We present a case of a primary cardiac lymphoma in a 60-year-old woman. The clinical presentation was non-specific and the diagnosis was suggested by its appearance on multidetector computed tomography. The final diagnosis was achieved by histopathological study and was corroborated by a decrease in tumor volume after targeted chemotherapy. A brief review of the appearance of primary cardiac lymphomas in imaging studies is presented.
Os autores apresentam um caso de linfoma cardíaco primário diagnosticado numa mulher de 60 anos. Enquanto que a apresentação clínica foi inespecífica, o diagnóstico foi proposto por tomografia computorizada. O diagnóstico definitivo foi efetuado por histopatologia. A redução do volume tumoral após quimioterapia dirigida corroborou o diagnóstico. A propósito do caso clínico foi efetuada uma breve revisão da expressão radiológica dos linfomas cardíacos primários.
A 60-year-old woman with a history of inferior myocardial infarction presented to the emergency department due to chest pain and recurrent episodes of syncope. Physical examination was unremarkable except for mild ectasia of the superficial thoracic wall vessels and regular bradycardia. The ECG showed de novo atrial fibrillation (AF) and a junctional rhythm of 40 bpm. Laboratory tests were unremarkable, except for elevated lactate dehydrogenase (LDH) of 768 UI/l (normal 240–480 UI/l). Transthoracic echocardiography (TTE) showed no significant abnormality.
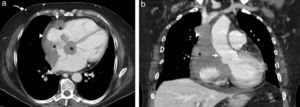
Pacemaker implantation for symptomatic bradycardia was proposed. During the fluoroscopy-guided transsubclavian vein positioning of the pacing leads, complete obstruction of the superior vena cava (SVC) was noticed, and the procedure was aborted. To elucidate the obstruction, a chest multidetector computed tomography (CT) scan was performed (BrightSpeed® 16 slice, GE Healthcare, Milwaukee, Wisconsin, USA) before and after intravenous contrast administration (120 ml of iopromide [Ultravist 370] at a rate of 3.5 ml/s) (Figure 1). Contrast-enhanced CT (non-ECG-gated) showed an infiltrative, hypoattenuating mass, apparently arising from the right atrium (RA) free wall and extending along the interatrial septum and epicardium, through the atrioventricular (AV) groove, following the course of the right coronary artery (RCA). No endoluminal arterial invasion was noted but the mass extended to the RA chamber, occluding the SVC. The mass showed no calcifications or necrosis, revealing mild enhancement. The proximal RCA was patent and a small pericardial effusion was observed.
Axial (a) and coronal reconstructed (b) images from non-ECG-gated enhanced computed tomography, at presentation. A primary cardiac lymphoma (asterisks, a, b) extends through the atrioventricular groove, the right atrial chamber and interatrial septum (asterisks). The patency of the right coronary artery (arrow, a) is preserved. A mild pericardial effusion is present (arrowhead, a) and superficial collateral circulation is shown (curved arrows, a). Coronal reconstructed images better illustrate the sparing of the aortic root (arrow, b) and obstruction of the superior vena cava (arrowhead, b).
A pronounced collateral circulation was evident along the thoracic wall, due to SVC obstruction. Based on the imaging findings the hypothesis of primary cardiac lymphoma (PCL) was proposed.
Histopathology following endomyocardial biopsies revealed a diffuse large B-cell non-Hodgkin lymphoma (CD20+ and BCL6+). Whole-body CT and bone marrow biopsy revealed no extracardiac spread.
A pacemaker for symptomatic bradycardia was finally implanted via the femoral vein.
Chemotherapy with R-COP (rituximab associated with cyclophosphamide, vincristine and prednisolone) was begun.
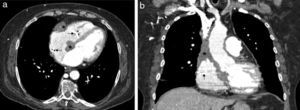
Follow-up CT performed three months later showed moderate decrease in tumor volume (Figure 2).
DiscussionMalignant tumors of the heart are rare and mostly metastatic. Secondary involvement of the heart in the context of a systemic lymphoma is frequently found at autopsy. PCL, i.e. the exclusive involvement of the heart and/or the pericardium by a lymphoma, accounts for only 1.3% of cardiac tumors and 0.5% of extranodal lymphomas.1–3
PCLs are predominantly large B-cell non-Hodgkin lymphomas and can arise from the epicardium or the myocardium, more frequently in the right cardiac chambers and mostly the RA.1–3
The clinical presentation is heterogeneous.2 Several non-specific electrocardiographic abnormalities can be found associated with PCL.4 Complete AV block is the most frequently observed ECG abnormality, as seen in our patient.2,5
The laboratory data are usually non-specific. Elevated LDH is the most notable finding. TTE is frequently the first-line imaging method; TEE often provides satisfactory images of the right atrium,1,2 but previous studies have shown a relatively low sensitivity and specificity.1,2 CT and magnetic resonance imaging (MRI) have an excellent spatial resolution, and can easily depict cardiac tumors and provide visualization of the great vessels, heart, pericardium, mediastinum and lung.2,3 CT usually depicts PCL as an infiltrating epicardial or myocardial mass that is often isoattenuating to hypoattenuating relative to the myocardium. After intravenous contrast, heterogeneous slow enhancement is often shown. The tumor extends along the epicardial surfaces of the heart and AV groove, encasing structures including the coronary arteries and aortic root. These features were present in our case. Pericardial effusion and thickening are common findings.3 MRI may be the best modality to depict the cardiac extension of the disease.3
CT and MRI suggest the differential diagnosis between PCL and angiosarcoma (the most common primary malignancy of the heart) also arising from the RA. Angiosarcomas are extremely invasive through the vessels (coronaries or great vessels) and the valve annular plane. Strong enhancement after contrast is expected in angiosarcomas but not in lymphoma. Central necrosis is also commonly found in angiosarcoma, but is rare in lymphoma.3 Other possible differential diagnosis should include metastatic origin,3 but our patient had no history of extra-cardiac malignancies.
Patients with PCL have a poor prognosis due to late diagnosis and the aggressiveness of the disease.1,2 Prompt diagnosis may allow early treatment and improved prognosis. Contrast-enhanced multidetector CT, along with a high clinical suspicion to detect RA tumors, can improve the early diagnosis of PCL.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.