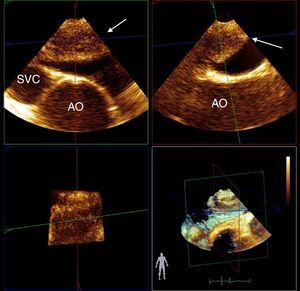
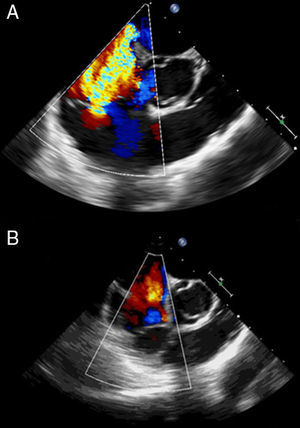
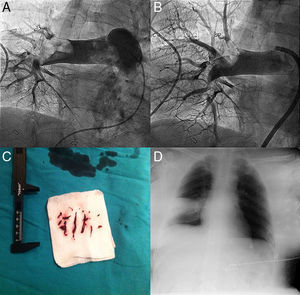
A 40-year-old woman was admitted to the intensive care unit after extensive thoracic burns. During surgical debridement, she experienced rapidly progressive hypoxemia and hypotension requiring high-dose vasopressors, and oxygen saturation remained low despite 100% inspired oxygen concentration. Three-dimensional transesophageal echocardiography was performed, which showed a large thrombus in the right pulmonary artery, extending from the main pulmonary artery bifurcation (Figure 1). It also revealed right ventricular dilatation and severe tricuspid regurgitation (Figure 2A). Given the high bleeding risk associated with recent surgery, a decision was made to perform percutaneous thrombectomy with low-dose intra-arterial fibrinolysis instead of systemic full-dose thrombolysis. Pre-intervention angiography demonstrated a large filling defect in the right pulmonary artery with impaired distal flow (Figure 3A). Abundant thrombotic material was obtained (Figure 3C) and significant improvement in pulmonary circulation was noted (Figure 3B). After the procedure, the patient experienced a dramatic improvement in hemodynamic and respiratory parameters, enabling discontinuation of vasopressors and the use of lower inspired oxygen concentration. Chest radiography demonstrated wedge-shaped pleural based opacities (the “Hampton's hump” sign, Figure 3D). Follow-up echocardiography performed 48 hours later showed resolution of right ventricular dilatation and tricuspid regurgitation (Figure 2B).
Mid-esophageal orthogonal views of the superior vena cava (SVC), ascending aorta (AO) and right pulmonary artery. Three-dimensional (3D) transesophageal echocardiography shows a large thrombus in the right pulmonary artery (white arrow), extending from the main pulmonary artery bifurcation. 3D reconstruction improves the morphological characterization of the thrombus.
Transesophageal echocardiography is useful in the diagnosis of pulmonary embolism in critically ill patients. It may show signs of right ventricular overload and enables direct visualization of thrombi in the right heart or the pulmonary artery. High-risk patients (e.g. those with hemodynamic instability) usually benefit from thrombolytic therapy, but percutaneous techniques are a reasonable alternative when there is significant risk of major bleeding.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.