A 32-year-old man was referred to the cardiology outpatient clinic due to a malformation of the mitral valve (MV). The patient was asymptomatic and had no relevant medical history. The physical examination was unremarkable except for the presence of an apical systolic murmur. To obtain a better understanding of the MV anatomy, three-dimensional transesophageal echocardiography (TEE) was performed that revealed thick and redundant MV leaflets with systolic ballooning of the anterior leaflet (Video 1A and B: blue arrow) and the presence of a fixed hyperechogenic membranous mass attached to the ventricular side of the anterior MV leaflet (Video 1A, B and D: yellow arrow). There was grade II/IV mitral regurgitation (Video 1C and Supplementary Figure S1A) and no signs of MV or left ventricular outflow tract (LVOT) obstruction.
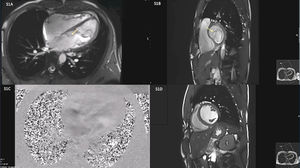
Cardiac magnetic resonance (CMR) was performed to rule out other congenital heart anomalies or myocardial disease. Findings on CMR were suggestive of accessory mitral valve tissue (AMVT) type IB (fixed membranous)1 (Supplementary Video S1A and Supplementary Figure S1B: yellow arrow). Additionally, the CMRI confirmed the presence of two slightly asymmetric papillary muscles (Supplementary Figure S1B).
The clinical case was discussed, and it was decided to adopt a conservative approach. After a three-year follow-up the patient remained asymptomatic with no cardiovascular events.
AMVT is a rare congenital malformation that is frequently associated with other congenital heart disease.1 Few cases have been reported in the literature and the diagnosis remains challenging, with some controversy regarding classification.1 Current literature does not recommend prophylactic removal of isolated AMVT in asymptomatic patients with no LVOT obstruction.1 This case highlights the pivotal role of echocardiography in the diagnosis, treatment and follow-up of this rare disease.
FundingThere were no external funding sources for this study.
Conflicts of interestThe authors have no conflicts of interest to declare.
The following are the supplementary data to this article: