A 64-year-old male, with cardiovascular risk factors and previous history of bilateral carpal tunnel syndrome, presented with exertional retrosternal pain. The resting echocardiogram was unremarkable. A stress echocardiogram with dobutamine revealed hypokinesis of the inferior wall, associated with angina, followed by ventricular tachycardia. The coronary angiography revealed slow flow, a dominant right coronary artery with non-obstructive atherosclerosis and a left anterior descending artery with intermediate lesions in mid and distal segments. The invasive functional evaluation, including fractional flow reserve, thermodilution coronary flow reserve and index of microvascular resistance, led to the diagnosis of microvascular angina, treated with calcium channel blockers and transdermal nitrate, giving symptom relief.
EvolutionThree years later he developed complete atrioventricular block and a dual chamber pacemaker was implanted. Shortly after, the patient developed progressive symmetrical tetraparesis, associated with marked muscle atrophy, hand numbness, orthostatic hypotension and dysphagia. The neurology workup led to the diagnosis of familial amyloidotic polyneuropathy, with the Val30Met mutation in the transthyretin gene. The following year he developed congestive heart failure. The echocardiogram showed moderate concentric left ventricular hypertrophy with preserved ejection fraction. A 99mTc-DPD Scintigraphy showed significant myocardial tracer uptake, leading to a diagnosis of TTR amyloid infiltration.
DiscussionPatients with exertional angina and microvascular disease should be kept under close surveillance, as they may have systemic disease with cardiac involvement. Carpal tunnel syndrome, in the context of undiagnosed cardiac disease, should trigger suspicion of cardiac amyloidosis.
Um homem de 64 anos, com fatores de risco cardiovascular e antecedentes de síndrome do canal cárpico bilateral, apresentou-se com queixas de angina de esforço. O ecocardiograma em repouso era normal. O ecocardiograma de sobrecarga com dobutamina revelou hipocinésia da parede inferior, acompanhada de angina e taquicardia ventricular autolimitada. A coronariografia revelou artérias com fluxo lento, coronária direita dominante com aterosclerose não obstrutiva e descendente anterior com lesões intermédias nos segmentos médio e distal. A avaliação invasiva do significado funcional das lesões incluiu fractional flow reserve, coronary flow reserve e index of microvascular resistance e resultou no diagnóstico de angina microvascular, tratada com bloqueador dos canais de cálcio e nitratos, com alívio sintomático.
EvoluçãoTrês anos depois, o doente desenvolveu bloqueio auriculoventricular completo, tendo sido implantado um pacemaker de dupla câmara. Concomitantemente, evoluiu com tetraparésia simétrica, atrofia muscular marcada, dormência das mãos, hipotensão ortostática e disfagia. A investigação do quadro neurológico resultou no diagnóstico de Polineuropatia Amiloidótica Familiar, com mutação Val30Met no gene da transtirretina. No ano seguinte, desenvolveu insuficiência cardíaca congestiva. O ecocardiograma apresentava agora hipertrofia ventricular esquerda concêntrica, com função sistólica preservada. Realizou uma cintigrafia com 99mTc-DPD que mostrou intensidade de sinal compatível com depósito intramiocárdico de substância amiloide.
DiscussãoOs doentes com angina de esforço e doença microvascular devem manter seguimento clínico regular, uma vez que poderão ter uma doença sistémica com envolvimento cardíaco. A síndrome do canal cárpico, no contexto de doença cardíaca não esclarecida, deve levantar a suspeita de amiloidose cardíaca.
Coronary artery disease (CAD) is a common cause of exertional retrosternal pain in middle aged men. In patients with non-obstructive CAD, other diagnoses, including microvascular angina (and microvascular disease in the setting of other specific cardiac diseases), should be considered.1 Microcirculatory dysfunction can be diagnosed invasively with thermodilution coronary flow reserve (CFR) and the index of microvascular resistance (IMR).2 CFR interrogates coronary circulation as a whole, identifying whether global flow supply is normal.3 IMR is considered a surrogate for microvascular damage and has been shown to have predictive value for myocardial recovery in patients with acute myocardial infarction.4 When IMR and CFR evaluations are combined in patients with intermediate coronary stenosis, high IMR and low CFR are associated with the worst prognosis.5 Our case will present the long-term prognosis of a patient with such characteristics, with the additional finding of a systemic disease with cardiac involvement.
Case descriptionA 64-year-old male presented with exertional retrosternal pain. He had a past medical history of hypertension, dyslipidemia, obesity, bilateral carpal tunnel syndrome and underwent bilateral surgical release and cervical laminectomy. The resting electrocardiogram revealed an incomplete left bundle branch block, while the resting echocardiogram was completely unremarkable. He underwent a stress echocardiogram with dobutamine; at peak stress, the left ventricle developed regional wall motion abnormalities including hypokinesis of the inferior wall, associated with angina and soon followed by ventricular tachycardia, reversed with propranolol. The patient was hospitalized and underwent a coronary angiography which revealed slow flow, dominant right coronary artery with non-obstructive atherosclerosis and a left anterior descending artery (LAD) with intermediate lesions in mid and distal segments (Figures 1 and 2). A functional evaluation revealed a non-significant fractional flow reserve of 0.86 in the LAD, but a pathological CFR of 1.8 and an IMR of 61. Given the patient's symptoms, risk factors and diagnostic tests, he was considered to have microvascular angina and was treated with antiplatelet therapy, a statin, a calcium channel blocker and a transdermal nitrate, with symptomatic relief.
Three years later he developed complete atrioventricular block and presented in the emergency department with sudden hemodynamic collapse. A dual chamber pacemaker was implanted, and he was discharged asymptomatic.
Shortly after, the patient developed progressive symmetrical tetraparesis, associated with marked muscle atrophy, hand numbness, orthostatic hypotension and dysphagia. The neurology workup led to the diagnosis of familial amyloidotic polyneuropathy (FAP), and the Val30Met mutation in the transthyretin (TTR) gene was detected.
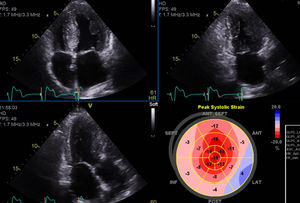
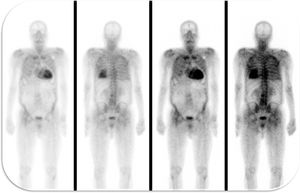
The following year, he developed NYHA class II to III congestive heart failure (HF), requiring uptitration of diuretics. The repeat echocardiogram showed moderate concentric left ventricular hypertrophy, with preserved ejection fraction but an abnormal global longitudinal strain and elevated filling pressures (Figure 3). He repeated the coronary angiography which excluded CAD progression. He underwent a 99mTc-DPD scintigraphy that revealed significant myocardial tracer uptake, diagnosing TTR amyloid infiltration (Figure 4). He was stabilized with medical therapy and kept under close follow-up, requiring antianginal therapy uptitration for exertional microvascular angina.
Transthyretin FAP with the Val30Met mutation in the transthyretin gene affects primarily the peripheral nervous system. Still, it can be associated with clinically significant myocardial infiltration6 in up to 15% of the patients with late onset disease.7 Cardiac presentation includes conduction block, arrhythmia and cardiac hypertrophy.
In our clinical case, the patient presented with microvascular angina, a rare symptom of cardiac infiltration. The only findings from his medical history that were in keeping with the suspicion of an infiltrative disease were the bilateral carpal tunnel syndrome and the atrioventricular block.8 The echocardiographic findings suggestive of myocardial infiltration were present only when the patient developed HF, after 4 years of medical follow-up. At that time, the 99mTc-DPD scintigraphy was consistent with TTR infiltration. This technique has been shown to be specific for cardiac involvement in TTR amyloidosis, with mild or no tracer uptake in patients without cardiac involvement9 or in patients with other types of systemic amyloidosis.10 As a consequence, 99mTc-DPD scintigraphy is recommended as a diagnostic test for TTR cardiac amyloidosis in the European guidelines.11
An alternative, well validated imaging technique for the diagnosis of cardiac amyloidosis would be cardiovascular magnetic resonance, which often reveals a pattern of global, sub-endocardial or segmental late gadolinium enhancement.12 However, this exam was contraindicated in this case, as the patient had a conventional pacemaker implanted before developing HF.
Therapeutic options are limited for patients with FAP. Liver transplantation is a treatment option that prolongs life, particularly in patients with the Val30Met mutation.13 Tafamidis is a TTR protein stabilizer approved for the treatment of this condition. In a recently published trial, tafamidis reduced mortality and cardiovascular hospitalization when compared with placebo, in patients with wild type TTR amyloidosis and FAP.14
An important learning point of this case is that in patients with exertional angina and microvascular disease, a specific etiology should be sought, as this may occur in the context of myocardial disease, due to vascular infiltration or adverse remodeling.15
Conflicts of interestThe authors have no conflicts of interest to declare.