To assess ambulatory blood pressure monitoring (ABPM) circadian patterns and their determinants in a large sample of normotensive and hypertensive patients.
MethodsA total of 26170 individual ABPM recordings from 1995 to 2015 were analyzed. Mean office blood pressure (OBP), 24-hour blood pressure (BP), daytime BP and nocturnal BP were measured. Circadian patterns were classified by nocturnal systolic BP fall as extreme dipper (ED, ≥20%), dipper (D, 10%-19.9%), non-dipper (ND, 0%-9.9%), and reverse dipper (RD, <0%).
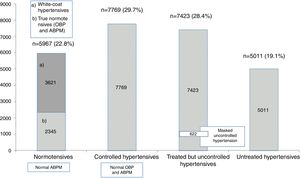
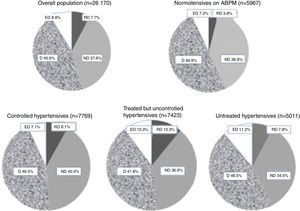
ResultsThe population were 52% female, aged 58±15 years, mean body mass index (BMI) 27±5 kg/m2. Using ABPM criteria of normalcy, 22.8% were normotensives (NT), 19.1% were untreated hypertensives, 29.7% were controlled hypertensives and 28.4% were treated but uncontrolled hypertensives. Among NT, 60.7% were white-coat hypertensive. In controlled hypertensives 62.4% had OBP ≥140/90 mmHg. In treated but uncontrolled hypertensives 8.2% had masked uncontrolled hypertension. ABPM values were lower than OBP in all cases. In all subgroups the most common pattern was D (42-50%), followed by ND (35-41%), ED (7-11%) and RD (4-11%). Age and BMI were determinants of attenuation of nocturnal BP fall and ND+RD. The proportion of ND+RD was higher in patients with BMI >30 kg/m2 vs. others (46.5 vs. 42.9%, p<0.01) and in those aged ≥65 vs. <65 years (54.9. vs. 33.1%, p<0.00). Nocturnal BP fall was greater in NT than in hypertensives (11.3±6.7 vs. 9.9±7.9%, p<0.000).
ConclusionsThere was a marked discrepancy between office and ABPM values. The rates of control on ABPM were more than double those on OBP. Non-dipping occurred in >43%, including in NT. Age and BMI predicted non-dipping.
Avaliar os perfis circadiários da pressurometria ambulatória 24 h (ABPM) numa vasta população de normotensos e hipertensos.
MétodosAnalisaram-se 26 170 registos de ABPM (1995-2015). Avaliou-se a pressão arterial (BP) de consultório (cBP), diurna (dayBP), noturna (nightBP) e de 24-horas (24hBP). Perfis circadiários definidos pela queda percentual noturna (Nqueda %) da pressão sistólica (SBP): extreme dipper (ED>=20%), dipper (D, 10%-19,9%), non-dipper (ND 0%-9,9%) e reverted dipper (RD <0%).
ResultadosPopulação com 52% mulheres, 58+15 anos, IMC 27+5 Kg/m2. Sob critérios de normalidade da ABPM, 22,8% eram normotensos (NT), 18,1% hipertensos não tratados (UnTxHT), 22,7% hipertensos controlados (TxcHT) e 28,4% hipertensos tratados e não controlados (TxnoncHT). Nos NT, 60,7% tinham HT da bata branca. Dos TxnoncHT 8,2% apresentaram HT mascarada. Os valores da ABPM foram sempre inferiores à cBP. O perfil mais frequente foi D (42-50%), seguido por ND (35-41%), ED (7-11%) e RD (4-11%). Idade e o IMC e determinaram o non-dippering e o conjunto ND+RD. A % de RD+ND foi superior nos obesos versus não obesos (46,5 versus 42,9%, p<0,01), e superior se >=65 versus < 65 anos (54,9 versus 33,1%, p<0,00). Nqueda % foi superior nos NT do que nos hipertensos (11,3+6,7, versus 9,9+7,9%, p<0,000).
ConclusãoHá uma marcada discrepância entre a pressão casual e ambulatória; as taxas de controlo tensional por ABPM foram mais do dobro das da pressão casual. O perfil non-dipper ocorreu em 43-49%, inclusive nos normotensos. A idade e o IMC determinaram o fenómeno non-dipper.
Up to 40% of adults worldwide have hypertension.1,2 This high prevalence constitutes a serious public health threat in both developed and developing countries.1–3 Elevated blood pressure (BP) is the most important risk factor for morbidity and mortality worldwide, accounting for more than 15% of all deaths.1–3 It is also the leading risk factor for global disease burden, causing 9 million deaths, 7.6 million premature deaths and 7% of disability-adjusted life years per year.1–3 A continuous relationship between BP and cardiovascular and renal events has been widely reported.2
The diagnosis of clinical hypertension is based on office blood pressure (OBP) measurement.2 However, OBP levels do not always reflect BP in daily life, while diurnal variations and nocturnal dipping, which are important determinants of morbidity and mortality, are not routinely measured.4–6 Besides, OBP measurement only provides a momentary BP value, frequently under circumstances that can influence BP level.5–7 As a result, many hypertensive patients remain unidentified or untreated.8 Additionally, OBP measurement is associated with white-coat hypertension, characterized by a BP rise caused by the presence of a physician.7,9 Masked hypertension, in which OBP is normal but ambulatory BP is raised, carries a similar adverse prognosis to that of sustained hypertension.5,7,8 Thus, 24-hour ambulatory blood pressure monitoring (ABPM) has become a valuable tool in the diagnosis and management of patients with hypertension.4,5,10–12 It has valuable prognostic significance in determining target-organ damage and cardiovascular outcomes,4,5,10–12 since it provides a large number of accurate BP readings throughout both day and night and is highly reproducible.5,6,10 ABPM also identifies white-coat and masked hypertension in both untreated and treated individuals,4–6,9,10 which is probably one of its most valuable indications.4–6,9,10 Additionally, ABPM is essential for assessing BP circadian profiles, including nocturnal hypertension and 24-hour BP variability, as well as for evaluating the 24-hour efficacy of antihypertensive medication.4–6,9,10 ABPM demonstrates the well-known circadian pattern of BP: an early morning surge, lower levels in the evening and a decline when shifting from wakefulness to sleep.7,11–17 This decline may be defined as the nocturnal/daytime BP ratio2,16 or as the percentage decrease in BP during sleep relative to mean BP during daytime activity.6,11 Individuals are then categorized as extreme dippers (≥20% decline), dippers (≥10-19.9% decline), non-dippers (decline <0-10%), and reverse dippers (also known as risers) (<0% decline, i.e., mean nocturnal systolic BP [SBP] higher than mean waking SBP).2,6,11
There is a strong association between the non-dipper/reverse dipper BP pattern and an increased incidence of fatal and non-fatal cardiovascular events.2,11,17,18 Moreover, it has been demonstrated that nocturnal BP is superior to daytime or 24-hour BP in predicting mortality and cardiovascular risk.2,6,11,12,17,18 The relative proportions in very large populations of these circadian patterns and the clinical conditions associated with each have been reported in only a few countries, including Spain,19 but have not so far been examined in Portugal. Thus, the aim of the present study was to determine the prevalence of circadian BP patterns in a broad population recruited from four hospital reference centers in Portugal and to assess certain characteristics (age, gender, body mass index [BMI] and treatment) associated with them.
MethodsStudy participantsA total of 26170 individual ABPM records from 1992 to 2015 were analyzed, from true or suspected hypertensive patients observed or referred to four hypertension centers (Faculty of Medicine of the University of Porto; Moss Clinic, Porto; the Hypertension Unit of Hospital Pedro Hispano, Matosinhos; and Hospital Infante D. Pedro, Aveiro) and from apparently healthy individuals recruited from hospital staff or their relatives. The confidentiality of all data was fully assured. The present study was part of a more extensive one which was approved by the local ethics committee and that incorporated both the inclusion criteria and the analysis of the present substudy. The inclusion criteria were men and women aged ≥18 years with valid ABPM data (at least 85% successful recordings). Exclusion criteria were arm circumference >41 cm or atrial fibrillation or other arrhythmias that could interfere with ABPM recordings. Subjects doing shift work were assessed only during a work period consisting of daytime activity and resting at night.
Blood pressure measurementOBP measurements were taken before ABPM with validated semiautomatic devices after 5 min rest in a sitting position. The OBP value was taken as the mean of three readings taken 2 min apart. ABPM studies were carried out for 24-25 hours on a working weekday with a Spacelabs 90207 (Redmond, WA, USA). Appropriate cuff sizes were used. The patients were instructed to engage in their normal daily activities, but to avoid strenuous exercise and to keep the arm immobile and stop moving and talking at the time of cuff inflation. BP readings were obtained automatically at 20-min intervals during the waking (daytime) period (between 7 am and 11 pm) and at 30-min intervals during sleep (nocturnal) periods (between 11:30 pm and 6:30 am). The absolute and percentage decreases in nocturnal SBP from daytime SBP were calculated in all subjects. The percentage nocturnal SBP fall was calculated as 100×(1-nocturnal SBP/daytime SBP ratio). Patients were classified as extreme dippers (ED) if the nocturnal SBP fall was ≥20%, dippers (D) if ≥10-19.9%, non-dippers (ND) if 0%-9.9% and reverse dippers (RD) if <0%. In order to facilitate comparison between dippers and non-dippers another classification was introduced: all dippers (D+ED) and all non-dippers (ND+RD). All individual data including age, gender, BMI and details of anti-hypertensive treatment were collected at the time of ABPM. All individual ABPM recordings, as well as subjects’ anthropometric data and ongoing treatment, were exported by a macro to a spreadsheet in which all subsequent calculations were performed.
The study that incorporated both the inclusion criteria and analysis of these data was approved by the local ethics committee.
Definition of groupsFor the purposes of the present study, ‘true normotensives’ were defined as: (1) the population of apparently healthy individuals recruited from the hospital staff and their close relatives who over the years were included as a control group in several studies carried out by us and who in a clinical examination had normal BP values, both office and 24-hour ABPM; and (2) those subjects who were initially referred with suspected white-coat hypertension but who subsequently showed normal BP values in OBP assessments as well as on 24-hour ABPM. We additionally included under the classification of ‘ABPM normotensives’ the above true normotensives plus untreated subjects with true white-coat hypertension, i.e. those in whom normal 24-hour ABPM values coexisted with OBP persistently ≥140/90 mmHg. ‘Suspected hypertensives’ were defined as those referred for 24-hour ABPM due to suspicion of white-coat hypertension, and were thereafter classified as true normotensives or white-coat hypertensives. Beyond the classification of ED, D, ND, RD and of D+ED and ND+RD, individuals in the following groups were also analyzed: normotensives on ABPM criteria (mean 24-hour ABPM <130/80 mmHg and nocturnal BP <120/70 mmHg), including subjects with ABPM <140/90 mmHg and OBP ≥140/90 mmHg (white-coat hypertensives), controlled treated hypertensives (mean 24-hour ABPM <130/80 mmHg and nocturnal BP <120/70 mmHg), uncontrolled treated hypertensives (24-hour ABPM ≥130/80 mmHg or nocturnal BP ≥120/70 mmHg) and untreated hypertensives (OBP ≥140/90 mmHg and 24-hour ABPM ≥130/80 mmHg or nocturnal BP ≥120/70 mmHg). In the uncontrolled treated hypertensives group, subjects with abnormal ABPM values but OBP <140/90 mmHg were considered to have masked uncontrolled hypertension.
Statistical analysisData are shown as mean ± standard deviation if normally distributed or as a percentage otherwise. Continuous variables in patient groups were compared by analysis of variance. Categorical variables were compared by the chi-square test. The Student's t test was used for continuous variables and Pearson's test for linear correlations. A value of p<0.05 was accepted as statistically significant. The statistical analysis was performed using SPSS version 22.0 (IBM SPSS Inc., Chicago, IL, USA).
ResultsPopulationThe population were 52% female, aged 58±15 years, mean BMI 27±5 kg/m2. As shown in Figure 1, using ABPM criteria of normalcy,2 22.8% were normotensives, 60.7% of whom had OBP ≥140/90 mmHg (white-coat hypertensives), and the remainder were true normotensives on both OBP measurement and ABPM. Among the overall population, 29.7% were controlled hypertensives, 28.4% were treated but uncontrolled hypertensives on ABPM, including 622 (8.2% of this group) with OBP <140/90 (masked uncontrolled hypertension), and 19.1% were untreated hypertensives.
Circadian patternsAs shown in Figure 2, the distribution of the four circadian patterns in the overall population and in the different subgroups (normotensives, controlled hypertensives, treated but uncontrolled hypertensives, and untreated hypertensives) was fairly similar, particularly in hypertensive subjects. In all subgroups the most common pattern was D (42-50%), followed by ND (35-41%). The ED pattern was found in 7-11% and the RD pattern in 4-11%. There was a slight tendency for D to be more common in normotensives and less common in treated but uncontrolled hypertensives. By contrast, there was a slight tendency for the RD pattern to be more common in treated but uncontrolled hypertensives, and less common in normotensives. As shown in Table 1, there was no difference in the distribution of the four circadian patterns in men vs. women. Obese individuals and elderly subject (>65 years) showed RD and ND patterns significantly more frequently and D and ED patterns significantly less frequently than overweight and normal weight individuals and other age groups, respectively. Table 2 shows the results of multiple linear regression analysis using percentage nocturnal SBP fall as a continuous variable. Age was the most important determinant of absence of normal nocturnal SBP fall. As can be seen, variables such as age and number of antihypertensive drugs (when applicable) were independently associated with the percentage nocturnal fall of SBP in the overall population and in all the different subgroups, whereas the association of BMI was only seen in the overall population and in hypertensives (controlled, uncontrolled, and untreated), but not in normotensives. Female or male gender were not significantly associated with nocturnal SBP fall.
Prevalence of different circadian blood pressure patterns in normotensives, controlled hypertensives, treated but uncontrolled hypertensives, untreated hypertensives, and the overall population. ABPM: ambulatory blood pressure monitoring; D: dippers; ED: extreme dippers; ND: non-dippers; RD: reverse dippers. See main text for detailed definitions.
Proportions of the different circadian patterns according to gender, age group and body mass index.
| % of total | RD | ND | D | ED | |
|---|---|---|---|---|---|
| Men | 47.9% | 7.8% | 37.3% | 45.8% | 9.1% |
| Women | 52.1% | 7.6% | 38.3% | 45.3% | 8.8% |
| Age <40 years | 15% | 1.4% | 29.5% | 59.4% | 9.8% |
| Age 40-65 years | 50% | 5.1% | 29.5% | 52.4% | 12.9% |
| Age >65 years | 35% | 13.9%* | 41.0%* | 36.8%* | 8.3%* |
| BMI ≥30 kg/m2 | 17.5% | 8.4%* | 38.1% | 45.0%* | 8.5%* |
| BMI 25-29.9 kg/m2 | 58.9% | 6.8% | 36.1% | 47.4% | 9.7% |
| BMI <25 kg/m2 | 41.2% | 6.7% | 36.4% | 47.1% | 9.6% |
BMI: body mass index; D: dippers; ED: extreme dippers; ND: non-dippers; RD: reverse dippers. See main text for detailed definitions.
Multiple linear regression analysis of independent variables with nocturnal SBP fall.
| B | SE | Wald | df | Sig | Exp(B) | 95% CI for Exp(B) | |||
|---|---|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||||
| Step 1a | Age | -0.029 | 0.001 | 623.040 | 1 | 0.000 | 0.972 | 0.970 | 0.974 |
| BMI | -0.022 | 0.003 | 40.915 | 1 | 0.000 | 0.978 | 0.972 | 0.985 | |
| Gender | 0.046 | 0.033 | 1.965 | 1 | 0.161 | 1.047 | 0.982 | 1.116 | |
| Constant | 2.646 | 0.121 | 479.459 | 1 | 0.000 | 14.100 | |||
BMI: body mass index; CI: confidence interval; SE: standard error.
Table 3 compares the clinical characteristics associated with the dipping status of two groups, one consisting of subjects with ND or RD circadian patterns (ND+RD) and the other consisting of subjects with D or ED (D+ED), for the overall population and for each of the subgroups (normotensives, controlled hypertensives, treated but uncontrolled hypertensives, and untreated hypertensives). In all the cohorts as well as in both D+ED and ND+RD groups, 24-hour, daytime and nocturnal ABPM values were in all cases lower than OBP values, regardless of normotension/hypertension status. When D+ED and ND+RD were compared in the overall population and in the subgroups, subjects with ND+RD were in all cases older, with higher BMI, and with lower OBP and daytime systolic and diastolic BP and higher 24-hour and nocturnal BP values. For the groups under antihypertensive treatment, the classification of ND+RD was significantly associated with the use of a greater number of drugs, independently of whether they were controlled or uncontrolled. Percentage nocturnal SBP and DBP fall was greater in normotensives than in the other groups.
Clinical characteristics of normotensives, controlled hypertensives, treated but uncontrolled hypertensives and untreated hypertensives according to dippers/extreme dippers and nondippers/reverse dippers.
| ABPM normotensives | Controlled hypertensives | Treated but uncontrolled hypertensives | Untreated hypertensives | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| D+ED | ND+RD | D+ED | ND+RD | D+ED | ND+RD | D+ED | ND+RD | D+ED | ND+RD | |
| n | 3416 | 2551 | 4002 | 3767 | 3878 | 3545 | 2679 | 2332 | 14319 | 11851 |
| Female (%) | 57.9 | 53.9 | 51.9 | 48.2 | 53.1 | 48.2 | 47.2 | 49.4 | 52.4 | 51.6 |
| Age (years) | 48±14 | 53±17* | 58±13 | 64±13* | 61±14 | 65±13* | 51±14 | 57±17* | 55±15 | 62±15* |
| Proportion in the group | 57.3% | 42.7%* | 51.5% | 48.5% | 52.2% | 47.8% | 53.5% | 46.5% | 54.7% | 45.3% |
| BMI (kg/m2) | 26±5 | 27±5* | 27±5 | 28±5* | 28±5 | 29±5* | 27±4 | 28±4* | 28±5 | 29±5* |
| Office SBP (mmHg) | 141±14 | 138±15* | 143±13 | 140±17* | 164±20 | 162±22* | 159±17 | 156±20* | 152±20 | 150±21* |
| Office DBP (mmHg) | 89±11 | 86±11* | 88±12 | 84±12* | 95±15 | 92±16* | 97±13 | 94±14* | 93±14 | 89±14* |
| Office HR (bpm) | 81±15 | 80±14* | 77±15 | 76±15* | 78±18 | 77±15* | 80±14 | 79±15 | 79±15 | 78±15* |
| 24-hour SBP (mmHg) | 120±7 | 122±7* | 119±7 | 121±8* | 141±10 | 145±12* | 139±9 | 143±11* | 130±14 | 132±15* |
| 24-hour DBP (mmHg) | 74±7 | 74±7* | 72±7 | 71±8* | 80±10 | 80±11 | 83±11 | 84±11* | 78±10 | 77±11* |
| 24-hour HR (bpm) | 74±9 | 73±10 | 70±10 | 69±10* | 72±10 | 70±11* | 74±10 | 73±11 | 72±10 | 71±11* |
| Daytime SBP (mmHg) | 126±7 | 124±7* | 125±7 | 122±8* | 148±11 | 147±13* | 146±9 | 145±12* | 136±14 | 134±15* |
| Daytime DBP (mmHg) | 79±7 | 77±8* | 77±8 | 73±8* | 85±11 | 82±12* | 89±10 | 86±11* | 82±10 | 79±12* |
| Daytime HR (bpm) | 77±11 | 76±11 | 73±11 | 72±12* | 75±11 | 72±12* | 78±11 | 75±12* | 76±11 | 74±12* |
| Nocturnal SBP (mmHg) | 107±7 | 117±8* | 106±7 | 117±9* | 124±11 | 142±14* | 122±10 | 139±12* | 115±12 | 129±16* |
| Nocturnal DBP (mmHg) | 64±7 | 69±8* | 62±6 | 67±8* | 68±9 | 76±11* | 71±9 | 80±12* | 66±9 | 73±11* |
| Nocturnal HR (bpm) | 65±9 | 67±10* | 63±9 | 64±10* | 65±10 | 65±10 | 66±9 | 67±11* | 65±10 | 66±10* |
| Nocturnal SBP fall (%) | 11.1±6.4 | 9.8±7.5** | 9.6±8.5** | 10.4±7.5** | 10.4±7.7 | |||||
| Nocturnal SBP fall (%) | 15.3±3.8 | 5.1±4.6* | 15.5±4.0 | 3.9±5.5* | 16.3±4.7 | 2.9±5.9* | 16.2±4.3 | 3.8±5.4* | 15.8±4.3 | 3.9±5.4* |
| Nocturnal DBP fall (%) | 15.8±11.1 | 14.0±9.7** | 13.6±10.1** | 14.7±12.3** | 14.6±10.6** | |||||
| Nocturnal DBP fall (%) | 20.2±8.1 | 8.2±7.6* | 19.9±7.6 | 7.9±8.2* | 20.2±9.2 | 7.0±7.6* | 20.9±10.1 | 7.5±9.1* | 20.3±9.0 | 7.8±8.1* |
| Nocturnal HR fall (%) | 14.1±10.0 | 12.3±9.9** | 11.7±10.7** | 13.9±12.3** | 12.8±10.6** | |||||
| Nocturnal HR fall (%) | 15.4±7.7 | 9.4±6.2* | 13.8±10.6 | 10.7±9.8* | 13.5±11.6 | 9.8±9.6* | 19.9±5.4 | 8.0±6.1* | 19.7±5.7 | 8.2±6.5* |
| Abnormal OBP (%) | 60.6 | 62.4 | 91.8 | 100 | 77.5 | |||||
| Abnormal OBP (%) | 65.1 | 54.5 | 66.1 | 58.9 | 93.7 | 89.7 | 100 | 100 | 80-5 | 73.9 |
| % treated with >2 drugs** | NA | NA | 55.3 | 61.1* | 40.2 | 49.6* | NA | NA | 49.8 | 56.7* |
BMI: body mass index; bpm: beats per minute; D: dippers; DBP: diastolic blood pressure; ED: extreme dippers; HR: heart rate; NA: not applicable; ND: non-dippers; OBP: office blood pressure; RD: reverse dippers; SBP: systolic blood pressure. See main text for detailed definitions.
The present study was the first carried out in Portugal to assess the prevalence of circadian BP patterns in a large population of several thousand and their relationship with OBP and with certain population characteristics. Today there is no doubt of the importance of ABPM in the diagnosis, management and treatment of hypertension.2,6,7,11 Several studies have also shown that data from ABPM are more strongly correlated with target organ damage and cardiovascular prognosis than from OBP.5–9,12,16,17,20–24
The objectives and methodology of our study were similar to those of a recent large population study carried out in Spain,19 although we extended the analysis to more different circadian patterns and to various subgroups of treated, untreated, controlled and uncontrolled hypertensives. The first finding was that at least 43-49% of the population, which includes the normotensive population on ABPM criteria, exhibit attenuation of the nocturnal BP decline. Although this percentage was higher in hypertensives than in normotensives, our data suggest that the ND profile is a very common pattern, including in normotensive subjects. The second finding was that 60.6% of ABPM normotensives showed abnormally high OBP values (white-coat hypertension), as did 62.4% of hypertensive patients controlled on ABPM (hypertensives with white-coat effect). These findings indicate that the rates of control by ABPM are more than double of those by OBP. Also, 8.2% of treated but uncontrolled hypertensives on ABPM showed normal OBP values (masked uncontrolled hypertension). All these findings help confirm the usefulness of ABPM in the management of true and suspected hypertensive patients. A striking finding of the present study, which was not explored in the Spanish study,19 was the proportions of the four common types of circadian patterns (RD, ND, D and ED) in the overall population and in the subgroups. We found that the proportions of these patterns consistently had the same ranking order (D>ND>ED>RD) among all the subgroups of normotensives and hypertensives, irrespective of whether they were controlled, uncontrolled or untreated. As suggested by others,19 the absence of nocturnal SBP decline (as a continuous variable) and the non-dipping patterns (RD and ND) were associated with age and obesity: these patterns were significantly more common in subjects aged >65 years than in those younger than 65, as well as in obese compared to in normal and overweight individuals, and in those receiving a greater number of antihypertensive drugs. The relationship of age and obesity with increased BP is well established,2,3,25 including in Portugal,26 but their relationship with ABPM and particularly with nocturnal BP has only recently become widely recognized.4–6,16,17,19,21,25 It could be speculated that in some patients age and overweight may have been associated with the higher prevalence of the ND pattern due to the potential association with increased risk of sleep apnea. However, unlike the Spanish study,19 in our study gender did not influence the prevalence of the ND profile.
We should point out that the reproducibility of the ND phenomenon has been questioned by some authors,23,27 including by our group.28 However, it is equally questionable for all four circadian rhythm classifications (D, ND, ED and RD), since it has been shown28 that the circadian rhythm classification changes on a second ABPM assessment in at least 47% of individuals. Such concerns are more justifiable in management of an individual patient than when applied to large populations as a whole. In line with this assumption is the fact that in our study the relative proportions and the ranking order (D>ND>ED>RD) of the four circadian types were very similar among normotensive and hypertensives whatever the level of BP control and the presence of medication. Nevertheless, some authors13,19,27 have preferred to consolidate the RD, ND, D and ED types into only two categories, ND+RD and D+ED, in order to minimize the risk of low reproducibility. This is why in our subgroups of normotensives and hypertensives we compared the clinical characteristics of dipping and non-dipping profiles using ND+RD vs. D+ED.
In our study we found that patients receiving antihypertensive drugs had the highest prevalence of the non-dipping patterns. The difference (48.2% vs. 42.7%) was significant only in comparison with normotensives, not with untreated hypertensives. We did not confirm data from others19 indicating a higher prevalence of the ND pattern in treated than in untreated hypertensive subjects. On the contrary, in our study the prevalence of ND was similar in treated and untreated hypertensives. We did not collect data concerning the time at which the medication was given. However, other authors19 who did in fact collect this information showed conclusively that the increase in ND patterns associated with more frequent use of antihypertensive drugs was completely independent of the time at which the medication was given, i.e. that when patients taking medication in the morning, in the evening, or twice a day were compared, no differences in nocturnal BP decline were observed, challenging the advantage of chronotherapy in hypertension management. They also found19 that the proportion of patients taking all or part of their medication at night did not differ between dippers and non-dippers. Thus, one possible explanation for the higher frequency of non-dipping in treated patients may be that patients prescribed more medications may be in more severe medical condition and thus be in more need of treatment. As shown by others,19 the fact that treated patients are more often non-dippers may be because they present higher cardiovascular risk, rather than due to any influence of treatment. The fact that they are in more serious condition makes it plausible that they would exhibit a greater tendency for attenuation of nocturnal BP fall. Several studies4,11,12,17 have in fact suggested that the ND pattern is associated with an increased risk of cardiovascular events.
Our study has some limitations, including its cross-over design and the fact that the classification of the four circadian types and subsequent consolidation into only two categories was based on only a single ABPM recording. As pointed out above, another limitation is the limited reproducibility of circadian patterns based on a single ABPM recording, as we have previously reported.28 Furthermore, this low reproducibility of circadian patterns, as well as the fact that the ND pattern is frequently observed in the normotensive population, clearly suggests that the usefulness of the alleged relationship between non-dipper profiles and cardiovascular risk is questionable and should be re-evaluated. Other limitations relate to the lack of information on other risk factors, such as smoking, diabetes, dyslipidemia, duration of hypertension, African ancestry, high salt consumption, and renal disease, that could be important in increasing the prevalence of the ND profile. However, the study has the merit of assessing a very large population in a way that has never previously been done in Portugal. Also, in contrast to other similar studies,19 it has the advantage of having included a group of normotensives and two subgroups dividing treated subjects into controlled and uncontrolled hypertensives. The high prevalence of white-coat hypertension is probably related to the characteristics of the reference centers to which many patients are referred for 24-hour ABPM based on suspicion of this condition.
In conclusion, our study demonstrates in a very large population that the non-dipping pattern, however it is classified, is a very common condition, including in apparently normal normotensive subjects. Although non-dipping is clearly related to markers of increased cardiovascular risk such as age and obesity, our data suggest that it is not exclusive to high-risk patients, but may be found in apparently normal subjects. This means in practice that non-dipping, although possibly associated by itself with increased cardiovascular risk, should be added to other risk factors and target organ damage in order to establish overall cardiovascular risk. Finally, our study shows that the rates of hypertension control on ABPM are considerably more than double those on OBP, which reinforces the importance of ABPM in the clinical assessment of hypertensive status.
Conflicts of interestThe authors have no conflicts of interest to declare.