Right ventricular function is a major determinant of prognosis in pulmonary hypertension. The aim of this study was to assess and compare right ventricular contractile reserve in healthy subjects (controls) and in subjects with pulmonary hypertension (cases).
MethodsIn this prospective study of seven cases and seven controls undergoing treadmill stress echocardiography, right ventricular S-wave velocity, tricuspid annular plane systolic excursion (TAPSE), right ventricular fractional area change (RVFAC) and stroke volume index were assessed at rest and with exercise. The increase in each parameter between rest and exercise for cases and controls was analyzed and the magnitude of change in each parameter with exercise between cases and controls was compared.
ResultsA significant increase in S-wave velocity was observed in cases (rest: 9.4±3.1; exercise: 13.7±4.8 cm/s [p<0.05]). In controls there was a statistically significant increase in S-wave velocity (12.9±2.3 to 23.0±7.2 cm/s [p<0.005]), TAPSE (25.7±2.4 to 31.0±3.5 mm [p<0.05]) and RVFAC (53.8±14.7% to 64.4±9.9% [p<0.005]). The magnitude of change in S-wave velocity (cases: 4.3±3.3; controls: 10.1±5.5 cm/s [p<0.05]), TAPSE (cases: 0.6±2.5; controls: 5.3±3.8 mm [p<0.05]) and RVFAC (cases: −0.4±11.8; controls: 10.6±5.9% [p<0.05]) was significantly different between cases and controls.
ConclusionsS-wave velocity, TAPSE and RVFAC increased significantly with exercise in controls. S-wave velocity was the only parameter that showed a significant increase in cases, although the magnitude of this increase was significantly less than in controls.
A função ventricular direita é um determinante major do prognóstico na hipertensão pulmonar. Caracterização e comparação da reserva contrátil do ventrículo direito em indivíduos saudáveis (controlos) e doentes com hipertensão pulmonar (casos).
MétodosEstudo prospetivo de sete casos e sete controlos submetidos a ecocardiograma de esforço. Avaliámos, em repouso e no esforço, a velocidade da onda S ventricular direita, a excursão sistólica do plano anular tricúspide, a área de encurtamento fracional do ventrículo direito e o volume sistólico indexado. Analisámos o aumento de cada parâmetro entre repouso e esforço para casos e controlos e comparámos a magnitude de variação com o exercício de cada parâmetro entre casos e controlos.
ResultadosNos casos observámos aumento significativo da onda S (repouso 9,4±3,1; esforço 13,7±4,8cm/seg [p<0,05]). Nos controlos ocorreu aumento significativo da onda S (repouso 12,9±2,3; esforço 23,0±7,2cm/seg [p<0,005]), da excursão sistólica do plano anular tricúspide (repouso 25,7±2,4; esforço 31,0±3,5mm [p<0,05]) e da área de encurtamento fracional (repouso 53,8±14,7%; esforço 64,4±9,9% [p<0,005]). A magnitude de variação da onda S (casos 4,3±3,3; controlos 10,1±5,5cm/seg [p<0,05]), da excursão sistólica do plano anular tricúspide (casos 0,6±2,5; controlos 5,3±3,8mm [p<0,05]) e da a área de encurtamento fraccional (casos 0,4±11,8; controlos 10,6±5,9% [p<0,05]) foi significativamente diferente entre casos e controlos.
ConclusõesA onda S, a excursão sistólica do plano anular tricúspide e a área de encurtamento fracional aumentaram significativamente com o esforço nos controlos. A onda S foi o único parâmetro que aumentou significativamente nos casos, embora a magnitude desse aumento seja significativamente menor do que nos controlos.
magnitude of change
blood pressure
body surface area
heart rate
left ventricular
left ventricular eccentricity index
left ventricular outflow tract
pulmonary artery pressure
pulmonary hypertension
right ventricular
right ventricular fractional area change
right ventricular/right atrial
systolic blood pressure
arterial oxygen saturation
stroke volume index
tricuspid annular plane systolic excursion
velocity-time integral
Pulmonary arterial hypertension and chronic thromboembolic pulmonary hypertension are relatively rare diseases, with estimated prevalences of 15 cases/million adults and 3.8 cases/100 survivors of acute pulmonary embolism, respectively.1 Pulmonary hypertension (PH) is characterized by a progressive increase in pulmonary vascular resistance leading to right ventricular (RV) failure and death.2
RV function is the main determinant of evolution and prognosis in PH patients.3 Various clinical, functional, echocardiographic and hemodynamic parameters are used to assess severity, prognosis and response to therapy in PH patients, most of which reflect RV function.
RV contractile (or inotropic) reserve is defined as the response of the right ventricle to stress and may be an important prognostic factor, but the best parameters for its assessment remain to be determined.4
Treadmill stress echocardiography enables physiological assessment of different echocardiographic parameters throughout exercise.
AimThe aim of this study was to characterize and compare the RV contractile reserve of PH patients (cases) and healthy individuals (controls) using echocardiographic parameters of RV contractile reserve4,5 assessed through treadmill stress echocardiography.
MethodsStudy design and populationThis was a prospective observational study of seven cases and seven age- and gender-matched controls.
The following inclusion criteria were used in the selection of cases: age 18–65 years; sinus rhythm; PH confirmed by right heart catheterization according to the criteria of the 2009 European Society of Cardiology guidelines on PH1 and classified as in clinical group 1 (excluding PH associated with congenital diseases or portal hypertension) or group 4 (excluding patients who had undergone thromboendarterectomy); patients under unmodified therapy in the month previous to stress echocardiography; patients in NYHA/WHO functional class I, II or III (if the latter, in stable and satisfactory clinical condition); patients with a 6-minute walk test of over 350 m without developing hypotension or arterial oxygen desaturation exceeding 15%. Exclusion criteria were left heart disease, known lung disease, resting tachycardia (heart rate over 100 bpm), uncontrolled blood pressure (pre-exercise values greater than 160/100 mmHg), decompensated PH requiring hospitalization in the last month, and hemoglobin less than 10.0 g/l.
Inclusion criteria for the control group were asymptomatic status, normal cardiovascular examination, and ECG and transthoracic echocardiogram at rest without significant changes. Those with a history of cardiovascular or lung disease were excluded.
The protocol was approved by the ethics committee of our hospital and the exams were performed after patients’ informed consent was obtained.
Echocardiographic assessmentCases and controls underwent symptom-limited treadmill stress echocardiography according to the standard methodology used in our laboratory, using the modified Bruce protocol.6 All examinations were performed by the same operator on a Philips iE33 ultrasound system and were partially recorded.
The following were assessed before, during and after exercise echocardiography: ECG, arterial oxygen saturation (SO2) (non-invasively by pulse oximetry), and hemodynamic parameters (heart rate [HR] and blood pressure [BP]). Test duration and weight and height for calculation of body surface area (BSA) were recorded.
The following echocardiographic parameters were assessed at rest (standing position) and at peak exercise:
- –
for assessment of RV contractile reserve: in apical 4-chamber view, RV area in diastole (Figure 1) and in systole (to calculate right ventricular fractional area change [RVFAC]), tricuspid annular plane systolic excursion (TAPSE) at the level of the RV free wall, S-wave velocity (with tissue Doppler of the basal segment of the RV free wall), and left ventricular outflow tract (LVOT) velocity-time integral (VTI) (Figure 2). In parasternal long-axis view, LVOT diameter (Figure 1) was assessed only at rest, considering that this dimension does not change with exercise. Stroke volume index (SVI) was calculated on the basis of LVOT diameter, LVOT VTI and BSA.
Figure 2.Echocardiographic parameters of right ventricular contractile reserve in a pulmonary hypertension patient at rest (left) and at peak exercise (right); top – S-wave velocity; middle – TAPSE; bottom – LVOT VTI (used to calculate stroke volume index). LVOT VTI: left ventricular outflow tract velocity-time integral; TAPSE: tricuspid annular plane systolic excursion.
- –
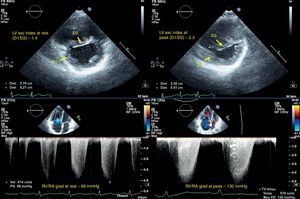
other parameters for characterization of RV morphology and function: in apical 4-chamber view, diastolic RV diameters (Figure 1) and the gradient between the right ventricle and right atrium in systole (RV/RA gradient). In parasternal short-axis (at the level of the papillary muscles): left ventricular diastolic diameters, to calculate the diastolic left ventricular eccentricity index (LVEI) (Figure 3).
Figure 3.Echocardiographic measurements in a pulmonary hypertension patient at rest (left) and at peak exercise (right); top – diastolic left ventricular eccentricity index; bottom – RV/RA gradient. D1 and D2: left ventricular diameters; LV exc index: diastolic left ventricular eccentricity index; RV/RA grad: right ventricular/right atrial gradient in systole.
Means and standard deviations were determined for each of the continuous variables studied. RV contractile reserve parameters (S-wave velocity, TAPSE, RVFAC and SVI) at rest and at peak exercise were compared between cases and controls, using the Student's t test for independent samples. The Student's t test for paired samples was used to compare values of RV contractile reserve parameters between rest and peak exercise within each group (cases and controls). The magnitude of change with exercise of RV contractile reserve parameters was also compared between cases and controls, using the Student's t test for independent samples. The statistical analysis was performed using IBM SPSS Statistics® version 20. A p value of <0.05 was considered statistically significant.
ResultsThe demographic characteristics of cases and controls are shown in Table 1.
The cases had mean pulmonary artery pressure (PAP) of 49.3±9.3 mmHg and mean pulmonary vascular resistance of 11.0±5.1 Wood units, by thermodilution. Three patients were in NYHA/WHO functional class I, three in class II and one in class III. Four patients were receiving triple therapy for PH, two dual therapy and one had not started treatment (Table 2). The cases had a mean hemoglobin level of 12.4±0.9 g/l (11.3–13.9 g/l).
Therapy regimen of cases at time of exercise echocardiography.
| Phosphodiesterase inhibitors | Endothelin receptor blockers | Prostaglandins | |
| Patient 1 | Sildenafil (50 mg 3 times daily) | Bosentan (125 mg 2 times daily) | Treprostinil (67 ng/kg/min SC) |
| Patient 2 | Bosentan (125 mg 2 times daily) | Iloprost (42 μg daily IN) | |
| Patient 3 | Sildenafil (50 mg 3 times daily) | Bosentan (125 mg 2 times daily) | Iloprost (250 μg daily IV) |
| Patient 4 | |||
| Patient 5 | Bosentan(125 mg 2 times daily) | Iloprost (54 μg daily IN) | |
| Patient 6 | Sildenafil (75 mg 3 times daily) | Bosentan (125 mg 2 times daily) | Treprostinil (68 ng/kg/min SC) |
| Patient 7 | Sildenafil (75 mg 3 times daily) | Bosentan (125 mg 2 times daily) | Treprostinil (47 ng/kg/min SC) |
IN: inhaled; IV: intravenous; SC: subcutaneous.
All exams took place without complications and were interrupted by symptoms (dyspnea or fatigue). All cases and controls maintained sinus rhythm during the stress echocardiograms.
Test duration, hemodynamic parameters and SO2 of cases and controls, at rest and at peak exercise, are shown in Table 3.
Test duration, hemodynamic parameters and arterial oxygen saturation of cases and controls.
| Duration (s) | Rest | Peak exercise | |||||
| HR | SBP | SO2 | HR | SBP | SO2 | ||
| Cases | 359.0±199.7 | 87.0±9.9 | 114.3±13.9 | 97.6±2.6 | 131.4±33.8 | 127.1±19.8 | 93.8±4.8 |
| Controls | 711.4±167.7 | 84.4±10.6 | 110.0±11.5 | 97.8±1.7 | 170.7±12.9 | 142.1±13.5 | 97.7±1.5 |
HR: heart rate; SO2: arterial oxygen saturation in %; SBP: systolic blood pressure in mmHg.
Echocardiographic parameters for RV characterization, at rest and at peak exercise, are shown in Table 4.
Echocardiographic characteristics of cases and controls at rest and at peak exercise.
| Cases | Controls | |||
| Rest | Peak exercise | Rest | Peak exercise | |
| Basal DD (mm) | 42.2±7.3 | 43.2±7.0 | 28.8±3.6 | 27.4±5.2 |
| Mid DD (mm) | 45.2±11.8 | 46.9±10.8 | 27.5±4.2 | 26.0±2.5 |
| Base-apex DD (mm) | 78.0±2.6 | 77.8±7.2 | 61.4±6.4 | 55.8±6.4 |
| RV diastolic area (cm2) | 30.5±7.2 | 31.6±8.9 | 13.5±2.2 | 7.0±1.4 |
| RV systolic area (cm2) | 24.6±7.2 | 25.6±8.8 | 6.2±2.1 | 3.9±1.4 |
| LVEI | 1.7±0.3 | 2.0±0.5 | 1.0±0.1 | 1.0±0.0 |
| RV/RA (mmHg) | 63.1±18.0 | 102.4±31.4 | 12.6±7.2 | 22.3±10.7 |
DD: diastolic diameter; LVEI: left ventricular eccentricity index; RV: right ventricle; RV/RA: right ventricular/right atrial gradient in systole.
Comparison of RV contractile reserve parameters (S-wave velocity, TAPSE, RVFAC and SVI) between cases and controls, at rest and at peak exercise, is shown in Tables 5 and 6.
Comparison of right ventricular contractile reserve parameters at rest.
| S-wave velocity (cm/s) | TAPSE (mm) | RVFAC (%) | SVI (ml/m2) | |
| Controls | 12.9±3.1 | 25.7±2.4 | 53.8±14.7 | 33.6±6.2 |
| Cases | 9.4±3.1 | 16.1±4.6 | 19.8±9.7 | 25.8±3.8 |
| p | <0.05 | <0.005 | <0.005 | <0.05 |
RVFAC: right ventricular fractional area change: SVI: stroke volume index; TAPSE: tricuspid annular plane systolic excursion.
Comparison of right ventricular contractile reserve parameters at peak exercise.
| S-wave velocity (cm/s) | TAPSE (mm) | RVFAC (%) | SVI (ml/m2) | |
| Controls | 23.0±7.2 | 31.0±3.5 | 64.4±9.9 | 36.9±5.3 |
| Cases | 13.7±4.8 | 16.8±2.7 | 19.4±14.4 | 24.5±4.8 |
| p | <0.05 | <0.005 | <0.005 | <0.005 |
RVFAC: right ventricular fractional area change; S wave: S wave velocity; SVI: stroke volume index; TAPSE: tricuspid annular plane systolic excursion.
The echocardiographic parameters used to assess RV contractile reserve at rest and at peak exercise were significantly different between cases and controls.
The echocardiographic parameters used to evaluate RV contractile reserve and their comparison between rest and peak exercise in the two populations are shown in Tables 7 and 8.
Comparison of right ventricular contractile reserve parameters between rest and peak exercise in cases.
| S-wave velocity (cm/s) | TAPSE (mm) | RVFAC (%) | SVI (ml/m2) | |
| Rest | 9.4±3.1 | 16.1±4.6 | 19.8±9.7 | 25.8±3.8 |
| Peak exercise | 13.7±4.8 | 16.8±2.7 | 19.4±14.4 | 24.5±4.8 |
| p | <0.05 | NS | NS | NS |
RVFAC: right ventricular fractional area change; SVI: stroke volume index; TAPSE: tricuspid annular plane systolic excursion.
Comparison of right ventricular contractile reserve parameters between rest and peak exercise in controls.
| S-wave velocity (cm/s) | TAPSE (mm) | RVFAC (%) | SVI (ml/m2) | |
| R | 12.9±2.3 | 25.7±2.4 | 53.8±14.7 | 33.6±6.2 |
| PE | 23.0±7.2 | 31.0±3.5 | 64.4±9.9 | 36.9±5.3 |
| p | <0.005 | <0.05 | <0.005 | NS |
RVFAC: right ventricular fractional area change; SVI: stroke volume index; TAPSE: tricuspid annular plane systolic excursion.
In cases (Table 7) there was a significant increase in S-wave velocity from rest to peak exercise but no significant increase in any other parameter (TAPSE, RVFAC or SVI).
In controls (Table 8) there was a statistically significant increase in three of the four parameters assessed – S-wave velocity, TAPSE and RVFAC – but no significant increase in SVI.
The magnitude of change with exercise in echocardiographic parameters of RV contractile reserve between cases and controls is shown in Table 9.
Changes in right ventricular contractile reserve parameters with exercise.
| Δ S-wave velocity (cm/s) | Δ (%) | Δ TAPSE | Δ (%) | Δ RVFAC | Δ (%) | Δ SVI | Δ (%) | |
| Cases | 4.3±3.3 | 46 | 0.6±2.5 | 4 | −0.4±11.8 | −2 | −1.3±5.6 | −5 |
| Controls | 10.1±5.5 | 78 | 5.3±3.8 | 21 | 10.6±5.9 | 20 | 3.3±6.0 | 10 |
| p | <0.05 | <0.05 | <0.05 | NS |
Δ: magnitude of change; RVFAC: right ventricular fractional area change in %; S wave: S wave velocity in cm/s; SVI: stroke volume index in ml/m2; TAPSE: tricuspid annular plane systolic excursion in mm.
There was a significant difference in the magnitude of change in echocardiographic parameters of RV contractile reserve between cases and controls, with the exception of SVI. This was also true for S-wave velocity, which was the only parameter to show a significant increase in both cases and controls.
DiscussionThe definition of PH is based on hemodynamic criteria (mean PAP ≥25 mmHg).1 PH can occur in association with various conditions, and is classified in six clinical groups with specific characteristics.1
RV failure is the leading cause of death in patients with PH, and the ability of the RV to adapt to the progressive increase in pulmonary vascular resistance is the main determinant of functional capacity and survival.7
Ventricular reserve is the ability of the ventricle to respond to exercise or pharmacological stress. When ventricular reserve refers specifically to changes in systolic function with stress, it is called contractile (or inotropic) reserve.4 Contractile reserve depends on various factors, including ventricular contractility, myocardial interstitial fibrosis, ventricular remodeling, ventricular afterload, myocardial perfusion and response to neurohormonal activation.4
The prognostic value of contractile reserve has been demonstrated in several diseases, including heart failure, valvular heart disease and coronary heart disease.4 Its main usefulness is related to the fact that ventricular response to stress has a superior predictive value to parameters assessed at rest.4
The best measure of contractile reserve remains to be defined, although theoretically change in ventricular elastance with dobutamine may be considered the best method.4 In clinical practice, contractile reserve is defined by a change in ventricular ejection fraction and stroke volume, although other measures have been proposed for RV contractile reserve, including TAPSE, S-wave velocity and RVFAC.2,4,5
In our study, we used these three parameters (TAPSE, S-wave velocity and RVFAC) and SVI to assess RV contractile reserve, and since there are no well-defined reference values for these parameters, a healthy population (controls) was used for comparison. These variables were chosen because they are quickly and easily obtained even during treadmill stress echocardiography, and are widely available, and thus easy to use in clinical practice.
The choice of patients in clinical groups 1 and 4 of PH was in order to avoid the possible influence of other variables (cardiac, pulmonary or other) that could confound the results of stress echocardiography, due to functional limitations or cardiac alterations unrelated to PH.
There have been no studies on the assessment of RV contractile reserve with treadmill exercise echocardiography in the context of PH. Our hypothesis was that this assessment could be useful in these patients, as in other diseases, to detect RV dysfunction detection at an earlier stage of disease (even when parameters at rest are normal) or at a more advanced stage (when ventricular dysfunction is already manifest), to enable better prognostic stratification. To demonstrate its prognostic value it will be necessary to study larger cohorts and to correlate their RV contractile reserve parameters with events during follow-up.
Due to its ready availability, echocardiography is used as the first-line imaging modality for non-invasive detection, prognostic assessment and guidance of therapeutic strategies in patients with PH.8 It is also an excellent tool to assess the adaptation of the pulmonary circulation and the right heart to exercise in normal or diseased states9 by determining RV contractile reserve. For this reason, we used treadmill stress echocardiography as it is performed in our laboratory,6 assessing echocardiographic parameters during exercise.
In the context of PH, exercise echocardiography appears to be superior to other stress modalities: it provides a better understanding of the symptoms associated with daily activities9 and the increase in cardiac output with exercise more accurately reflects RV functional capacity when overloaded.10 It also enables assessment of other parameters such as functional capacity, ECG changes, hemodynamics and arterial oxygen saturation.
Stress echocardiography has been used to assess abnormal PAP response in mitral valve disease, with prognostic value,9 and in non-invasive assessment of hemodynamic parameters in patients with PH in order to clarify the pathophysiology of the disease.11 The assessment of RV contractile reserve may be another application of stress echocardiography in PH.
Analysis of the echocardiographic characteristics of our patients showed RV morphologic and functional changes related to PH including increased diameters and areas and increased diastolic LVEI at rest (mean 1.7; a value ≥1.7 is a marker of increased mortality in patients with idiopathic PH12). This parameter increased with exercise in cases (from 1.7 to 2.0), but not in controls. This increase is due to rising PAP during exercise, as reflected by the increase in mean RV/RA gradient from 63 mmHg to 102 mmHg, and the consequent increase in RV pressure overload and septal deviation to the left.
Comparison of RV contractile reserve parameters (S-wave velocity, TAPSE, RVFAC and SVI) between cases and controls, at rest and at peak exercise, showed that they were all significantly different, reflecting different populations and significant RV functional changes in PH patients.
In healthy subjects, all RV contractile reserve parameters increased significantly with exercise, with the exception of SVI. This may be considered the normal RV response to exercise and thus an indication that contractile reserve is preserved.
The non-significant increase in SVI may be due to several factors, both physiological (it has been reported that stroke volume increases mainly in the early stages of exercise, but may decrease in stages near to peak stress4,13,14) and technical (errors in the echocardiographic measurements required to calculate SVI, particularly LVOT diameter and LVOT VTI).
Some reference values for RV contractile reserve parameters have been described in the literature; for TAPSE an increase in 5 mm or a relative increase of 20% (with exercise),47 which is in agreement with the value found by us; for S-wave velocity an increase of >200%4 and for RVFAC an increase >9%5 are described as normal for dobutamine stress,4,5 but no value is reported with exercise. For stroke volume, an increase of 30% (with dobutamine or exercise) is reported,4 which we did not find.
S-wave velocity was the only parameter that increased significantly in cases, with an increase of 46% with exercise. In the control group, the increase was 78%, significantly more than in cases.
Unlike in controls, in cases TAPSE and RVFAC did not increase with exercise. This may be indicative of decreased and/or absent contractile reserve. Nevertheless, all these measurements are dependent on loading conditions, and in cases afterload increased considerably with exercise (RV/RA gradient rose from 63.1±18.0 mmHg to 102.4±31.4 mmHg), which may have influenced the results.
Larger studies will be required to define the best parameter(s) for assessment of RV contractile reserve and the corresponding reference values. The occurrence of events should also be assessed longitudinally during follow-up and correlated with RV contractile reserve parameters in order to determine their prognostic value.
Study limitationsThe main limitation of this study lies in the small population size, which is related to the fact that PH is a rare and physically disabling disease. Patients who may be subjected to stress echocardiography must be selected carefully, which significantly reduces the number of patients able to undergo the study, even in a referral center.
ConclusionsThere were statistically significant differences in S-wave velocity, TAPSE, RVFAC and SVI, at rest and at peak exercise, between cases and controls, reflecting significant differences in RV function between patients and healthy individuals.
This preliminary study has shown that S-wave velocity, TAPSE and RVFAC increase significantly with exercise in healthy individuals and may be good parameters for the assessment of RV contractile reserve. SVI does not appear to be a good parameter to assess RV contractile reserve. S-wave velocity was the only parameter that showed a significant increase in patients with PH.
The magnitude of change with exercise in S-wave velocity, TAPSE and RVFAC differs between cases and controls.
Larger studies are needed to determine the best parameter(s) to study RV contractile reserve, to determine the corresponding reference values and to define their possible role in the prognostic assessment of PH patients.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
















 LVOT: left ventricular outflow tract; RV: right ventricle.'/>
LVOT: left ventricular outflow tract; RV: right ventricle.'/>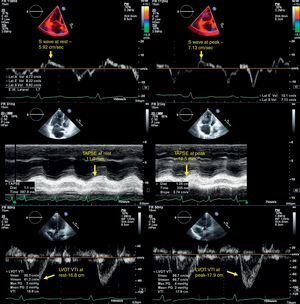 TAPSE; bottom –
TAPSE; bottom –