Diagnostic tests that use ionizing radiation play a central role in cardiology and their use has grown in recent years, leading to increasing concerns about their potential stochastic effects.
The aims of this study were to compare the radiation dose of three diagnostic tests: single photon emission computed tomography (SPECT), invasive coronary angiography (ICA) and cardiac computed tomography (cardiac CT) and their evolution over time, and to assess the influence of body mass index on radiation dose.
MethodsWe assessed consecutive patients included in three prospective registries (SPECT, ICA and cardiac CT) over a period of two years. Radiation dose was converted to mSv and compared between the three registries. Differences over time were evaluated by comparing the first with the fourth semester.
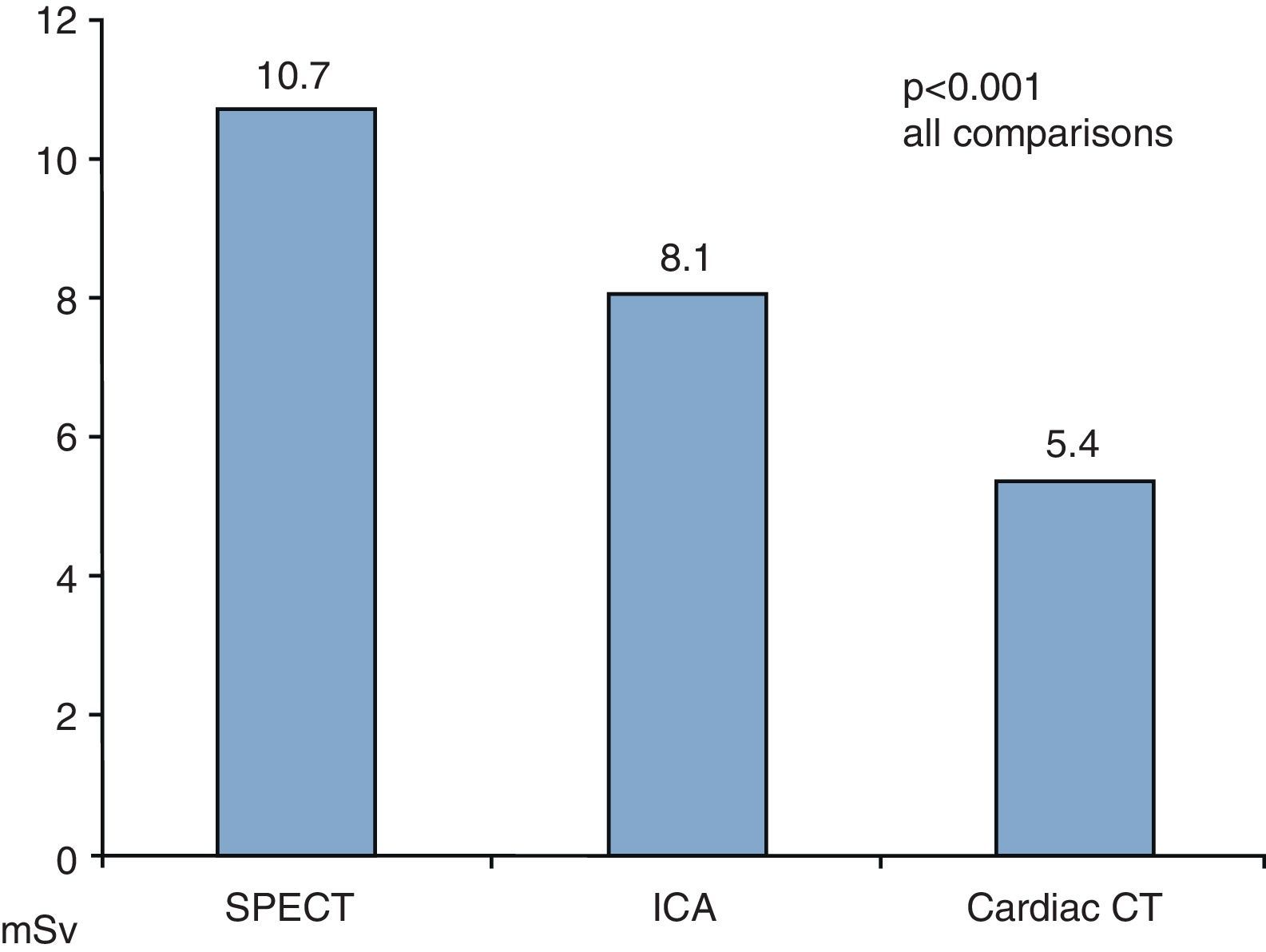
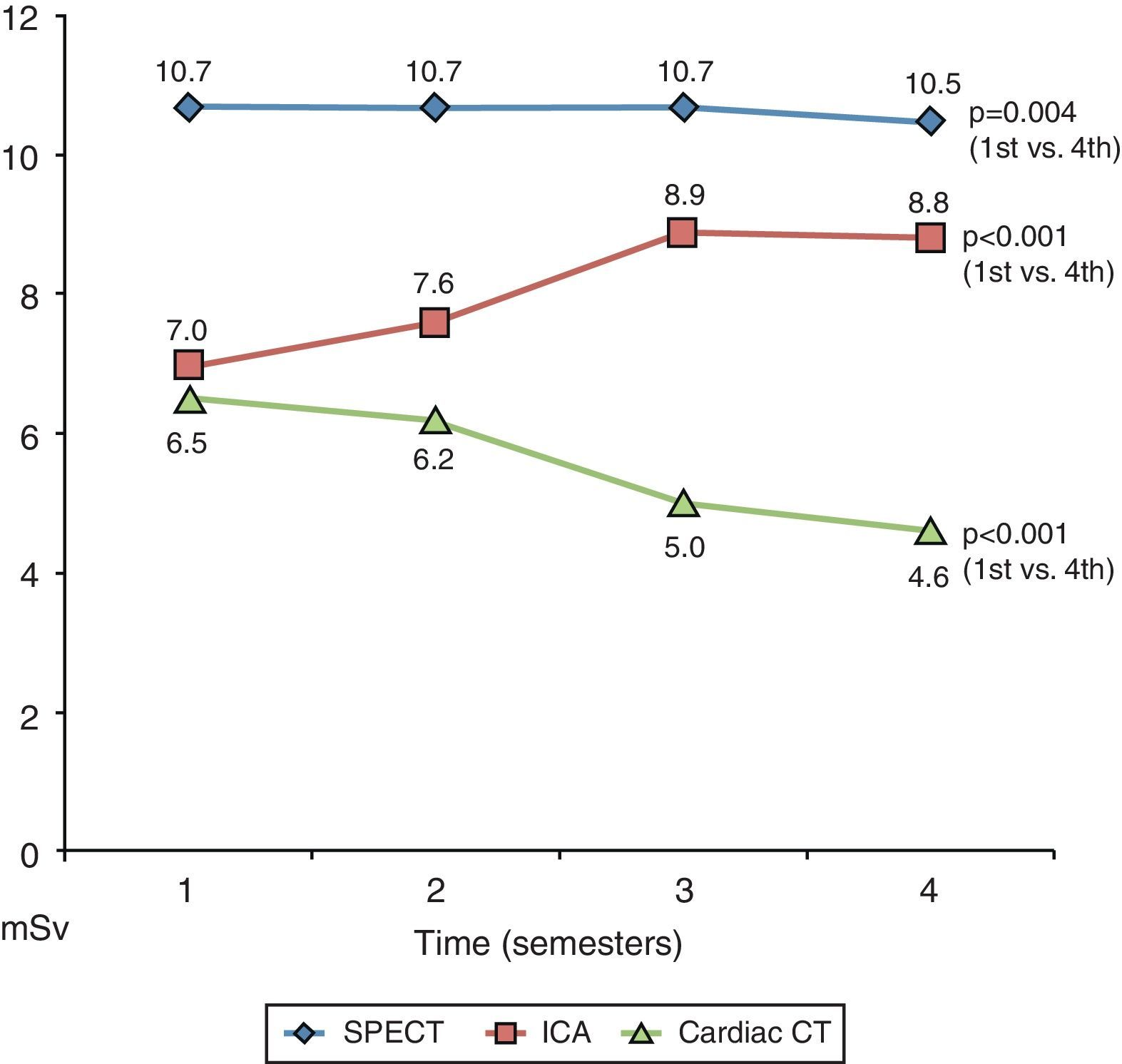
ResultsA total of 6196 exams were evaluated: 35% SPECT, 53% ICA and 22% cardiac CT. Mean radiation dose was 10.7±1.2 mSv for SPECT, 8.1±6.4 mSv for ICA, and 5.4±3.8 mSv for cardiac CT (p<0.001 for all). With regard to the radiation dose over time, there was a very small reduction in SPECT (10.7 to 10.5 mSv, p=0.004), a significant increase (25%) in ICA (7.0 to 8.8 mSv; p<0.001), and a significant reduction (29%) in cardiac CT (6.5 to 4.6 mSv, p<0.001). Obesity was associated with a significantly higher radiation dose in all three exams.
ConclusionsCardiac CT had a lower mean effective radiation dose than invasive coronary angiography, which in turn had a lower mean effective dose than SPECT.
There was a significant increase in radiation doses in the ICA registry and a significant decrease in the cardiac CT registry over time.
Os exames diagnósticos que usam radiação ionizante têm um papel central na cardiologia e a par do seu uso crescente, tem aumentado a preocupação pelos seus potenciais efeitos estocásticos.
Os objetivos deste estudo foram: 1) Comparar a dose de radiação de três exames: Cintigrafia de perfusão miocárdica (SPECT), coronariografia invasiva (CAT) e tomografia computorizada cardíaca (AngioTC) e a sua evolução temporal. 2) Avaliar o impacto do índice de massa corporal na dose de radiação.
MétodosDoentes consecutivos incluídos em três registos prospetivos (SPECT, CAT e AngioTC) durante dois anos. A dose de radiação foi convertida a mSv e comparada entre os três registos. A evolução temporal foi avaliada por comparação do 1.° e 4.° semestres.
ResultadosForam avaliados 6196 exames: 35% SPECT, 53% CAT e 22% AngioTC. A dose de radiação foi: 10,7 ± 1,2 mSv para o SPECT; 8,1 ± 6,4 mSv para o CAT; 5,4 ± 3,8 mSv para a AngioTC (p < 0,001 todas comparações).
Evolução temporal da dose de radiação: redução muito ligeira no SPECT (10,7 para 10,5 mSv; p = 0,004); aumento significativo (25%) no CAT (7,0 para 8,8 mSv; p < 0,001); redução significativa (29%) na AngioTC (6,5 para 4,6 mSv; p < 0,001). A obesidade associou-se a níveis de radiação significativamente mais elevados nos três exames.
ConclusãoO exame associado a uma menor dose de radiação foi a AngioTC, seguida do CAT que, por sua vez, foi menor que a do SPECT. Houve um aumento significativo da dose de radiação no registo CAT e uma redução significativa no registo da AngioTC ao longo do tempo.
Body mass index
coronary artery disease
computed tomography
invasive coronary angiography
single photon emission computed tomography
In recent years, the development of imaging techniques using ionizing radiation has resulted in considerable progress in the diagnosis and treatment of heart disease. Three commonly used diagnostic modalities that involve ionizing radiation are used for assessing patients with possible coronary artery disease (CAD): single photon emission computed tomography (SPECT), cardiac computed tomography (cardiac CT) and invasive coronary angiography (ICA), the latter being considered the gold standard for the diagnosis of CAD.1
Different radiation doses have been reported for each of these exams, ranging from 5 to 10 mSv for ICA, 6 to 15 mSv for SPECT, and 4 to 21 mSv for cardiac CT.2–5 With more frequent use of these exams, there have been growing concerns about the radiation's potential secondary effects, especially the stochastic effects of high cumulative doses over time.6,7
We have previously reported on the effective radiation dose associated with cardiac CT in a single-center registry, documenting a significant decrease in dose over time, and were able to identify the predictors of higher dose.8
New scanners and acquisition protocols have recently been developed which lead to significant reductions in radiation dose associated with cardiac CT.9,10
The aims of this study were to evaluate and compare the radiation dose used in three diagnostic tests – SPECT, ICA and cardiac CT – and their evolution over time, and to assess the influence of body mass index on radiation dose.
MethodsFrom three prospective registries of SPECT, ICA and cardiac CT, we selected for this analysis the exams performed during a two-year period (October 1, 2008 to September 30, 2010) in which the indication was assessment of possible CAD.
The exams were performed with an SMV DST-XL gamma camera using 99m Tc-tetrofosmin with stress/rest or rest/stress protocols (SPECT registry), a Siemens Coroskop TOP/ARTIS dFC system (ICA registry), and a Siemens Somatom Definition dual-source scanner (cardiac CT registry). The effective radiation dose was converted to mSv in accordance with current literature and the manufacturer's product information and compared between the registries. Briefly, a factor of 0.014 mSv/Gy cm was used for the conversion of cardiac CT dose-length product,9,11 a factor of 0.183 mSv/Gy cm2 was used for the conversion of ICA dose-area product,12,13 and factors of 0.0060 mSv/MBq−1 (after exercise) and 0.0071 mSv/MBq−1 (at rest) were used for the conversion of injected activity in SPECT.14–16 To evaluate the evolution of radiation doses over time, the study period was divided into four semesters according to the date of the exam and effective radiation dose was compared between the first and last semesters in each registry. All prospectively collected variables in the respective registries were analyzed, looking for predictors of dose change over time.
Statistical analysisContinuous variables are presented as mean ± standard deviation (unless otherwise specified), and categorical variables as number (n) or frequency (%).
Continuous variables were analyzed using the Mann–Whitney or Kruskal–Wallis nonparametric tests. The chi-square test was used to assess differences in frequencies.
Statistical significance was accepted for two-sided p values <0.05.
The statistical analysis was performed using SPSS Statistics 17.0 for Windows.
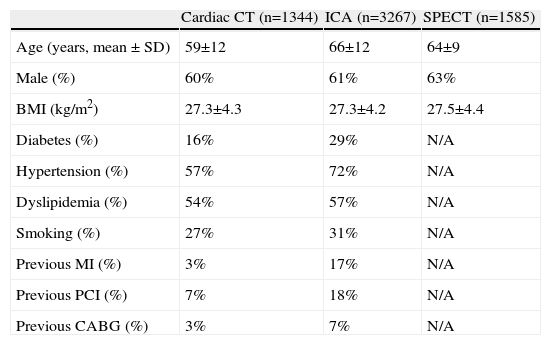
ResultsDuring the two-year period of this analysis, 6196 exams were performed: 3267 (52.7%) ICA, 1585 (25.6%) SPECT and 1344 (21.7%) cardiac CT. The demographic and clinical characteristics of the study population are presented in Table 1.
Demographic and clinical characteristics of the study population.
| Cardiac CT (n=1344) | ICA (n=3267) | SPECT (n=1585) | |
| Age (years, mean ± SD) | 59±12 | 66±12 | 64±9 |
| Male (%) | 60% | 61% | 63% |
| BMI (kg/m2) | 27.3±4.3 | 27.3±4.2 | 27.5±4.4 |
| Diabetes (%) | 16% | 29% | N/A |
| Hypertension (%) | 57% | 72% | N/A |
| Dyslipidemia (%) | 54% | 57% | N/A |
| Smoking (%) | 27% | 31% | N/A |
| Previous MI (%) | 3% | 17% | N/A |
| Previous PCI (%) | 7% | 18% | N/A |
| Previous CABG (%) | 3% | 7% | N/A |
Values are means (SD) or percentages. BMI: body mass index; CABG: coronary artery bypass grafting; CT: computed tomography; ICA: invasive coronary angiography; MI: myocardial infarction; N/A: not available; PCI: percutaneous coronary intervention; SPECT: single photon emission computed tomography.
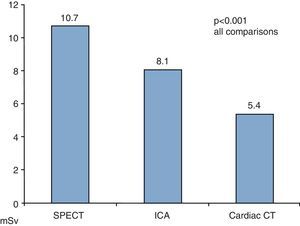
Mean effective radiation dose was 8.2±5.6 mSv for the whole population, 10.7±1.2 mSv for SPECT, 8.1±6.4 mSv for ICA and 5.4±3.8 mSv for cardiac CT (p<0.001 for all comparisons, Figure 1).
Division of the study period into semesters showed that there was a small but significant reduction in mean effective radiation dose over time for SPECT (10.7 to 10.5 mSv; p<0.01). In cardiac CT there was a significant 29% decrease in mean effective radiation dose (6.5 to 4.6 mSv, p<0.001) and in ICA a significant 25% increase (7.0 to 8.8 mSv; p<0.001) (Table 2 and Figure 2).
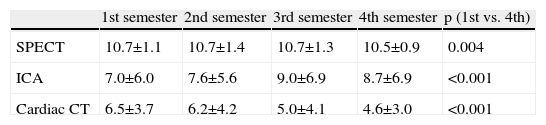
Mean effective radiation dose for each exam over the four semesters.
| 1st semester | 2nd semester | 3rd semester | 4th semester | p (1st vs. 4th) | |
| SPECT | 10.7±1.1 | 10.7±1.4 | 10.7±1.3 | 10.5±0.9 | 0.004 |
| ICA | 7.0±6.0 | 7.6±5.6 | 9.0±6.9 | 8.7±6.9 | <0.001 |
| Cardiac CT | 6.5±3.7 | 6.2±4.2 | 5.0±4.1 | 4.6±3.0 | <0.001 |
CT: computed tomography; ICA: invasive coronary angiography; SPECT: single photon emission computed tomography.
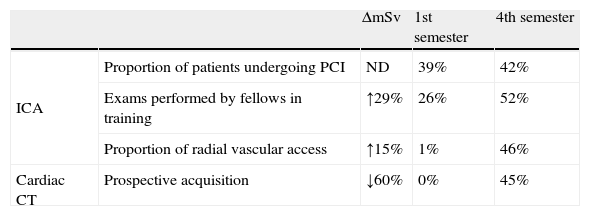
The factors associated with the 25% increase in mean effective radiation dose with ICA from the first to the fourth semester were the higher proportions of positive exams, radial vascular access and exams performed by fellows in training (Table 3). In the first semester 39% of ICA progressed to percutaneous coronary intervention, while in the fourth semester this proportion increased to 42% (p<0.001). Regarding vascular access, in the first semester only 1% of ICA were performed by radial access, which increased to 46% in the fourth semester. In our population, the use of radial vascular access was associated with a mean increase of 15% in effective radiation dose (from 7.8 mSv with femoral access to 9.0 with radial access, p<0.001). Finally, the proportion of exams performed by trainee operators increased from 26% in the first semester to 52% in the fourth. In this registry, when the exam was performed by a trainee operator there was a mean increase of 29% in effective radiation dose (from 7.3 mSv with a senior operator to 9.4 mSv with a trainee operator, p<0.001).
Variables associated with increase in ICA radiation dose and decrease in cardiac CT radiation dose.
| ΔmSv | 1st semester | 4th semester | ||
| ICA | Proportion of patients undergoing PCI | ND | 39% | 42% |
| Exams performed by fellows in training | ↑29% | 26% | 52% | |
| Proportion of radial vascular access | ↑15% | 1% | 46% | |
| Cardiac CT | Prospective acquisition | ↓60% | 0% | 45% |
CT: computed tomography; ICA: invasive coronary angiography.
The only variable associated with the decrease in effective radiation dose for cardiac CT was the use of prospective (step-and-shoot) acquisition: the use of a prospective acquisition protocol was associated with a decrease of 60% in effective radiation dose. In the first semester no exams were performed with this protocol, while in the fourth semester 45% were acquired prospectively (Table 3).
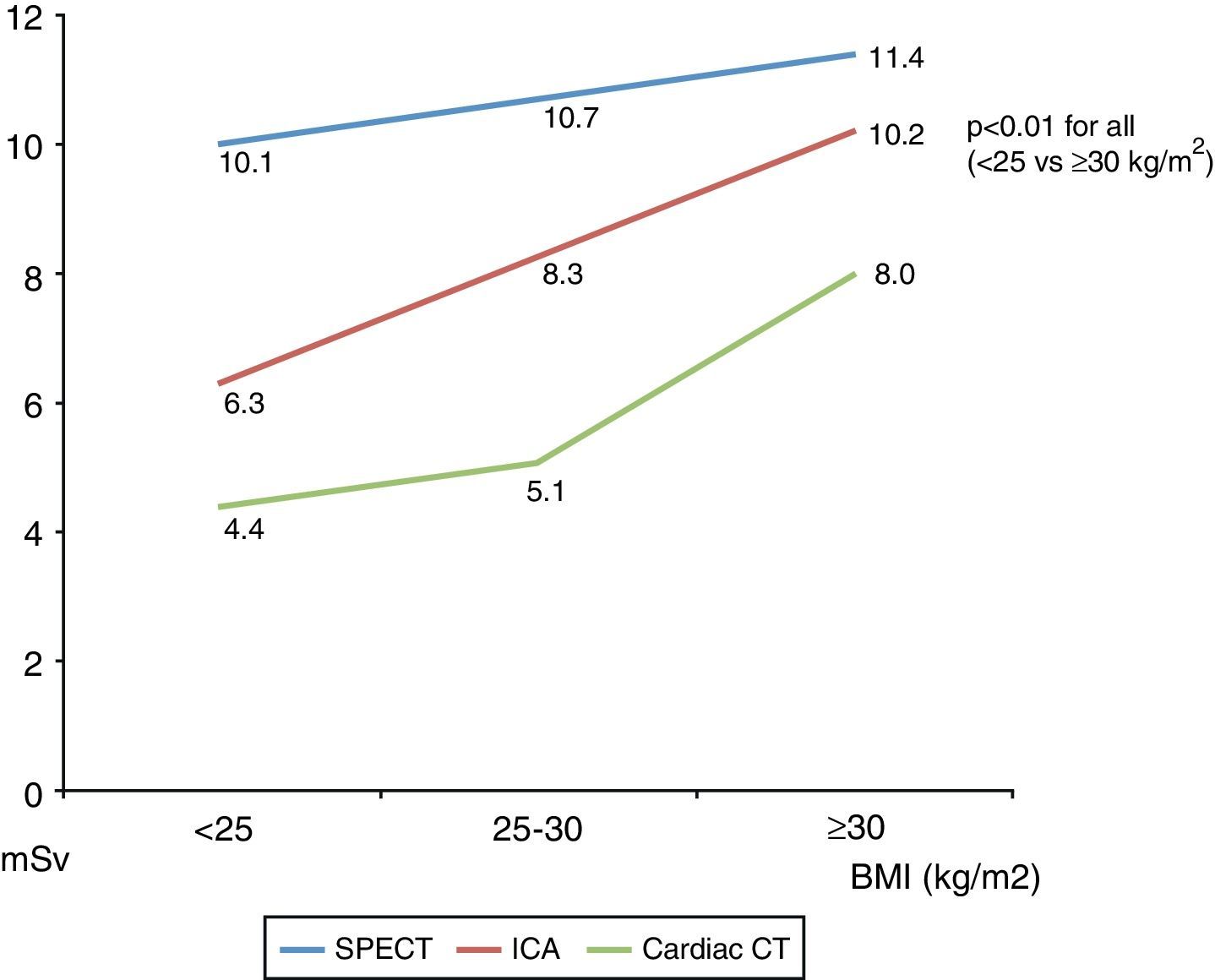
The influence of body mass index on mean effective radiation dose was also evaluated. There was a significantly higher dose in obese patients (BMI ≥30 kg/m2) compared to overweight patients, which in turn was higher that in patients with normal weight (BMI <25 kg/m2) (Figure 3).
DiscussionIn this analysis, we found significantly different effective radiation doses associated with common diagnostic tests used in cardiology. The dose was highest for SPECT, followed by ICA and lowest for cardiac CT. Furthermore, we found some time trends in the mean effective radiation dose associated with ICA and cardiac CT related to particular clinical and procedural methodologies.
The biological effects of ionizing radiation are related to the cumulative effective dose, and doses above 100 mSv have been linked to stochastic effects including the development of cancer, while the effects of lower radiation levels, common in diagnostic X-ray imaging, are much less clear.4,17 Although other theoretical models based on dose-threshold and hormetic effects have been proposed, the more conservative linear no-threshold model, which assumes that no level of radiation is without risk, is widely accepted.4,17
On this basis, procedures that use ionizing radiation should be performed in accordance with the “as low as reasonably achievable” philosophy, and physicians ordering and performing cardiac imaging diagnostic tests should be familiar with the associated radiation doses and with ways in which they can be minimized.
The mean effective radiation dose we found for each exam is in agreement with previous studies.3,4,6,18 Furthermore, we confirmed that certain variables influence the effective radiation dose delivered by these exams. For ICA, the effective radiation dose increased with the use of radial access and with less experienced operators, which is in line with published data.13,19 The higher radiation dose in the ICA registry over time was also associated with a higher proportion of positive exams; although we did not quantify the difference between positive and negative ICA, we can assume that positive tests needed more cine angiograms of the coronary arteries, with a consequent increase in the radiation dose used.
For cardiac CT, the introduction and increasingly frequent use of a prospective protocol during the study period was associated in our experience with a significant decrease in the effective radiation dose for this exam, as has been demonstrated by other authors.20–22 Finally, for SPECT, the dose change over time was very small, which is to be expected since there were no changes in protocol during the study period.
It is worth noting that during the same period, doses associated with stress-only and rest-only SPECT studies were significantly lower (with mean effective doses of 2.3±0.9 mSv and 5.8±1.0 mSv, respectively) but they were not considered for the purpose of this study, and the small number of patients involved (n=49 and n=63, respectively) would not have had a significant impact on the overall SPECT radiation dose.
Mean effective radiation doses were significantly higher for obese patients in all the exams analyzed. This was especially true for cardiac CT and ICA, with an almost two-fold increase in radiation dose compared to their normal-weight counterparts. In the SPECT registry, the effect of BMI was less pronounced. This should be taken in consideration when selecting the appropriate diagnostic exam, especially for those at higher risk from radiation exposure, like women and younger patients.23 In line with this, particular attention should be paid to cardiac CT dose, since patients in our registry undergoing cardiac CT were significantly younger than those in the ICA and SPECT registries.
Although the present study focuses on comparison of the radiation dose between three different diagnostic exams, other features should be taken into account when comparing different imaging modalities. As cardiac CT and ICA require the administration of iodinated contrast, care should be taken in the presence of impaired renal function or history of allergies; likewise, the probability of CAD is also an important factor, as SPECT and ICA are more appropriate for patients with higher probability of CAD.24,25 Thus, all these features (radiation dose, need for iodinated contrast and CAD probability) should be taken into consideration when selecting the most appropriate exam for each patient.
ConclusionsIn these registries of diagnostic tests commonly used in cardiology, the mean effective radiation dose used in cardiac CT was lower than that used in ICA, which in turn was lower than the doses used in SPECT. There was a significant increase over time in the mean effective radiation dose associated with ICA, mainly related to the increased use of radial access, and a decrease in cardiac CT doses as a consequence of the implementation of a prospective protocol. Obesity was associated with a significantly higher radiation dose in all three exams.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.


 ICA: invasive coronary angiography;
ICA: invasive coronary angiography; 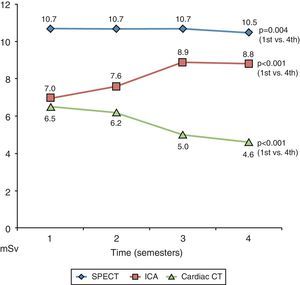 ICA: invasive coronary angiography;
ICA: invasive coronary angiography; 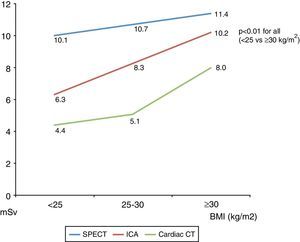 BMI: body mass index; CT: computed tomography;
BMI: body mass index; CT: computed tomography; 

