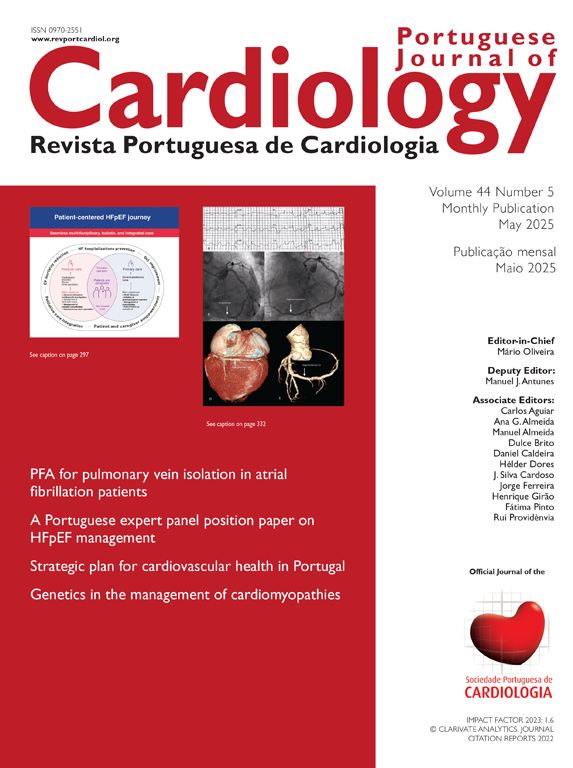
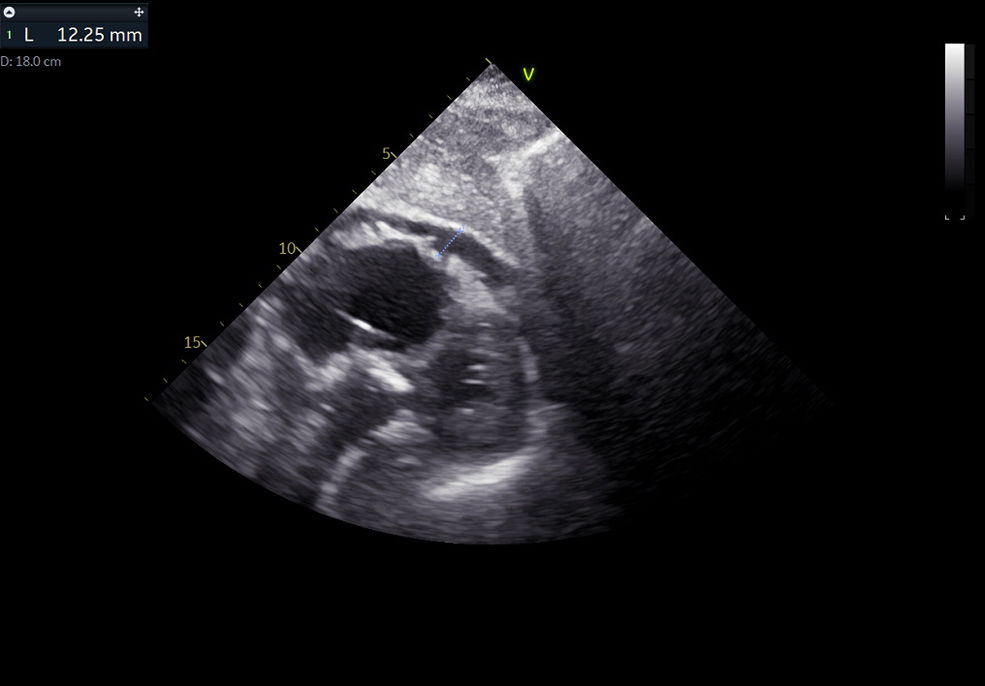
An 89-year-old man presented to the emergency department after recurrent episodes of syncope. Electrocardiographic monitoring yielded complete heart block with periods of ventricular asystole. A temporary transvenous pacemaker was inserted through the right femoral vein under fluoroscopic guidance. Following insertion, the patient reported severe chest pain, and undersensing with electrical capture failure was noted. Transthoracic echocardiography (TTE) revealed a de novo 12 mm circumferential pericardial effusion without tamponade (Figure 1). Cardiac computed tomography subsequently identified a sequential cardiac perforation: the pacemaker lead had penetrated the mid interventricular septum, then perforated the lateral left ventricular wall into the pericardial space (Figure 2). Due to the urgent need for device removal, anticoagulation was withheld. In the operating room, the electrode was successfully extracted by traction under TTE guidance. Although no additional pericardial effusion was seen post-removal, prophylactic pericardiocentesis was performed. The procedure was immediately complicated by an embolic ischemic stroke of the left anterior cerebral artery. Criteria for endovascular intervention were not met. He remained two weeks in the intensive care unit and was discharged one month after initial admission with left hemiparesis. This case highlights the potential for severe complications with temporary pacemaker insertion and underscores the need for vigilant monitoring post-implantation.
The authors have no conflicts of interest to declare.