The standard of care for acute ST-elevation myocardial infarction (STEMI) includes the activation of a STEMI care network, the administration of adjuvant medical therapy, and reperfusion through primary percutaneous coronary intervention (PCI). While primary PCI is nowadays the first option for the treatment of patients with STEMI, antithrombotic therapy, including antiplatelet and anticoagulant agents, is the cornerstone of pharmacological treatment to optimize their clinical outcomes.
ObjectiveThe aim of this study was to describe contemporaneous real-world patterns of use of antithrombotic treatments in Portugal for STEMI patients undergoing primary PCI.
MethodsAn observational, retrospective cross-sectional study was performed for the year 2016, based on data from two national registries: the Portuguese Registry on Acute Coronary Syndromes (ProACS) and the Portuguese Registry on Interventional Cardiology (PRIC). Data on oral antiplatelet and procedural intravenous antithrombotic drugs were retrieved.
ResultsIn 2016, the ProACS enrolled 534 STEMI patients treated with primary PCI, while the PRIC registry reported data on 2625 STEMI patients. Of these, 99.6% were treated with aspirin and 75.6% with dual antiplatelet therapy (mostly clopidogrel). GP IIb/IIIa inhibitors (mostly abciximab) were used in 11.6% of cases. Heparins were used in 80% of cases (78% unfractionated heparin [UFH] and 2% low molecular weight heparin). None of the patients included in the registry were treated with cangrelor, prasugrel or bivalirudin. Missing data are one of the main limitations of the registries.
ConclusionsIn 2016, according to data from these national registries, almost all patients with STEMI were treated with aspirin and 76% with dual antiplatelet agents, mostly clopidogrel. GP IIb/IIIa inhibitors were used in few patients, and UFH was the most prevalent parenteral anticoagulant drug.
O tratamento do enfarte agudo do miocárdio com elevação do segment ST (EAMCSST) baseia-se na ativação da via verde coronária, na administração de terapêutica médica adjuvante e na reperfusão através de angioplastia primária percutânea. A angioplastia primária constitui o tratamento de primeira linha para o EAMCSST e a terapêutica antitrombótica, incluindo antiagregantes e anticoagulantes, a base do tratamento farmacológico, contribuindo para a melhoria do prognóstico.
ObjetivoDescrever dados contemporâneos da vida real da utilização de terapêutica antitrombótica em Portugal, em doentes com EAMCSST submetidos a angioplastia primária.
MétodosFoi realizado um estudo observacional retrospetivo baseado nos dados de dois registos nacionais referentes ao ano de 2016: o Registo Nacional de Síndromes Coronárias Agudas (RNSCA) e o Registo Português de Cardiologia de Intervenção (RPCI). Foram colhidos dados relativos à utilização de antiagregantes plaquetários e terapêutica antitrombótica endovenosa utilizada na angioplastia primária.
ResultadosDurante o ano de 2016 foram incluídos 534 doentes no RNSCA e 2625 doentes no RNCI com o diagnóstico de EAMCSST submetidos a angioplastia primária. Aproximadamente 99,6% dos doentes foram tratados com ácido acetilsalicílico (AAS) e 75,6% com terapêutica antiagregante dupla (principalmente clopidogrel). Os inibidores do recetor da GpIIbIIIa foram utilizados em 11,6% das angioplastias primárias (principalmente abxicimab). Relativamente à terapêutica anticoagulante, em 78% dos casos foi utilizada heparina não fracionada (HNF) e em 2% heparina de baixo peso molecular. Nenhum dos doentes incluído no registo foi tratado com cangrelor, prasugrel ou bivalirrudina. Os dados omissos são uma das principais limitações dos registos.
ConclusõesEm 2016, de acordo com dados dos registos nacionais, quase todos os doentes foram tratados com AAS e 76% com terapêutica antiagregante dupla, na maioria dos casos incluindo o clopidogrel. Os inibidores dos recetors da GpIIbIIIa foram utilizados num número reduzido de doentes e a HNF foi o principal anticoagulante administrado.
The standard of care for acute ST-elevation myocardial infarction (STEMI)1,2 includes the activation of a STEMI care network, the administration of adjuvant medical therapy, and reperfusion through primary percutaneous coronary intervention (PCI).
Advances in the organizational aspects of health care (such as the Stent For Life initiative3,4) and reperfusion therapy mean that primary PCI is now the established first option for the treatment of patients with STEMI with impact on prognosis.
It is clear that the improved results in STEMI care are largely due to the development of adjuvant medical therapy over recent decades, in particular antithrombotic therapy, including antiplatelet and anticoagulant agents, which is now the cornerstone of pharmacological treatment to optimize clinical outcomes in patients with STEMI undergoing primary PCI.5
2017 marked the 21st anniversary of the publication of the first randomized clinical trial establishing the superiority of dual antiplatelet therapy (DAPT) over anticoagulant therapy among patients undergoing PCI.6 The subject of over 35 randomized clinical trials, including more than 225 000 patients, DAPT is among the most intensively investigated treatment options in the field of cardiovascular medicine.7
DAPT with aspirin and an oral P2Y12-receptor inhibitor is pivotal for the acute and long-term treatment of patients with STEMI undergoing primary PCI. Prasugrel and ticagrelor provide a more prompt, potent, and predictable antiplatelet effect than clopidogrel, which translates into better clinical outcomes. Therefore, these agents are the first-line treatment in primary PCI. However, patients can still experience adverse ischemic events, which may be in part due to alternative pathways triggering thrombosis.
Intravenous anticoagulant drugs available for primary PCI include the indirect thrombin inhibitors unfractionated heparin (UFH) and low molecular weight heparin (LMWH), and the direct thrombin inhibitor bivalirudin. The main intravenous antiplatelet drugs are glycoprotein (GP) IIb/IIIa inhibitors, which should only be considered in bailout therapy, in the event of angiographic evidence of a large thrombus, slow- or no-reflow, and other thrombotic complications, and the P2Y12-receptor inhibitor cangrelor.5
Since several new antithrombotic therapies have emerged in recent decades for the treatment of acute coronary syndromes (ACS), we aimed to describe contemporaneous real-world patterns of use of antithrombotic treatments in Portugal for STEMI patients undergoing primary PCI, through a cross-sectional observational study, based on data from national registries.
MethodsAn observational, retrospective cross-sectional study was performed for 2016 in order to assess the contemporaneous use of adjuvant antithrombotic therapy in patients treated with primary PCI in Portugal.
Data on oral antiplatelet and procedural intravenous antithrombotic drugs were retrieved from two registries: the Portuguese Registry on Acute Coronary Syndromes (ProACS; ClinicalTrials.gov identifier NCT01642329) and the Portuguese Registry on Interventional Cardiology (PRIC; ClinicalTrials.gov identifier NCT01867801).
The PRIC database is a prospective observational registry of PCI in interventional cardiology units in Portugal that includes data from 25 centers. The ProACS database is also a multicenter prospective observational registry, and includes data on patients hospitalized due to ACS in 49 centers.
The ProACS registry was used to assess data on oral antithrombotic drugs (prescribed and taken throughout hospital stay) and the PRIC registry was used to assess data on procedural intravenous antithrombotic treatment (antiplatelet and anticoagulant drugs).
This was a descriptive study and all variables were presented as frequencies and percentages. No inference analysis was performed. The plots were derived from Microsoft Excel®.
All data collection for the Portuguese Society of Cardiology's National Center for Data Collection in Cardiology (http://www.spc.pt/CNCDC/) and the registry procedures are in accordance with the rules of the Portuguese National Data Protection Authority. The registry was approved by the Portuguese Society of Cardiology's ethics committee. This report was approved by the coordinators of PRIC and ProACS.
ResultsIn 2016, ProACS enrolled 534 STEMI patients treated by primary PCI, while PRIC reported data on 2697 STEMI patients. Table 1 shows the characteristics of patients enrolled in the two registries.
Characteristics of ST-elevation myocardial infarction patients treated by primary percutaneous coronary intervention in the two registries.
| PRIC | ProACS | |
|---|---|---|
| n | 2697 | 534 |
| Age, years | 62.9 (13.3) | 62.3 (13.4) |
| Male | 75.2% | 77.3% |
| Risk factors | ||
| Smoking | 39.5% | 38.0% |
| Diabetes | 21.5% | 20.5% |
| Hypertension | 55.0% | 55.8% |
| Dyslipidemia | 41.1% | 50.0% |
| Comorbidities | ||
| Previous MI | 11.1% | 7.9% |
| Heart failure | 1.2% | 1.5% |
| Stroke | 4.1% | 4.3% |
| PAD | 2.1% | 3.0% |
| Chronic kidney disease | 3.7% | 2.8% |
| Previous interventions | ||
| Previous PCI | 12.9% | 7.5% |
| Previous CABG | 2.1% | 0.6% |
| Timings | ||
| Pain-to-balloon time, mina | 235 (145-440) | 252 (166-394) |
| Pain-to-door time, mina | 250 (157-458) | 164 (100-274) |
| Door-to-balloon time, mina | 10 (4-22) | 54 (20-135) |
| Admission | ||
| Killip class I | N/A | 89.7% |
| Killip class II-IV | N/A | 10.3% |
| LVEF <40% | 28.2% | 17.7% |
| Admitted to a PCI center | 92.3% | 62.9% |
| Transferred from a non-PCI center | 7.7% | 37.1% |
| Culprit vessel | ||
| LM | 1.1% | 0.4% |
| LAD | 42.6% | 46.6% |
| Circumflex | 14.8% | 11.3% |
| Right coronary | 37.4% | 41.3% |
| CABG | 0.5% | 0.2% |
| Multivessel disease | 50.9% | 39.5% |
| Arterial access | ||
| Radial | 79.5% | 87.3% |
| Femoral | 19.1% | 12.7% |
| Brachial | 0.4% | N/A |
| PCI with stent | 86.8% | 99.8% |
| DES in at least 1 lesion | 92.5% | 99.6% |
| Thrombus aspiration | 27.1% | 23.6% |
| Complete revascularization | 37.7% | 73.4% |
CABG: coronary artery bypass grafting; DES: drug-eluting stent; LAD: left anterior descending artery; LM: left main; LVEF: left ventricular ejection fraction; MI: myocardial infarction; N/A: not available; PAD: peripheral arterial disease, PCI: percutaneous coronary intervention; ProACS: Portuguese Registry of Acute Coronary Syndromes; PRIC: Portuguese Registry of Interventional Cardiology.
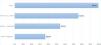
Almost all patients were treated with aspirin (99.6%) and the reported proportion of patients treated with DAPT was 75.6%. Besides aspirin, most of the included patients were still treated with clopidogrel (54.1%) despite the evidence-based efficacy of ticagrelor and prasugrel. Ticagrelor was used in 36.3% of patients (Figure 1). About 15% were prescribed both clopidogrel and ticagrelor in the same episode. No patients were treated with prasugrel or cangrelor.
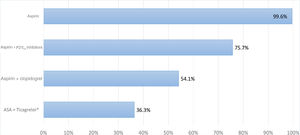
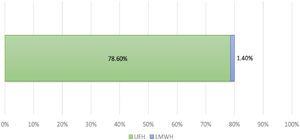
About 80% reported the use of heparin, 78% UFH and 2% LMWH (Figure 2). In patients not treated with heparin, 1% were treated with oral anticoagulants and only 7% received GP IIb/IIIa inhibitors. None of the patients included in the registry were treated with bivalirudin.
GP IIb/IIIa inhibitors were used in 11.6% of cases and abciximab was the most frequently used drug (8.0%) (Figure 3).
DiscussionThis cross-sectional study derived from registry data shows that almost all STEMI patients are treated with antiplatelet agents, and three-quarters with dual antiplatelet agents, mostly clopidogrel. The proportion receiving DAPT would be expected to be higher (particularly in patients undergoing primary PCI), and the main antiplatelet agent used was also surprising. The low proportion receiving DAPT may be due to incomplete registry data. The preponderance of clopidogrel can be explained by the late granting of reimbursement (December 2013) for ticagrelor in Portugal and its unavailability in some catheterization laboratories and prehospital emergency transport. There was also 15% concomitant use of clopidogrel and ticagrelor, which suggests a switch in P2Y12 inhibitors, moving to ticagrelor (to improve the antithrombotic effect) or to clopidogrel (e.g. need for DAPT and anticoagulation, inability to tolerate ticagrelor, or patient preference).
GP IIb/IIIa inhibitors were used in almost 12% of the patients, presumably as bailout therapy or in patients with high thrombotic burden.5 The choice of agent appeared to be related to the greater quantity of evidence available on abciximab, even though this is not in the context of background treatment of STEMI.
UFH was still the most used anticoagulant, and no cases of bivalirudin use were recorded. According to the registry data, about 20% of the patients did not receive intravenous anticoagulation, which may be due to incomplete filling of records (missing data reached 25%) or to cases in which previous administration of oral anticoagulants was not entered into the record.
Earlier data from ProACS showed that in the period 2002-2008 the rate of DAPT was 47%, GP IIb/IIIa inhibitor use was 20%, and UFH and LMWH were used in 37% and 83% of patients, respectively.8 In 2010-2011 100% of the subpopulation with STEMI and multivessel disease in ProACS were prescribed DAPT.9 In PRIC, the analysis of 2006-2012 showed use of GP IIb/IIIa inhibitors in 31% of STEMI patients treated by primary PCI.10 For the period 2006-2012, the PRIC showed a similar pattern of heparin use to our contemporaneous analysis, with 74% of STEMI patients using UFH and 3% using LMWH (unpublished data).
The rate of DAPT use was lower than expected, which may be explained by missing data or incorrect submission of information. Findings from some other registries were better than the results reported here. According to the Polish ORPKI national registry, in 2015/2016 the rate of DAPT in STEMI patients was 80%.11 The Japanese J-AMI registry (2011) revealed that DAPT was used in 85% of STEMI patients, 6% received triple antiplatelet therapy (adding cilostazol), 6% single antiplatelet therapy and 3% no antiplatelet therapy. In Australia (2009-2016), the rate of DAPT in patients discharged with ACS was 70.4%, but the proportion reached 87% in STEMI patients. In fact, STEMI was a predictor of DAPT prescription.12
In the Italian EYESHOT registry, the proportion of patients receiving GP IIb/IIIa inhibitors, heparins and bivalirudin in the catheterization laboratory was 29%, 66% and 19%, respectively.13
Cross-sectional studies are limited by the methodologies used in the registries, and in this case the data are collected on a voluntary basis and are not subject to external audit. In most centers, data are entered directly into the computer system during the interventional cardiology procedure, which results in reliable demographic, clinical, angiographic, and logistic data. However, fewer data are entered on in-hospital course and follow-up, limiting any update on the use of drugs. The rate of missing data on at least one characteristic (demographic or risk factors, medical history, or in-hospital medication) was significant, about 25%, and is a bias factor that should be acknowledged. This may explain why 24% of the patients were not reported to be on DAPT, and why the rate of PCI performed without heparin or other antithrombotic drugs was so high.
ConclusionsAdvances in antithrombotic treatment have led to significant improvements in the prognosis of patients with STEMI treated with primary PCI. In 2016, according to data from these national registries, the majority of STEMI patients were treated with DAPT, GP IIb/IIIa inhibitors were used in 12% of these patients, and in most cases UFH was the parenteral anticoagulant drug of choice for STEMI patients.
Conflicts of interestThe authors have no conflicts of interest to declare.