Advanced age is, unsurprisingly, one of the most important predisposing factors for adverse drug reactions (ADRs) and ADR-related hospital admissions. Elderly patients are more often on polypharmacy and have more extensive comorbidity, which increase the risk of ADRs through drug-drug or drug-disease interactions and abnormal pharmacokinetics. The higher prevalence of cognitive impairment and functional deficits in this group of patients also impacts on treatment adherence and tolerability. Among elderly patients in particular, ADRs are associated with increased morbidity and mortality.1,2 The most frequent ADRs are typically caused by cardiovascular drugs,3 and a significant percentage of all ADRs involve the cardiovascular system, the most frequent drug-related cardiovascular abnormality probably being bradycardia.4 This is commonly referred to as a type of proarrhythmia. Proarrhythmia can result from a direct effect of the drug on the electrophysiological properties of the conduction system, an abnormal amplification of its effect through drug-drug interactions, or drug-induced metabolic abnormalities. However, although drug-related bradycardia may be seen as a potentially reversible condition likely to subside after discontinuation of the offending drug, a significant percentage of these patients still receive pacemaker implantation during the index admission. Whether this is indeed the right approach in all-comers or just a more cautious, albeit potentially unnecessary one, remains to be determined. The current decision-making process is based on clinical judgment rather than on published guidelines, as little is known about the prognosis of this group of patients.
In this issue of the Journal, Gonçalves et al. present an interesting assessment of the need for permanent pacemaker implantation in elderly patients admitted to hospital due to bradycardia associated with potentially reversible causes such as antiarrhythmic drugs (including beta-blockers) or severe hyperkalemia.5 Their study revealed that more than half of these patients eventually require pacemaker implantation despite discontinuation of the culprit medication and correction of potassium levels. This was particularly true for patients on antiarrhythmic drugs admitted with atrioventricular (AV) conduction abnormalities, while the risk in the setting of sinoatrial dysfunction and/or isolated hyperkalemia was significantly lower.
Although there is little doubt on how to treat persistent severe and/or symptomatic bradycardia (most physicians would agree that pacemaker implantation is the right course of action in most, if not all, of these cases), it remains unclear whether prophylactic pacemaker implantation during the index admission should be offered to patients whose bradycardia resolved after the offending drug was discontinued. The present study offers valuable insight into this matter. The authors’ findings to some extent corroborate the results of the few studies performed to date on this subject and highlight the need for a greater level of attention from physicians caring for these patients. In their assessment of patients with drug-related bradycardia, Lee et al. concluded that, in approximately one quarter of cases, bradycardia persists after discontinuation of the offending drug.6 Similarly, Knudsen et al. reported that 25% of patients who were discharged without a permanent pacemaker subsequently presented with recurrent AV block requiring this treatment.7 Another study revealed that 56% of patients for whom drug discontinuation led to resolution of AV block had recurrence in the absence of antiarrhythmic therapy.8 These studies, together with that of Gonçalves et al., justify Zeltser's comment that AV block is commonly “related to drugs” but is rarely “caused by drugs”.8 Indeed, given the advanced age of most patients admitted due to drug-induced bradycardia, it is probable that antiarrhythmic drugs are simply unmasking underlying conduction system disease that would otherwise have gone unnoticed for some time.
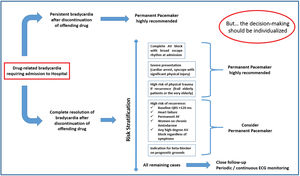
The management of patients for whom drug discontinuation led to resolution of the index bradycardia involves two critical steps: a decision on whether to implant a prophylactic pacemaker during or soon after the index hospitalization; and, for those discharged without a pacemaker, a commitment to close follow-up with periodic and perhaps long-term continuous monitoring. For elderly patients whose bradycardia resolves after drug discontinuation, it is not unreasonable to offer permanent pacemaker implantation when at least one of the following criteria is met:
- •
High risk of recurrent severe and/or symptomatic bradycardia, such as in patients who present with high-degree AV block and have a QRS width ≥120 ms9 (measured after the AV block subsided), or a history of heart failure and/or permanent atrial fibrillation, each of which nearly triples the odds of developing bradycardia requiring pacemaker implantation.10 Also, chronic amiodarone therapy for atrial fibrillation in women, given the long half-life of this drug and the increased risk of pacemaker implantation in elderly women taking this medication11;
- •
History of trauma caused by the proarrhythmia or high risk of sustaining significant physical injury in the event of recurrent bradycardia, which would include a significant percentage of these patients given their advanced age and comorbidity;
- •
Previous indication for beta-blockers on prognostic grounds, for instance those with heart failure or previous myocardial infarction, as discontinuation of this drug could lead to worse outcome.
For patients who do not fulfill any of these criteria, particularly if the baseline arrhythmia involves the sinoatrial node rather than the AV node and the patient was taking a high-dose chronotropic drug (or multiple drugs), a conservative approach with close follow-up is reasonable. Figure 1 provides some general guidance on how to manage these cases, although it should be stressed that common sense must prevail at all times. Formal risk stratification models such as the San Francisco Syncope Rule12 or Risk Stratification of Syncope in the Emergency Department (ROSE)13 score may help identify patients who can safely be discharged after presenting with syncope, but these scores have a very low specificity, which could result in unnecessary treatment or hospitalization for some patients.
It should be emphasized that drug-induced bradycardia is not the only type of drug proarrhythmia of which physicians should be aware. Polymorphic ventricular tachycardia (VT) and torsade de pointes (TdP) due to drug-related acquired long QT syndrome can also be triggered by various medications, including non-cardiovascular drugs, and it should be noted that these conditions are not always truly reversible. Similar to the concept, mentioned above, of unmasking underlying conduction system disease, drug-induced inhibition of the cardiac hERG/IKr potassium channel may lead to QT prolongation and TdP in patients with other repolarization stressors, including bradycardia. As some of the major epidemiological risk factors for QT prolongation and TdP, such as older age, female gender, heart failure, history of myocardial infarction and metabolic abnormalities, are also predictors of bradyarrhythmia in patients on antiarrhythmic therapy, physicians should bear in mind that some of these patients who present with severe bradycardia may also be at risk of polymorphic VT or TdP.
The relevance and interest of the present study notwithstanding, some final points should be noted. Firstly, these data cannot be extrapolated to young or middle-aged adults admitted due to iatrogenic bradycardia, as the underlying substrate and etiology may be different in this setting. While a degenerative etiology is by far the most common in older patients, advanced AV conduction abnormalities in younger patients are often congenital or associated with autoimmune or infiltrative disorders, including cardiac sarcoidosis, or with pathological hypervagotonia, in which case the investigation is likely to proceed differently.14 Secondly, as mentioned by the authors, the reader should be aware that more prolonged electrocardiographic monitoring, either in-hospital or ambulatory, could detect asymptomatic episodes of advanced AV block warranting pacemaker implantation. This would in fact strengthen the authors’ conclusions by increasing the number of patients requiring a permanent pacemaker. Thirdly, given the retrospective and single-center nature of this study, the possibility of selection bias should not be underestimated. Finally, their assessment of predictors of the need for pacemaker implantation is limited by the small size of the study sample and low number of available variables, and therefore these specific findings should be interpreted with caution.
In summary, elderly patients admitted to hospital due to presumably reversible bradycardia, in particular those with AV block, are at high risk of requiring a permanent pacemaker even after discontinuation of the culprit medication. Consideration should be given to prophylactic pacemaker implantation in patients deemed to be at higher risk of recurrence or physical injury, and others should be monitored in an observational unit and, if discharged, kept under close surveillance with periodic or continuous ambulatory monitoring.
1Conflicts of interestThe author has no conflicts of interest to declare.