European Society of Cardiology guidelines.13–16 Heart failure was defined as Killip class ≥2 during hospitalization and as NYHA class ≥2 during follow-up. Patients with AF were divided according to the timing of the arrhythmia: every patient who presented with AF for the first time (i.e., who did not have previously documented AF) at admission or during hospital stay was considered to have new-onset AF, while those with previously documented AF were classified as having pre-existing AF (paroxysmal, persistent or permanent).
Regarding AF management, a rhythm control strategy was defined as the aim of restoration and successful maintenance of sinus rhythm and rate control strategy as acceptance of AF rhythm with ventricular rate control. The use of oral anticoagulation and antiarrhythmic therapy (amiodarone) at discharge was also assessed. The management of each patient was individualized and based on clinical parameters.
Demographic, clinical, laboratory, echocardiographic and coronary angiographic data were collected prospectively and recorded in a computerized database, in accordance with our department's protocol for patients admitted to the coronary care unit with ACS.
Concerning laboratory data, N-terminal pro-brain natriuretic peptide (NT-proBNP) values were obtained within 24 hours of admission and peak creatinine was considered to be the maximum value during hospitalization. Glomerular filtration rate was calculated at presentation using the abbreviated Modification of Diet in Renal Disease formula.17
The first echocardiogram performed in hospital was used to provide echocardiographic data. Right ventricular systolic dysfunction was defined as tricuspid annular systolic excursion >16 mm.
Coronary angiographic data were collected from angiography performed during hospital stay. Significant coronary artery disease on coronary angiography was defined as at least one ≥50% lesion in the left main artery and/or ≥70% in other coronary arteries. Multivessel disease was defined as significant stenosis in two or more major epicardial arteries and coronary revascularization as successful percutaneous or surgical coronary intervention to restore blood flow.
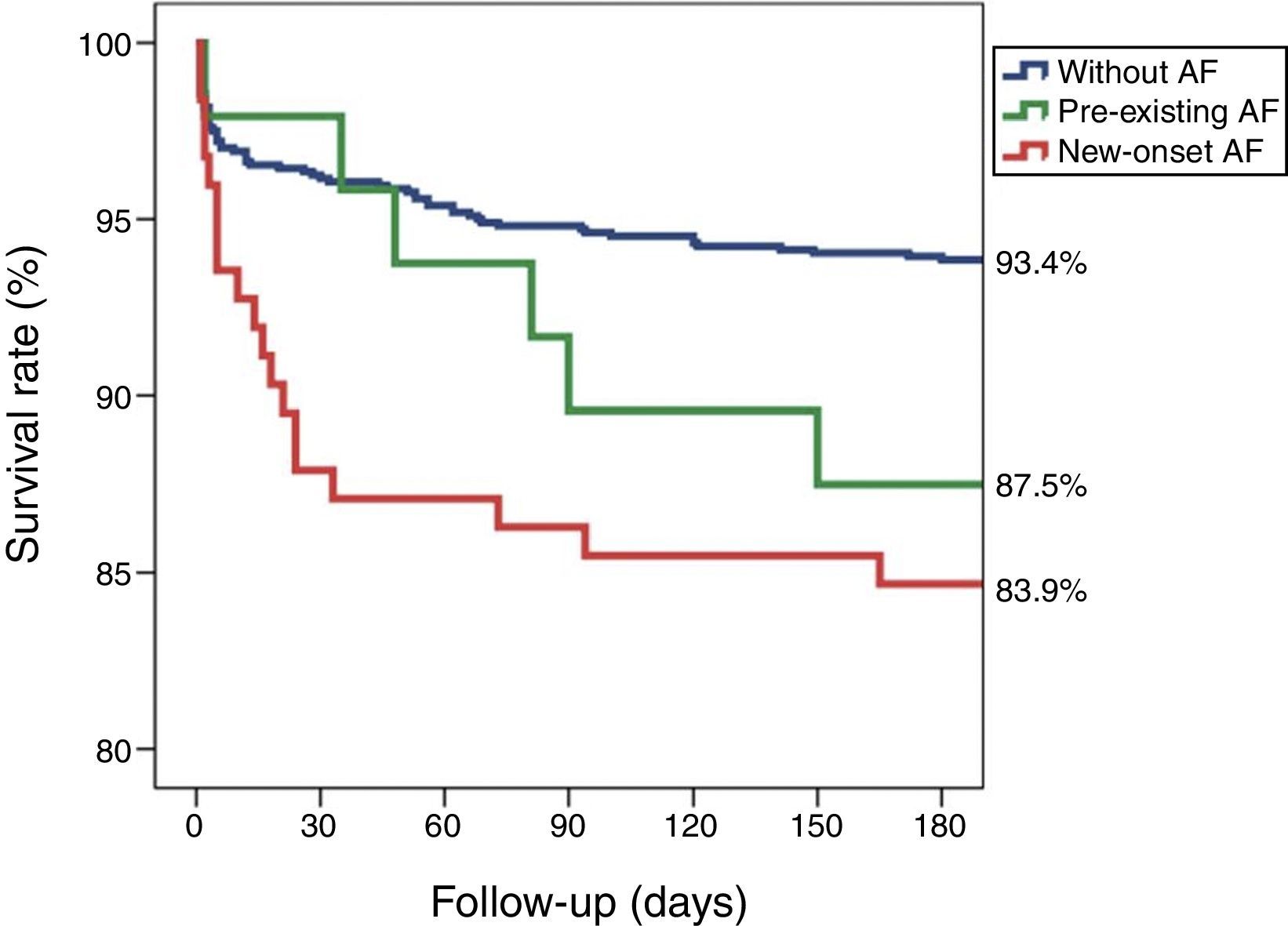
Statistical analysisUnivariate analysis of categorical variables was performed using the chi-square test, with results expressed as percentages, and of continuous variables using the Student's t test, with results expressed as means ± standard deviation. Analysis of the therapeutic strategy used to manage AF was performed after exclusion of patients who died during hospital stay. Multivariate logistic analysis was performed to determine the independent predictors of in-hospital mortality, including only variables with statistical significance on univariate analysis. Kaplan-Meier analysis was used to illustrate six-month cumulative mortality according to the presence of AF and AF type. Differences with p<0.05 were considered significant. The statistical analysis was carried out using SPSS version 18.0.
ResultsIn the study population (n=1373), AF rhythm was identified in 14.5% patients (n=199), of whom 71.4% (n=142) presented new-onset AF and 28.6% (n=57) pre-existing AF. Patients with new-onset AF, pre-existing AF and without AF were studied according to their baseline characteristics, in-hospital features and clinical outcomes.
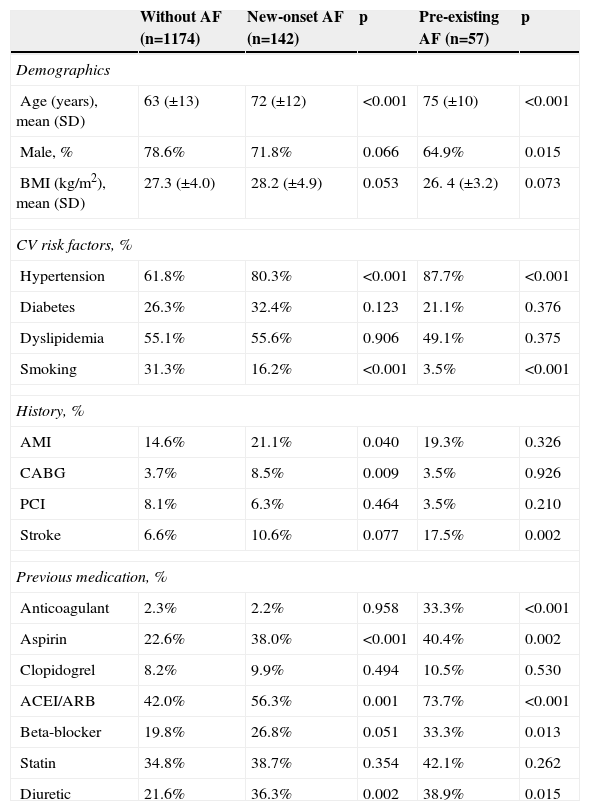
Baseline characteristics and in-hospital dataNew-onset AF and pre-existing AF patients were compared with those without AF. The baseline characteristics of the study population are shown in Table 1.
Baseline clinical characteristics of patients without AF compared with those with new-onset and pre-existing AF.
| Without AF (n=1174) | New-onset AF (n=142) | p | Pre-existing AF (n=57) | p | |
|---|---|---|---|---|---|
| Demographics | |||||
| Age (years), mean (SD) | 63 (±13) | 72 (±12) | <0.001 | 75 (±10) | <0.001 |
| Male, % | 78.6% | 71.8% | 0.066 | 64.9% | 0.015 |
| BMI (kg/m2), mean (SD) | 27.3 (±4.0) | 28.2 (±4.9) | 0.053 | 26. 4 (±3.2) | 0.073 |
| CV risk factors, % | |||||
| Hypertension | 61.8% | 80.3% | <0.001 | 87.7% | <0.001 |
| Diabetes | 26.3% | 32.4% | 0.123 | 21.1% | 0.376 |
| Dyslipidemia | 55.1% | 55.6% | 0.906 | 49.1% | 0.375 |
| Smoking | 31.3% | 16.2% | <0.001 | 3.5% | <0.001 |
| History, % | |||||
| AMI | 14.6% | 21.1% | 0.040 | 19.3% | 0.326 |
| CABG | 3.7% | 8.5% | 0.009 | 3.5% | 0.926 |
| PCI | 8.1% | 6.3% | 0.464 | 3.5% | 0.210 |
| Stroke | 6.6% | 10.6% | 0.077 | 17.5% | 0.002 |
| Previous medication, % | |||||
| Anticoagulant | 2.3% | 2.2% | 0.958 | 33.3% | <0.001 |
| Aspirin | 22.6% | 38.0% | <0.001 | 40.4% | 0.002 |
| Clopidogrel | 8.2% | 9.9% | 0.494 | 10.5% | 0.530 |
| ACEI/ARB | 42.0% | 56.3% | 0.001 | 73.7% | <0.001 |
| Beta-blocker | 19.8% | 26.8% | 0.051 | 33.3% | 0.013 |
| Statin | 34.8% | 38.7% | 0.354 | 42.1% | 0.262 |
| Diuretic | 21.6% | 36.3% | 0.002 | 38.9% | 0.015 |
ACEI: angiotensin-converting enzyme inhibitor; AF: atrial fibrillation; AMI: acute myocardial infarction; ARB: angiotensin receptor blocker; BMI: body mass index; CABG: coronary artery bypass grafting; CV: cardiovascular; PCI: percutaneous coronary intervention; SD: standard deviation.
AF, either new-onset or pre-existing, was more frequent in older, non-smoking and hypertensive patients. Although the proportion of women was higher in both AF types than in patients without AF, the difference was only significant for those with pre-existing AF (p=0.015). AF patients had greater cardiovascular disease burden and were more likely to be taking cardiovascular medication at presentation, as demonstrated in Table 1.
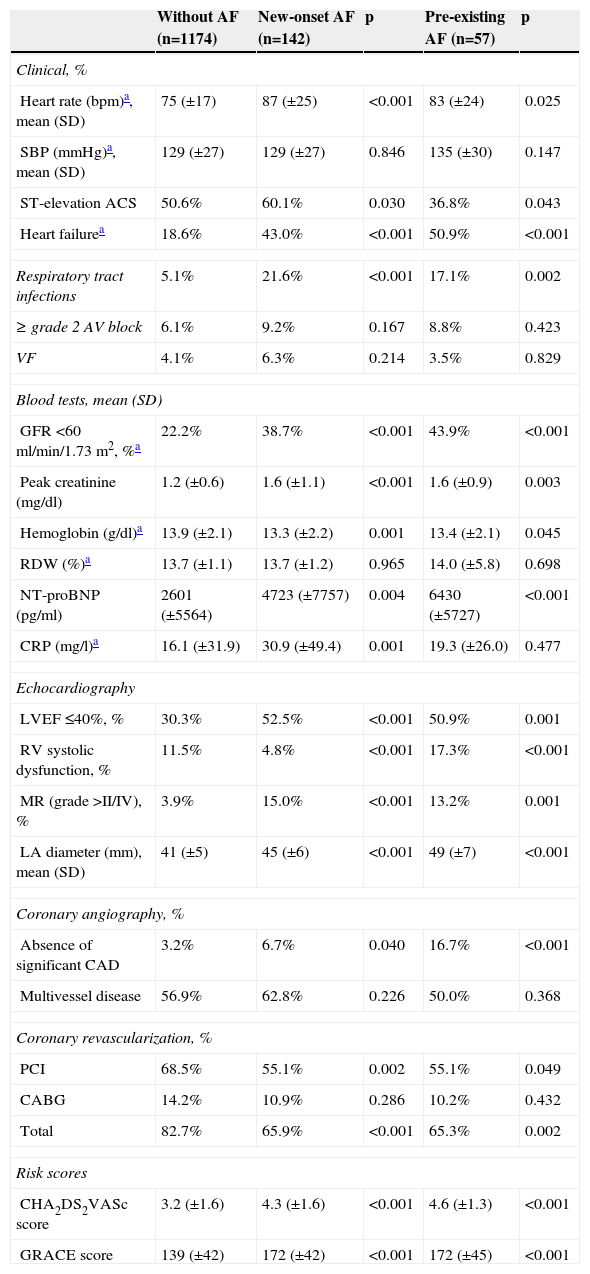
Clinical information during hospital stay and laboratory, echocardiographic, coronary angiographic and revascularization data are summarized in Table 2.
Clinical, laboratory, echocardiographic, coronary angiographic, and revascularization data and risk scores during hospital stay of patients without AF compared with those with new-onset and pre-existing AF.
| Without AF (n=1174) | New-onset AF (n=142) | p | Pre-existing AF (n=57) | p | |
|---|---|---|---|---|---|
| Clinical, % | |||||
| Heart rate (bpm)a, mean (SD) | 75 (±17) | 87 (±25) | <0.001 | 83 (±24) | 0.025 |
| SBP (mmHg)a, mean (SD) | 129 (±27) | 129 (±27) | 0.846 | 135 (±30) | 0.147 |
| ST-elevation ACS | 50.6% | 60.1% | 0.030 | 36.8% | 0.043 |
| Heart failurea | 18.6% | 43.0% | <0.001 | 50.9% | <0.001 |
| Respiratory tract infections | 5.1% | 21.6% | <0.001 | 17.1% | 0.002 |
| ≥ grade 2 AV block | 6.1% | 9.2% | 0.167 | 8.8% | 0.423 |
| VF | 4.1% | 6.3% | 0.214 | 3.5% | 0.829 |
| Blood tests, mean (SD) | |||||
| GFR <60 ml/min/1.73 m2, %a | 22.2% | 38.7% | <0.001 | 43.9% | <0.001 |
| Peak creatinine (mg/dl) | 1.2 (±0.6) | 1.6 (±1.1) | <0.001 | 1.6 (±0.9) | 0.003 |
| Hemoglobin (g/dl)a | 13.9 (±2.1) | 13.3 (±2.2) | 0.001 | 13.4 (±2.1) | 0.045 |
| RDW (%)a | 13.7 (±1.1) | 13.7 (±1.2) | 0.965 | 14.0 (±5.8) | 0.698 |
| NT-proBNP (pg/ml) | 2601 (±5564) | 4723 (±7757) | 0.004 | 6430 (±5727) | <0.001 |
| CRP (mg/l)a | 16.1 (±31.9) | 30.9 (±49.4) | 0.001 | 19.3 (±26.0) | 0.477 |
| Echocardiography | |||||
| LVEF ≤40%, % | 30.3% | 52.5% | <0.001 | 50.9% | 0.001 |
| RV systolic dysfunction, % | 11.5% | 4.8% | <0.001 | 17.3% | <0.001 |
| MR (grade >II/IV), % | 3.9% | 15.0% | <0.001 | 13.2% | 0.001 |
| LA diameter (mm), mean (SD) | 41 (±5) | 45 (±6) | <0.001 | 49 (±7) | <0.001 |
| Coronary angiography, % | |||||
| Absence of significant CAD | 3.2% | 6.7% | 0.040 | 16.7% | <0.001 |
| Multivessel disease | 56.9% | 62.8% | 0.226 | 50.0% | 0.368 |
| Coronary revascularization, % | |||||
| PCI | 68.5% | 55.1% | 0.002 | 55.1% | 0.049 |
| CABG | 14.2% | 10.9% | 0.286 | 10.2% | 0.432 |
| Total | 82.7% | 65.9% | <0.001 | 65.3% | 0.002 |
| Risk scores | |||||
| CHA2DS2VASc score | 3.2 (±1.6) | 4.3 (±1.6) | <0.001 | 4.6 (±1.3) | <0.001 |
| GRACE score | 139 (±42) | 172 (±42) | <0.001 | 172 (±45) | <0.001 |
ACS: acute coronary syndrome; AF: atrial fibrillation; AV: atrioventricular; CABG: coronary artery bypass grafting; CAD: coronary artery disease; CRP: C-reactive protein; GFR: glomerular filtration rate; LA: left atrial; LVEF: left ventricular ejection fraction; MR: mitral regurgitation; NT-proBNP: N-terminal pro-brain natriuretic peptide; PCI: percutaneous coronary intervention; RDW: red blood cell distribution width; RV: right ventricular; SBP: systolic blood pressure; SD: standard deviation; VF: ventricular fibrillation.
At admission, patients with new-onset and pre-existing AF had higher heart rate and worse Killip class. No differences were found in systolic blood pressure. Interestingly, ACS severity was related to AF type: ST-elevation ACS incidence was higher in new-onset AF (60.1%, p=0.030), intermediate in the AF-free group (50.6%) and lower in pre-existing AF (36.8%, p=0.043).
During hospitalization, the presence of AF, regardless of type, was associated with worse clinical, laboratory and echocardiographic features. Patients with AF were more likely to have heart failure, lower glomerular filtration rate, higher peak creatinine, lower hemoglobin and higher NT-proBNP. Additionally, patients with AF more often presented biventricular systolic dysfunction, higher mitral regurgitation grade and greater left atrial diameter. Although the incidence of respiratory tract infections was higher in AF groups, only new-onset AF patients had significantly higher C-reactive protein levels than patients without AF. No differences between non-AF and AF groups were found regarding other arrhythmic complications, such as high grade atrioventricular block or ventricular fibrillation.
The presence of multivessel disease was similar between groups. Patients with new-onset AF and pre-existing AF were less likely to have significant coronary lesions or to have undergone coronary revascularization, the latter due to the lower number of percutaneous coronary interventions (PCI) performed.
The thromboembolic risk score CHA2DS2VASc and the GRACE score were higher in patients with new-onset and pre-existing AF than in patients without AF.
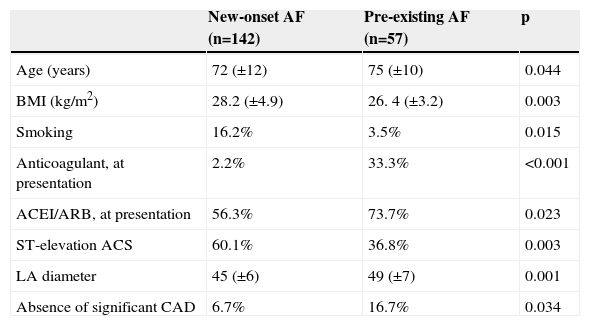
Comparison between atrial fibrillation typesThe clinical and in-hospital differences with statistical significance between new-onset AF and pre-existing AF groups are displayed in Table 3. Patients with new-onset AF were younger (p=0.044), more often smokers (p=0.015) and had higher body mass index (p=0.003). Concerning medication at admission, naturally, patients with pre-existing AF were more frequently taking anticoagulants (p<0.001) and renin-angiotensin system modulators (p=0.023). As pointed out earlier, in contrast to pre-existing AF, the majority of new-onset AF patients presented with ST-elevation ACS (60.1% vs. 36.8%, respectively, p=0.003). Although left atrial enlargement was common in both AF types, left atrial diameter on echocardiography was significantly greater in pre-existing AF (p=0.001). In coronary angiography, absence of significant coronary artery disease was observed more in pre-existing AF (p=0.034).
Differences between new-onset AF and pre-existing AF.
| New-onset AF (n=142) | Pre-existing AF (n=57) | p | |
|---|---|---|---|
| Age (years) | 72 (±12) | 75 (±10) | 0.044 |
| BMI (kg/m2) | 28.2 (±4.9) | 26. 4 (±3.2) | 0.003 |
| Smoking | 16.2% | 3.5% | 0.015 |
| Anticoagulant, at presentation | 2.2% | 33.3% | <0.001 |
| ACEI/ARB, at presentation | 56.3% | 73.7% | 0.023 |
| ST-elevation ACS | 60.1% | 36.8% | 0.003 |
| LA diameter | 45 (±6) | 49 (±7) | 0.001 |
| Absence of significant CAD | 6.7% | 16.7% | 0.034 |
ACEI: angiotensin-converting enzyme inhibitor; ACS: acute coronary syndrome; ARB: angiotensin receptor blocker; BMI: body mass index; CAD: coronary artery disease; LA: left atrial.
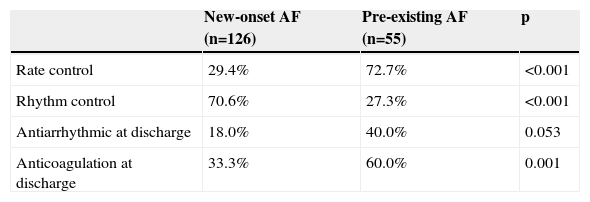
Regarding management strategies, new-onset AF patients were more often treated by rhythm control during hospital stay (p<0.001) than pre-existing AF patients, as shown in Table 4. Patients with pre-existing AF treated by rhythm control were more likely to be prescribed antiarrhythmic therapy to maintain sinus rhythm, although without significance. At discharge, new-onset AF patients were less often anticoagulated than those with pre-existing AF (p<0.001).
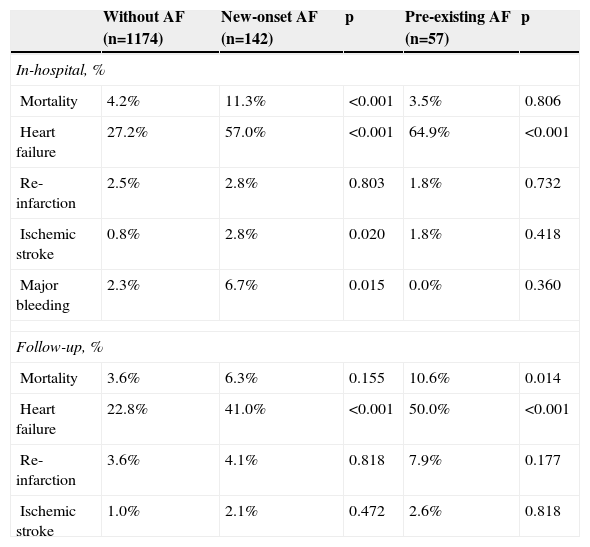
Prognostic impact of atrial fibrillation typeNew-onset AF was associated with significantly worse in-hospital adverse outcomes of death, heart failure, ischemic stroke and major bleeding compared to patients with no arrhythmia, as demonstrated in Table 5. Except for heart failure, such associations were not present in the group with pre-existing AF.
In-hospital and follow-up adverse outcomes: comparison between patients without AF with new-onset and pre-existing AF groups.
| Without AF (n=1174) | New-onset AF (n=142) | p | Pre-existing AF (n=57) | p | |
|---|---|---|---|---|---|
| In-hospital, % | |||||
| Mortality | 4.2% | 11.3% | <0.001 | 3.5% | 0.806 |
| Heart failure | 27.2% | 57.0% | <0.001 | 64.9% | <0.001 |
| Re-infarction | 2.5% | 2.8% | 0.803 | 1.8% | 0.732 |
| Ischemic stroke | 0.8% | 2.8% | 0.020 | 1.8% | 0.418 |
| Major bleeding | 2.3% | 6.7% | 0.015 | 0.0% | 0.360 |
| Follow-up, % | |||||
| Mortality | 3.6% | 6.3% | 0.155 | 10.6% | 0.014 |
| Heart failure | 22.8% | 41.0% | <0.001 | 50.0% | <0.001 |
| Re-infarction | 3.6% | 4.1% | 0.818 | 7.9% | 0.177 |
| Ischemic stroke | 1.0% | 2.1% | 0.472 | 2.6% | 0.818 |
AF: atrial fibrillation.
Together with glomerular filtration rate in ml/min/1.73 m2 (odds ratio [OR] 0.97, 95% confidence interval [CI] 0.95–0.99, p=0.010), heart failure (OR 3.80, 95% CI 1.22–11.86, p=0.022) and ventricular fibrillation (OR 5.42, 95% CI 1.29–22.87, p=0.021), new-onset AF remained an independent predictor of in-hospital mortality, carrying a risk 2.67 times higher than in the group without AF (95% CI 1.01–7.02, p=0.047).
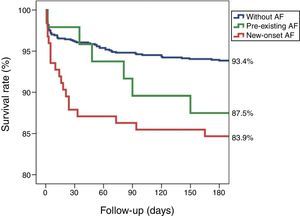
During follow-up (mean 218±92 days), heart failure occurred more frequently in AF groups than in patients without AF. Mortality was higher in pre-existing (p=0.014) but not in new-onset AF, although the latter was associated with a trend towards higher mortality (6.3% vs. 3.6%, p=0.155). No differences were found regarding reinfarction or ischemic stroke during follow-up.
Kaplan-Meier survival curves (Figure 1) illustrate a trend towards worse prognosis for both AF groups compared with no arrhythmia, with significance for new-onset AF (log rank p<0.001) but not for pre-existing AF (log rank p=0.120).
Patients with new-onset AF discharged in sinus rhythm and followed in the outpatient clinic of our hospital (n=33) had a longer follow-up (mean 557±381 days). The recurrence rate of AF in this subgroup during follow-up was 24.2% (n=8).
DiscussionRecently, our group reported that patients with new-onset AF in the context of ACS had worse clinical manifestations and adverse prognostic implications during hospitalization and throughout follow-up.18 Questions regarding the clinical features and prognostic impact of different AF types, new-onset or pre-existing, remained unanswered. The present study included a larger number of patients, allowing direct comparison between new-onset and pre-existing AF.
First, regardless of type, patients with AF presented high-risk clinical features during hospitalization, such as older age, heart and renal failure, respiratory tract infections, lower hemoglobin, higher NT-proBNP, biventricular dysfunction, significant mitral regurgitation, less coronary revascularization and higher GRACE risk score. The bulk of evidence clearly demonstrates that the presence of AF in itself during ACS is associated with worse in-hospital outcomes.1,2,7,19,20 The pathophysiological mechanisms underlying this relation may differ according to the timing of the arrhythmia. It is well known that acute AF complicating ACS is proportional to the grade of ischemia and has a negative effect on coronary perfusion and cardiac hemodynamics,2 and is a marker of larger area of necrosis.5,21 In contrast, pre-existing AF patients usually have greater cardiovascular disease burden and more structural heart disease owing to the longer duration of the arrhythmia.7 Indeed, in our study, patients with pre-existing AF were older, more likely to be taking cardiovascular medications at admission and had greater left atrial diameter on echocardiography than patients with new-onset AF.
Second, unlike in previous studies,5–7 the most frequently encountered type was new-onset AF, which was found in more than two-thirds of AF patients. This could be due to a bias related to the definition used, since patients without AF history who were admitted in AF rhythm were labeled as new-onset AF, although the timing in such cases could not be determined with certainty and, as such, they could have been misclassified. Regarding management, the majority of these patients promptly and successfully returned to sinus rhythm during hospitalization, which favors correct classification as new-onset AF.
Third, in our study, the main differences at presentation between AF types were related to ACS severity, left atrial diameter and coronary angiography details. As pointed out above,7,18 ST-segment elevation ACS is a predictor of new-onset AF, probably because the myocardial ischemic burden, and hence the arrhythmogenic substrate, are greater in this subgroup.9 The pathogenesis of AF in this context is multifactorial and may include atrial ischemia or infarction, ventricular dysfunction, pericardial inflammation, acute hypoxia, ionic disturbances, and neurohormonal and autonomic nervous system activation.22–24 Left atrial diameter was significantly greater in pre-existing AF patients, reflecting the progressive atrial dilatation and myocardial remodeling that occurs with AF evolution. It may represent a marker of arrhythmia duration, acting as a substrate for AF initiation and maintenance.10 Significant coronary artery disease on coronary angiography was more often absent in both subtypes, although in a higher proportion in pre-existing AF patients. In fact, AF can predispose to AMI without atherosclerotic plaque rupture through two mechanisms: coronary occlusion by a thromboembolic event or a mismatch between myocardial oxygen supply and demand caused by the elevated and irregular heart rate.14,25 We hypothesize that AF type might be a marker of the pathophysiologic mechanism underlying myocardial infarction: probably, acute plaque rupture is more common in new-onset AF and thromboembolism in pre-existing AF.
Fourth, short- and long-term prognosis differed according to AF type. New-onset AF conferred worse clinical outcomes and prognosis during hospital stay, while pre-existing AF was associated with mortality during follow-up, similar findings to the data published by Lau et al.7 The link between new-onset AF and ST-segment elevation ACS may in part explain the worse in-hospital prognosis. Unlike pre-existing AF, which does not imply an acute change in hemodynamic status and is therefore not associated with worse prognosis during hospitalization for ACS, new-onset AF acutely compromises hemodynamic status and, as such, implies worse clinical in-hospital course. In contrast, long-term mortality is higher in pre-existing AF, reflecting the existence of chronic structural and functional heart disease.26 Studies on the effect of AF type on prognosis after myocardial infarction show conflicting results.2,5–11 The heterogeneity of patients included in each study, and the substantial improvement in ACS treatment in recent years with the widespread use of PCI and the emergence of new drug therapies, could explain the dissimilarities in the clinical impact of AF type.
Finally, in our study, successful AF rhythm management predominated in patients with new-onset AF and rate control strategy was preferred in patients with pre-existing AF, as would be expected, since the latter were older and had larger left atrial diameter, recognized factors for AF recurrence, or were already on rate control for permanent AF. Regarding antithrombotic therapy at discharge, theoretically, patients with pre-existing AF should have been medicated with oral anticoagulation, since they all had CHA2DS2VASc scores ≥2. Unlike primary AF, the anticipated bleeding risk is higher in post-ACS patients due to the concomitant use of dual antiplatelet therapy, which is recommended by the current guidelines for at least one month and ideally up to one year after ACS.13 While triple antithrombotic therapy appears to be safe and effective in the short term (30 days), prolonged triple therapy (one year) is associated with an excessive major bleeding risk.27–29 We reported that 40% of patients with pre-existing AF did not receive anticoagulation at discharge. The occurrence of bleeding complications during hospitalization and the presence of high bleeding risk were the main factors that precluded triple antithrombotic therapy. Lopes et al.,30 in a large registry including 69 225 patients with AMI, found similar results, showing that fewer than 50% of patients with pre-existing AF received warfarin and only 14.6% were treated with triple antithrombotic therapy at discharge. In routine practice and in contrast to recommendations, older patients with AF and ACS who undergo PCI are more likely to receive dual antiplatelet therapy rather than triple antithrombotic therapy.31,32 In the WOEST trial,33 the use of clopidogrel without aspirin in patients receiving concomitant oral anticoagulants and undergoing PCI was associated with a significant reduction in bleeding complications and no increase in the rate of thrombotic events within one year of intervention, posing the question whether high bleeding risk patients with ACS should be treated with single antiplatelet therapy plus anticoagulation. In our study, patients with new-onset AF were even less likely to be discharged with anticoagulation (only one third). In contrast to patients with pre-existing AF, the approach to anticoagulation in those with new-onset AF during ACS is far less clear. Studies report a non-negligible recurrence rate of new-onset AF that varies between 10 and 34%,34–37 a similar value to the 24.2% we described in the subgroup of patients discharged in sinus rhythm followed in our outpatient clinic. Asanin et al.37 found that AF recurred more frequently soon after hospital discharge (<3 months) in patients who had longer duration AF episodes (>3.5 hours) within 48 hours of myocardial infarction. Furthermore, patients with new-onset AF are also more likely to suffer stroke during follow-up. Zusman et al.35 reported an annual incidence of ischemic stroke of 4.4% vs. 0.2% in the non-AF group, and Siu et al.34 found incidences of 10.2% and 7.5%, respectively, during the first and second year of follow-up, in patients with transient AF during inferior AMI when they were treated with antiplatelet therapy alone. Asanin et al.37 described some predictors of stroke in patients with a history of new-onset AF, including absence of anticoagulation at discharge, recurrence of AF and heart failure during follow-up. To summarize, although new-onset AF in the setting of ACS can be transient, it should not be regarded as a benign complication of the acute event, since it carries a substantial future risk for recurrence and stroke. Therefore, oral anticoagulation should also be strongly considered in patients with new-onset AF.
LimitationsThere are several limitations to be considered in the interpretation of our study. First, this was a retrospective, observational and non-randomized study conducted at a single hospital, and as such, both identified and unidentified confounders may have influenced the outcomes. As pointed out above, new-onset AF patients could have been misclassified. Second, our results are limited by the relatively small numbers of patients studied with new-onset and pre-existing AF. Finally, most variables were determined by consulting medical records that could have been incomplete.
ConclusionsIn summary, new-onset AF was more common in patients presenting with ST-elevation ACS who had high-risk clinical features and worse prognosis during hospitalization, probably reflecting a greater degree of ischemia. In turn, patients with pre-existing AF had greater mortality throughout follow-up, reflecting the existence of established structural heart disease.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.