The aim of the present paper is to report trends in Portuguese interventional cardiology from 2004 to 2013 and to compare them with other European countries.
MethodsBased on the Portuguese National Registry of Interventional Cardiology and on official data from the Directorate-General of Health, we give an overview of developments in coronary interventions from 2004 to 2013.
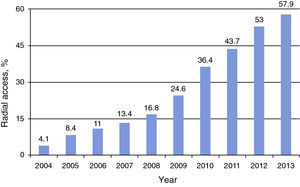
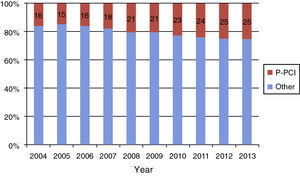
ResultsIn 2013, 36810 diagnostic catheterization procedures were performed, representing an increase of 34% compared to 2007 and a rate of 3529 coronary angiograms per million population. Coronary interventions increased by 65% in the decade from 2004 to 2013, with a total of 13897 procedures and a rate of 1333 coronary interventions per million population in 2013. Primary percutaneous coronary intervention (PCI) increased by 265% from 2004 to 2013 (1328 vs. 3524), an adjusted rate of 338 primary PCIs per million, representing 25% of total angioplasties. Stents were the most frequently used devices, drug-eluting stents being used in 73% in 2013. Radial access increased from 4.1% in 2004 to 57.9% in 2013.
ConclusionInterventional cardiology in Portugal has been expanding since 2004. We would emphasize the fact that in 2013 all Portuguese interventional cardiology centers were participating in the National Registry of Interventional Cardiology, as well as the growth in primary PCI and increased use of radial access.
Foi nosso objetivo estudar as tendências da intervenção coronária percutânea entre 2004-2013 e comparar Portugal com outros países europeus.
MétodosAnálise dos procedimentos coronários efetuados entre 2004-2013 com base num registo prospetivo, multicêntrico, voluntário, doente a doente – Registo Nacional de Cardiologia de Intervenção (RNCI) da Associação Portuguesa de Intervenção Cardiovascular da Sociedade Portuguesa de Cardiologia (APIC-SPC) – e dos dados oficiais publicados pela Direção Geral de Saúde (DGS).
ResultadosEm 2013 realizaram-se 36810 cateterismos diagnósticos (3529 coronariografias por milhão de habitantes), representando um aumento significativo de 34% relativamente ao ano de 2007 (p<0,001). As intervenções coronárias percutâneas (ICP) cresceram 64% desde 2004, atingindo um total de 13897 procedimentos e uma taxa de 1333 por milhão de habitantes no ano de 2013 (p<0,001). A angioplastia primária (ICP-P) cresceu 265% (1328 versus 3524) atingindo uma taxa de 338/milhão, o que representou 25% do total de angioplastias efectuadas em 2013. Os stents foram o dispositivo intracoronário mais utilizado, com uma taxa de stents eluidores de fármaco de 73% em 2013. O acesso radial passou de 4,1% em 2004 para 57,9% em 2013 (p<0,001).
ConclusõesA cardiologia de intervenção mantém uma tendência de crescimento desde 2004 a 2013. Neste ano, a totalidade dos centros de cardiologia de intervenção portugueses estavam a exportar os dados para o RNCI, destacando-se o aumento relativo da angioplastia primária e o incremento do acesso radial.
Portuguese Association of Cardiovascular Intervention
National Center for Data Collection in Cardiology
drug-eluting stents
Directorate-General of Health
European Association of Percutaneous Cardiovascular Interventions
intravascular ultrasound
optical coherence tomography
percutaneous coronary intervention
National Registry of Interventional Cardiology
Portuguese Society of Cardiology
ST-elevation myocardial infarction
The Portuguese Society of Cardiology (SPC) established the National Registry of Interventional Cardiology (RNCI) in 2002 with the aim of providing a prospective and continuous record of percutaneous procedures and patient characteristics in Portugal.1 In parallel, the Directorate-General of Health (DGS) publishes official data based on surveys conducted in interventional cardiology centers.3
We have previously reported developments in interventional cardiology in Portugal from 1992 to 2003.4 We now present data from 2004 to 2013 and analyze trends in Portuguese interventional cardiology over the last 20 years (1992–2013).
In any analysis of this activity it is important to make comparisons with other countries, particularly within Europe. Meier et al. published European data for several years,5,6 but this has not been the case in recent years, and so we opted to compare Portugal with Spain and Switzerland. Spain has published annual data since 1990, and as a European country bordering Portugal, it is probably the closest to Portugal in economic and cultural terms.7,8 Switzerland has also regularly published data on its activity in this area, which enables comparison with a different context that is more representative of northern and central Europe.9,10
MethodsThe RNCI is a voluntary, prospective, multicenter patient registry, compiled according to the Cardiology Audit and Registration Data Standards for clinical cardiology practice2 and centralized in the National Cardiology Data Collection Center (CNCDC), under the aegis of the Portuguese Association of Cardiovascular Intervention (APIC) of the SPC. Between 2004 and 2013, 113971 percutaneous coronary interventions (PCIs) were recorded. The RNCI has progressively included a greater percentage of all procedures performed over the years under analysis. The official data published by the DGS regarding the total number of coronary angiograms and PCIs, collected by annual surveys sent to interventional cardiology centers, are complementary to the RNCI, and the data presented, expressed as numbers and percentages, are based on the RNCI.
To compare our experience with that of Spain we used the annual reports of the Hemodynamics and Interventional Cardiology Section of the Spanish Society of Cardiology (1990–2013)8; for the comparison with Switzerland, we used the data published by Micha et al.9 for 2010 and the data presented for 2013 by the Swiss Working Group of Interventional Cardiology and Acute Coronary Syndromes, as reported by Gregor Fahrni and kindly made available by Meier et al.10
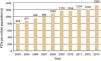
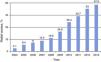
The percentage of patients included in the RNCI has progressively increased. For the first year of the period under analysis (2004), the sample represented only 46% of all procedures in that year, while in the last two years practically all patients treated in Portugal were included (Figure 1), with a slight decrease in 2013.
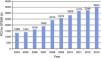
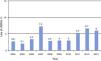
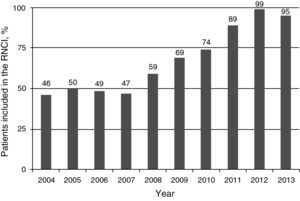
ResultsCoronary angiographyNo official figures have been published on coronary angiograms between 2004 and 2006.3 The total number of coronary angiograms in 2007 was 27746, while in 2013 it was 36810, an increase of 33% (Figure 2). In 2013, 3539 angiograms were performed per million population.
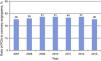
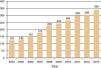
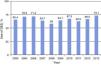
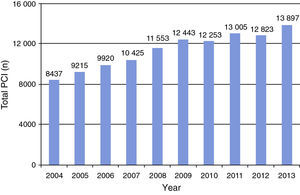
Percutaneous coronary interventionFrom 8437 PCIs performed in Portugal in 2004, this figure rose continuously and significantly to 13897 in 2013 (p<0.001, Figure 3), an increase of 65% and a rate of 1333 PCIs per million population. Figures 3 and 4 summarize developments between 2004 and 2013.
Figure 5 shows changes in the ratio of PCIs to coronary angiograms, which in 2013 stood at 0.38.
With regard to interventions in more complex coronary lesions, the percentage of multivessel PCI has remained relatively stable since the start of the registry, albeit with some fluctuations: from 18% in 1992 to a peak of 24% in 2004, and back to 18% in 2013 (Figure 6).4 PCI for unprotected left main disease varied between 2.8% and 1.9%, the latter in 2013 (Figure 7).
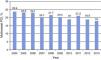
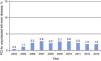
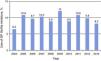
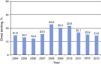
Primary PCI for ST-segment elevation myocardial infarction (STEMI) showed a progressive increase between 2004 (1328 procedures) and 2013 (3524 procedures) (Figure 8). The rate of primary PCI was 338 per million population in 2013 (Figure 9). There was also a parallel increase in primary PCI as a percentage of the total procedures performed in interventional cardiology centers, reaching 25% in 2013 (Figure 10).
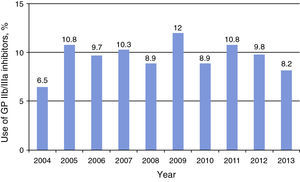
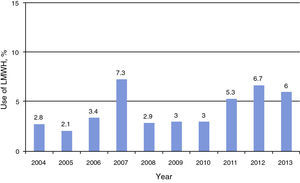
Use of glycoprotein IIb/IIIa inhibitors in the period under analysis varied between 6.5% and 12.0% (Figure 11), with percentages close to those reported in Spain for 2013 (8.2% in Portugal and 10% in Spain; Figure 12).
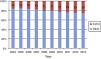
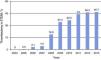
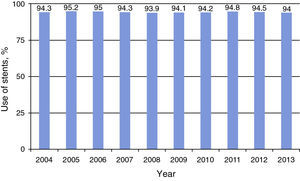
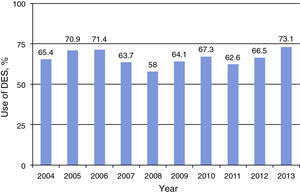
StentingFigure 13 shows that the rate of stent implantation in Portugal for the years under analysis remained stable between 94% and 95%. Use of drug-eluting stents (DES) in the RNCI showed fluctuations, ranging between a minimum of 58% in 2008 to a maximum of 73.1% in 2013 (Figure 14).
Figure 15 shows the rate of direct stenting, with the highest percentages being observed between 2008 and 2010.
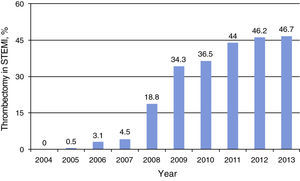
Other interventional cardiology devicesAspiration thrombectomy in the context of STEMI showed a marked increase from 2008, reaching 46.7% in 2013 (Figure 16). Use of distal protection devices in PCI of aorto-coronary bypass grafts varied over the years, and was 12% in the last two years under analysis (Figure 17).
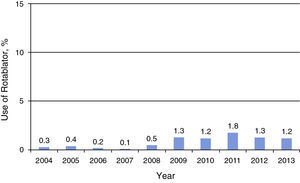
Rotational atherectomy (with the Rotablator device) was used in fewer than 2% of cases (Figure 18). There is no record of use of lasers, brachytherapy or directional atherectomy during the period under study.
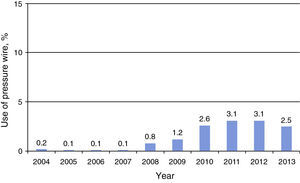
Intracoronary diagnostic techniquesFunctional assessment using pressure wires increased from 2008, reaching a peak in 2011 and 2012 (3.1% of procedures; Figure 19)
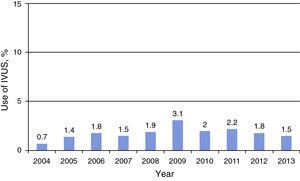
Use of intravascular ultrasound (IVUS) showed an increase up to 2009, when it was used in 3.1% of procedures, but then began to decline, to 1.5% of interventions in 2013 (Figure 20).
Vascular access and closure devicesUse of radial access (Figure 21) increased progressively, reaching 57.9% in 2013, when it was also the most frequently used access in primary PCI (54.6%). Closure devices were used in over 80% of cases of femoral access throughout the period under analysis, reaching 84.8% in 2013.
DiscussionAs mentioned above, there was marked growth in the number of PCI procedures between 1994 and 20084; the growth rate between 2004 and 2008 was 37% but this slowed to 20% in the following five years (2009–2013). After remaining relatively stable between 2010 and 2012, diagnostic procedures increased again in 2013, but this was not accompanied by growth in PCIs, leading to a lower ratio of PCIs to coronary angiograms of 0.38. The ratio between interventions and diagnostic procedures in Spain has been relatively stable since 2007, with a ratio of 0.55 in 2013. There is thus a difference between the two countries, with a larger proportion of diagnostic procedures in Portugal (3539 per million population in 2013 vs. 2592 in Spain) and a smaller proportion of PCIs (1333 per million population in 2013 vs. 1419 in Spain). However, the Spanish registry is not a patient registry, which may bias the comparison. In the Swiss registry,10 the ratio of PCIs to coronary angiograms was 0.48 in 2013, which is higher than in Portugal but lower than in Spain. It should be noted that publication of the COURAGE trial results in 200711 does not appear to have affected indications for interventional cardiology exams since neither the total number of coronary angiograms nor the ratio of interventions to coronary angiograms has decreased.
Assessing Portugal's performance in the European context is important not only for health professionals directly involved in the diagnosis and treatment of patients but also for decision-makers. Meier et al. collected and published data on interventional cardiology in Europe for several years,5,6 but with the exception of primary PCI12 the latest European figures are for 2005.6 The RNCI is unique in Europe since it now collects data from all interventional cardiology centers in the country and most systems enable patient data to be made available online, thus allowing almost instantaneous overall assessment and benchmarking. A robust, high-quality national registry ensures that the data are reliable and guards against the publication of results that may distort the true situation. For example, in the data published by the European Heart Network,13 the rate of PCIs per million population reported for Portugal in 2009 was 229, whereas the true figure was 1163 per million.3
With regard to multivessel PCI, this activity appears to have stagnated over the years. In 2013 the rate in Portugal was 18% of procedures, while Spain reported a rate of 30%.8 This may be because studies have shown that in diffuse multivessel disease, particularly in diabetic patients, PCI may not be the best option.15–17 It may also be related to the fact that increasingly older patients are being treated, with various comorbidities, especially renal failure, in whom a less aggressive approach is indicated, with staged procedures. In addition, from the standpoint of hospital contracts for interventional cardiology programs in Portugal, it is more advantageous to treat multivessel disease in multiple sessions. The good results achieved with second-generation DES18,19 mean that in the 2014 ESC/EACTS guidelines on myocardial revascularization, for the first time PCI for both multivessel and unprotected left main disease is on an equal footing with coronary artery bypass grafting for patients with low or intermediate SYNTAX scores.20
Treatment of unprotected left main disease accounted for 1.9% of all procedures in 2013, a lower percentage than in Spain (3.3%),8 and has remained relatively stable over the period under analysis. The good long-term results reported in the SYNTAX trial14–16 may well have an impact on treatment of unprotected left main disease in Portugal.
Since their introduction in 2002, Portugal has had one of the highest rates of use of DES. Despite a decrease in 2007 (from 71.4% in 2006 to 58.0% in 2008), possibly due to fears of risk of stent thrombosis,21 this soon changed, the rate of use reaching 67.3% in 2010. This fell again in 2011, which was attributed to financial constraints imposed by the economic crisis which favored the use of cheaper bare-metal stents. The rate again rose in 2012, reaching 73.1% in 2013, higher than in Spain (62%) but far lower than in Switzerland (92%).10 One possible explanation for these differences may be the price of stents, which is significantly lower in Portugal and Switzerland than in Spain, making their use more cost-effective.
Direct stenting decreased steadily from 2010. Since anatomical complexity in PCI patients has not increased, this may reflect differences in technique for lesion preparation or possibly use of devices with less efficient delivery systems for economic reasons.
Primary PCI has been the subject of particular attention within the European Association of Percutaneous Cardiovascular Interventions (EAPCI), notably through the Stent for Life initiative.22 The EAPCI considers that Europe should aim for a rate of 600 primary PCIs per million population per year.22–24 In 2013, the rate was 338 in Portugal and 395 in Spain.8 In 2014, Kristensen et al.12 published data for 2010/2011 for 37 European countries, in which only Austria (769), Bulgaria (694), the Czech Republic (596), Germany (638), Hungary (553), The Netherlands (884), San Marino (640) and Switzerland (506) performed over 500 primary PCIs per million per year. Portugal, with 303 per million per year, was in an intermediate group that includes Belgium (297), Finland (265), Greece (346), Greenland (396), Spain (225) and England and Wales (286). This is in contrast to a previous report by Widimsky et al.25 for 2007–2008, in which Portugal was among the countries with a low level of primary PCI. The percentage of primary PCI has progressively increased, accounting for 25% of total procedures in the last year under analysis. PCI in the context of infarction accounted for 26% of overall activity in Spanish centers in 2013.8
Aspiration thrombectomy began to be used more widely in 2008, coinciding with the publication of the TAPAS study.26 Its use in the last three years of the study period approached 50%, and the results of the TASTE trial are awaited to see what impact these will have on future use.27 In Spain thrombus aspiration was used in 67% of procedures in 2013,8 but a retrospective analysis of the RNCI in Portugal showed that the technique had no impact on in-hospital mortality in patients with STEMI.28
Pressure wire assessment of fractional flow reserve increased by 0.8% from 2008, coinciding with publication of the FAME study.29 In 2013, Portugal saw a slight decrease in use to 2.5%, while the rate in Spain was 6.2%,8 which indicates a need for greater experience in this technique in Portugal.
Use of intracoronary diagnostic methods has remained low. The highest rate of IVUS was in 2009 (3.1%) but this fell progressively to 1.5% in 2013, considerably below the Spanish rate of 6.7% for the same year.8 Optical coherence tomography (OCT) was not included in the RNCI, but it appears that use of intracoronary imaging techniques in general has remained stable.
Lastly, use of radial access increased, reaching 53% in 2012 and overtaking femoral access. This figure rose to 58% in 2013, close to the 64% reported in Spain.8
LimitationsWhen assessing activity in interventional cardiology, as well as analyzing trends in the use of various techniques, it is also valuable to analyze clinical and pharmacological parameters, the devices used and outcomes, particularly complications. By the end of the period under study the RNCI included all patients treated in Portugal but the data on clinical follow-up are heterogeneous and should be the subject of a separate analysis; we therefore did not assess the rate of complications. This problem is common to registries that include all patients. Furthermore, there is additional information that should be collected in the future, in particular specifying the number of ad-hoc PCI procedures, drugs used, angiographic features, treatment of chronic total occlusions, type, size and generation of DES, and use of the latest diagnostic methods (OCT and instantaneous wave-free ratio).
Interventional cardiology is no longer focused exclusively on the treatment of coronary artery disease, the main developments now being in the treatment of structural heart disease. It is important to assess current trends in the percutaneous treatment of aortic stenosis, mitral valve stenosis and regurgitation, and hypertrophic cardiomyopathy and closure of shunts, and in the prevention and treatment of ischemic stroke, hypertension and peripheral vascular disease. APIC's working groups have established specific registries for transcatheter aortic valve implantation, renal denervation and atrial appendage closure, which will be published at a future date.
ConclusionInterventional cardiology in Portugal expanded between 2004 and 2013 as assessed by the number of coronary angiograms and PCIs. In the last year under study, all centers involved in this activity contributed individual patient data to the RNCI.
Overall, a relative increase in primary PCI was observed, together with growth in the use of DES and considerably increased use of radial access. Use of intracoronary imaging techniques and invasive functional assessment showed only marginal progress. We have identified variables that should be included in the RNCI in the future.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that no patient data appears in this article.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
We are grateful to Dr. Adriana Belo, biostatistician of the CNCDC, for her help in processing the RNCI data.
Please cite this article as: Pereira H, Teles RC, Costa M, et al. Evolução da intervenção coronária percutânea entre 2004-2013. Atividade em Portugal segundo o Registo Nacional de Cardiologia de Intervenção. Rev Port Cardiol. 2015;34:673–681.





 RNCI: Portuguese National Registry of Interventional Cardiology.'/>
RNCI: Portuguese National Registry of Interventional Cardiology.'/>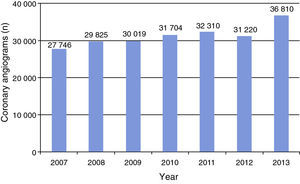
 PCI: percutaneous coronary intervention.'/>
PCI: percutaneous coronary intervention.'/>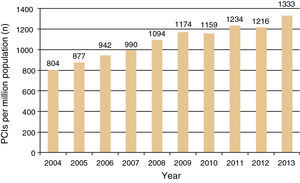 PCI: percutaneous coronary intervention.'/>
PCI: percutaneous coronary intervention.'/>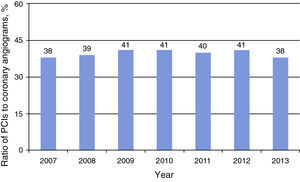 PCI: percutaneous coronary intervention.'/>
PCI: percutaneous coronary intervention.'/>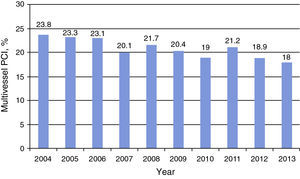 PCI: percutaneous coronary intervention.'/>
PCI: percutaneous coronary intervention.'/>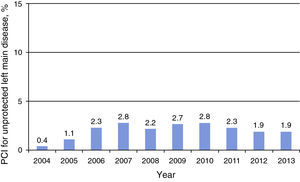 PCI: percutaneous coronary intervention.'/>
PCI: percutaneous coronary intervention.'/>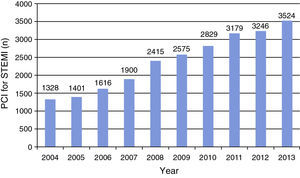 PCI: percutaneous coronary intervention;
PCI: percutaneous coronary intervention; 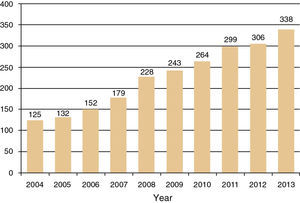
 DES: drug-eluting stent.'/>
DES: drug-eluting stent.'/>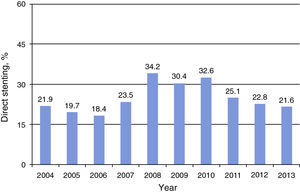
 STEMI: ST-elevation myocardial infarction.'/>
STEMI: ST-elevation myocardial infarction.'/>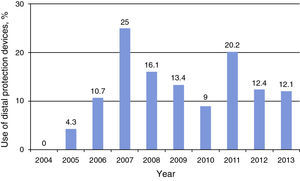
 IVUS: intravascular ultrasound.'/>
IVUS: intravascular ultrasound.'/>