Inappropriate implantable cardioverter-defibrillator (ICD) therapies due to supraventricular tachyarrhythmia (SVT) are a common problem.
The authors report this case to warn of a possible detection problem and subsequent failure of deliver appropriate therapy in patients with atrial fibrillation (AF) and a dual-chamber ICD using the PARAD+ algorithm. To our knowledge this is the first reported case of failure to deliver a shock in a dual-chamber ICD due to the PARAD+ algorithm.
Case reportThe authors present a case of a 68-year-old Caucasian man with permanent AF and a dual-chamber Sorin Paradym ICD with the PARAD+ algorithm, who presented an episode of sustained ventricular tachycardia (VT). The ICD did not store the event and did not delivery a therapy, although the heart rate curve was consistent with an episode of VT. No evidence of system dysfunction was found.
ConclusionDue to simultaneous occurrence of VT and AF rhythms and alternation in rhythm classification by the PARAD+ algorithm the number of cycles needed to diagnose VT was not achieved and no therapy was delivered.
In patients with permanent or long-term persistent AF with a dual-chamber ICD using the PARAD+ algorithm, discrimination should be based only on the ventricular channel. In patients with paroxysmal or persistent recurrent AF the risk of not delivering VT therapy must be weighed against the risk of inappropriate therapy.
as terapias inapropriadas de um cardioversor-desfibrilhador implantável (CDI) devido a taquiarritmias supraventriculares (TSV) são ainda um problema comum.
Os autores relatam este caso de modo a alertar um possível problema de deteção e subsequente falha na entrega de terapia apropriada em pacientes com CDI de dupla-câmara e fibrilhação auricular (FA) com o algoritmo PARAD+. Ao nosso conhecimento, trata-se do primeiro caso reportado de falha na entrega de choque num CDI de dupla-câmara, devido ao algoritmo PARAD+.
Caso clínicoos autores relatam um caso de um homem de 68 anos de idade, caucasiano, com FA permanente, portador de um CDI de dupla-câmara Paradym Sorin com o algoritmo PARAD+, que apresentou um episódio de taquicardia ventricular (TV) mantida. O CDI não armazenou o episódio e não administrou qualquer terapia, apesar de a curva da frequência cardíaca ser consistente com um episódio de TV. Não foi encontrada nenhuma evidência de disfunção do sistema.
ConclusãoDevido à ocorrência simultânea de ritmos de TV e FA e à alternância na classificação de ritmo pelo algoritmo PARAD+, não foi alcançada a persistência programada para a deteção de TV e a terapia não foi administrada.
Em pacientes com FA persistente de longa duração/permanente com CDI de dupla câmara com algoritmo PARAD+, a discriminação deve ser baseada apenas no canal ventricular. Em pacientes com FA paroxística/persistente recorrente o risco de não entrega de terapia para a TV deve ser balançado com o risco de terapia inapropriada.
The broadening of indications for treatment with an implantable cardioverter-defibrillator (ICD) to include patients at risk (primary prevention) has further increased the importance of limiting the incidence of device-related adverse events in order to preserve patients’ quality of life.
Inappropriate delivery of ICD therapies triggered by supraventricular tachyarrhythmias (SVT) is a common problem, occurring in 16–22% of patients.1
Studies have shown that detection enhancements in dual-chamber ICDs are able to reduce inappropriate therapies due to SVT and associated adverse clinical outcomes. However, other studies have failed to find an improvement in rhythm classification or a reduction of shocks with the use of dual-chamber algorithms.2
Recently, more advanced detection algorithms have been proposed in order to reduce the number of inappropriate ICD therapies. The PARAD and PARAD+ algorithms correctly identify ventricular tachycardia (VT) in more than 99% of cases, and slow VT (150 bpm) in 94%. Their specificity for SVT detection is particularly high (92%), with 86% of episodes of atrial fibrillation (AF) or atrial flutter being correctly classified.3 The PARAD+ algorithm, which inhibits VT therapy when a long ventricular cycle is detected, improves the performance of the PARAD algorithm in AF, by increasing specificity for AF in the slow zone, without decreasing sensitivity for VT.4
The authors report the case of a patient with a dual-chamber ICD with the PARAD+ algorithm who presented sustained VT but no therapy was delivered.
Case reportThe authors report a case of a 68-year-old Caucasian male with a history of paroxysmal AF, stroke and ischemic cardiomyopathy with severe left ventricular systolic dysfunction, who had a dual-chamber ICD (Paradym DR, Sorin) implanted after an episode of monomorphic VT in 2010. In 2011 AF became permanent. No therapies were delivered by the ICD.
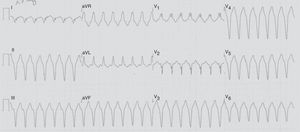
On December 31, 2012 the patient suddenly complained of rapid and persistent palpitations, dyspnea and dizziness. The ECG revealed VT with a rate of 170 bpm (Figure 1). His blood pressure was 70/45 mmHg. An external shock was immediately delivered, which successfully terminated the VT approximately two hours after the onset of palpitations.
Interrogation of the ICD revealed no abnormal sensing or pacing parameters. Ventricular autosensing histograms revealed that all detected ventricular waves were well above the sensitivity threshold. The ICD was programmed with four detection zones and corresponding therapies: slow VT zone, programmed at 462 ms for 100 consecutive cycles, with no therapy (monitoring zone); VT zone, programmed at 400 ms for 50 consecutive cycles, with anti-tachycardia pacing (ATP) and shock; a fast VT zone at 300 ms for 14 consecutive cycles, with ATP and shock; and finally a ventricular fibrillation (VF) zone at 250 ms. The PARAD+ detection algorithm was activated.
In the arrhythmia history stored in the device, after the last follow-up on September 14, 2012 there were 15 episodes, but none was dated December 31, 2012, and none was labeled as VT. The most recent episode was dated December 11, 2012 and was labeled as SVT/ST. However, the last 24-hour heart rate curve was consistent with the reported VT (Figure 2).
On January 2nd 2013 VF was induced and correctly detected and terminated with a 20-J shock.
The patient was discharged after a change to the Stability+/Acceleration algorithm and a reduction in the VT zone to 30 cycles. At three-month follow-up, the patient remained asymptomatic and no events were recorded.
DiscussionWhy did the ICD not record an event or deliver a therapy? Was the device functioning correctly?
In order to answer these questions, it is essential to understand the PARAD+ algorithm and how it determines the functioning of the ICD. When a majority of RR intervals are detected within the VT zone, both the PARAD and PARAD+ algorithms first examine ventricular stability. If the rhythm is unstable, AF is diagnosed and therapy is withheld. If the rhythm is stable, atrioventricular (AV) conduction is then analyzed. If the rhythm is stable and A and V are dissociated, VT is diagnosed by PARAD and therapy is delivered. However, if PARAD+ is activated, the occurrence of long ventricular cycles is examined. Each ventricular cycle is compared beat-to-beat to the mean tachycardia cycle length, the average of the last four intervals shorter than or equal to the programmed tachycardia detection interval. VT therapy is inhibited for 24 consecutive cycles after each ventricular interval longer than this average plus a programmable increment, set at a nominal value of 172 ms.4
The maximum storage of the Sorin Paradym DR ICD is 15 episodes. At the time the ICD was interrogated on January 1, 2013, the device memory was full. In such circumstances, according to priorities for storage of episodes, the device continues to record sustained episodes only. So, from the device's point of view (according to the discrimination algorithms and the programmed settings) no sustained ventricular arrhythmia occurred after December 11, 2012. This means that during the episode none of the programmed numbers of consecutive cycles was reached, either for the slow VT zone (100 consecutive cycles), or for the VT zone (50 consecutive cycles), or for the fast VT/VF zone (14 consecutive cycles), probably due to changes in the rhythm majorities.
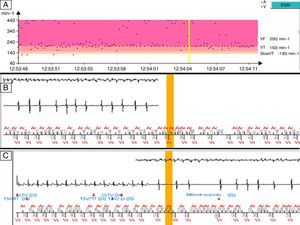
When the last stored episodes were analyzed, episodes correctly classified as SVT were noted, corresponding to AF episodes with rapid ventricular rate. However, in the last episode stored the intracardiac electrograms (IEGMs) and the tachograph (Figure 3) revealed a period suggestive of VT (based on rhythm stability and on the ventricular IEGM). During this period, the device successively alternated the rhythm classification between SVT/ST and ventricular tachycardia with long cycle length (VTLC), based on AV association. As seen above, once the rhythm is classified as stable (meaning that in nominal settings at least 75% of the last eight RR intervals are within a 65-ms stability window), AV conduction is analyzed. The rhythm is considered associated when at least 75% of the total PR intervals from the eight last RR intervals fall in the 65-ms stability window. In the episode described, the device successively alternated the AV association from stable and not associated (VTLC diagnosis) to N:1 association (SVT diagnosis) and 1:1 association (classified as SVT or VT by PARAD+, depending on additional acceleration criteria).
Intracardiac electrograms and tachograph of the last stored episode, dated 11 December, 2012. (A) Tachogram showing some irregularity in atrial waves but regularity of ventricular activity; (B and C) electrograms revealing changes in morphology and regularity of the RR interval and successive alternation of rhythm classification between supraventricular tachyarrhythmia/ventricular tachycardia and ventricular tachycardia with long cycle length.
Thus, in the case reported, the most probable hypothesis is that due to simultaneous occurrence of VT and AF rhythms, the ongoing rhythm classification (based on AV association) alternated between SVT/ST majority and VT/VTLC majority, and so the programmed VT cycle number was never reached and therapy was consecutively delayed. Also, since there were already 15 episodes stored in the device's arrhythmia history, no event was recorded.
Since the patient had permanent AF it was decided to change the algorithm criterion to “Stability+/Acceleration”. This criterion is based on ventricular intervals only; the algorithm does not take PR association into account, and therefore there is no risk of not treating a VT due to changing PR association. However, it does not take into account the origin of the acceleration, so there is a risk of misclassifying an SVT with 1:1 conduction in the ventricle as VT, which could lead to the delivery of inappropriate therapies.
We cannot say with certainty what would happen if the VT zone were programmed for less than 50 consecutive cycles, but the risk of not delivering appropriate therapy would certainly be lower. However, recent studies have reported fewer inappropriate shocks using a duration of 30 cycles for VT, with no increase in the incidence of syncope or death,5 and in the MADIT-RIT trial (in which AF patients were excluded), a 60-second delay (VT zone 170–199 bpm) before initiation of therapy had a overall result superior to conventional programming.6 Due to the reported event we decreased the number of consecutive cycles to 30.
To our knowledge this is the first case report worldwide of failure to deliver a shock in a dual-chamber ICD due to the PARAD+ algorithm.
ConclusionPhysicians’ knowledge of the algorithms of the different models and manufacturers is necessarily imperfect.
In patients with permanent or long-term persistent AF with a dual-chamber ICD using the PARAD+ algorithm, discrimination should be based only on the ventricular channel, in order to avoid problems with detection and subsequent failure to deliver therapy. In patients with paroxysmal or persistent recurrent AF the risk of not delivering VT therapy must be weighed against the risk of delivering inappropriate therapy.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
AuthorshipRC and IJ were major contributors in writing the manuscript. All authors read and approved the final manuscript.
Conflicts of interestThe authors have no conflicts of interests to declare.