Appointed jointly by the Portuguese Society of Cardiothoracic and Vascular Surgery (SPCCTV) and the Portuguese Society of Cardiology (SPC), the Working Group on Waiting Times for Cardiac Surgery was established with the aim of developing practical recommendations for clinically acceptable waiting times for the three critical phases of the care of adults with heart disease who require surgery or other cardiological intervention: cardiology appointments; the diagnostic process; and invasive treatment.
Cardiac surgery has specific characteristics that are not comparable to other surgical specialties. It is important to reduce maximum waiting times and to increase the efficacy of systems for patient monitoring and tracking.
The information in this document is mainly based on available clinical information. The methodology used to establish the criteria was based on studies on the natural history of heart disease, clinical studies comparing medical treatment with intervention, retrospective and prospective analyses of patients on waiting lists, and the opinions of experts and working groups.
Following the first step, represented by publication of this document, the SPCCTV and SPC, as the bodies best suited to oversee this process, are committed to working together to define operational strategies that will reconcile the clinical evidence with the actual situation and with available resources.
Nomeado em conjunto pela Sociedade Portuguesa de Cirurgia Cardio-Torácica e Vascular (SPCCTV) e pela Sociedade Portuguesa de Cardiologia (SPC), o Grupo de Trabalho sobre Tempos de Espera para Cirurgia Cardíaca constituiu-se com a missão de elaborar recomendações práticas acerca dos tempos de espera clinicamente aceitáveis para o largo espetro de patologias cardíacas do adulto que necessitam de cirurgia, ou de intervenção nas três fases críticas do seu tratamento: consulta de especialidade, ato de diagnóstico e terapêutica invasiva.
A cirurgia cardíaca detém uma especificidade própria, não comparável às outras especialidades cirúrgicas e, como tal, assume-se de especial importância a redução significativa dos seus tempos de espera máximos, assim como uma maior eficácia nos sistemas de monitorização e rastreabilidade do doente.
A informação presente neste manuscrito baseou-se, predominantemente, na informação clínica existente. A metodologia usada para estabelecer os critérios baseou-se em estudos de história natural da doença, em estudos clínicos que compararam o tratamento médico com a intervenção, em análises retrospetivas ou prospetivas de doentes em lista de espera e na opinião de peritos ou de grupos de trabalho.
Após esta primeira etapa, assinalada por esta publicação, a SPCCTV e a SPC devem ser consideradas como as interlocutoras naturais da tutela sobre esta matéria e comprometem-se a colaborar de forma decisiva para a definição de estratégias de atuação, através da adequação da evidência clínica com a realidade e com os recursos disponíveis.
Canadian Cardiovascular Society
national health service
New York Heart Association
Organisation for Economic Co-operation and Development
Integrated System for Management of Waiting Lists for Surgery
Portuguese Society of Cardiology
Portuguese Society of Cardiothoracic and Vascular Surgery
The question of criteria for waiting times for cardiac surgery arises principally in Beveridge-type health systems, in which the State is mainly responsible for funding and providing health care. It is less of an issue in countries such as France, Germany, Switzerland, Belgium and the USA, where health systems are based on the Bismarckian model, in which health care (including surgical interventions) is managed directly between hospitals (and surgeons) and patients and insurers, with or without State support. In this model, there are no problems with the supply of treatment, and access to health care is governed by the patient's resources and/or the coverage and prices set by funding bodies. By contrast, as in the Scandinavian countries and the UK, the Portuguese national health service (NHS) is based on the Beveridge model. In Portugal, resources are limited, and it is thus essential to use them as efficiently as possible to ensure that the support structures of the NHS meet the health care needs of the population, including management of waiting lists.
Waiting times for cardiac surgery in Portugal are longer than those for other types of cardiological intervention, which may indicate inadequacies in the supply of treatment or in patient referral. Waiting times, while covered by the legislation governing the NHS, are also longer than recommended in international guidelines. It has not so far been deemed necessary to differentiate maximum acceptable waiting times for cardiac surgery (such as for aortic stenosis or coronary disease) from those for other types of surgery, such as orthopedic or ophthalmological, in which the consequences of delay are less serious. However, the effects of long waiting times for cardiac surgery are harmful not only in terms of patients’ health and quality of life (worsening of symptoms and more adverse events such as deterioration of ventricular function, myocardial infarction, heart failure or death), but also in economic terms, incurring direct and indirect costs from morbidity, repeated or lengthy hospitalizations, and significant reductions in ability to work for both patients and their families.
A wide range of criteria are used to determine surgical priorities, but specific information is lacking on waiting times for cardiac surgery in both national and international guidelines. Determining priority levels is a complex task for physicians, based on objective and subjective criteria, including the patient's clinical status, the disease, results of diagnostic exams and medical judgment. From the patient's standpoint, it is essential to take account of real total waiting time and to establish guidelines that will ensure clinically appropriate response times for cardiovascular surgery.
Against this background, it was decided to establish a Working Group on Waiting Times for Cardiac Surgery, which was appointed jointly by the Portuguese Society of Cardiothoracic and Vascular Surgery (SPCCTV) and the Portuguese Society of Cardiology (SPC). The aim of the Working Group was to develop recommendations for clinically acceptable waiting times for the wide range of heart disease in adults who require surgery or other cardiological intervention for the three critical phases of their treatment: cardiology appointments; the diagnostic process; and invasive treatment.
On the basis of the conclusions of the Working Group, the SPCCTV and the SPC decided that it was imperative to publish a report, based on scientific evidence and independent of the economic and political systems, defining clinically acceptable maximum waiting times for cardiological interventions and cardiac surgery, bringing waiting times for the two treatment modalities closer together and differentiating cardiovascular disease from other conditions that have less impact on patients’ life expectancy. The various steps and responsibilities involved, including referral for specialist consultations, preliminary studies and referral for surgery, were analyzed and defined. Following the first step, represented by publication of this document, the two societies, as the bodies best suited to oversee this process, are committed to working together to define operational strategies that will reconcile the clinical evidence with the actual situation and with available resources.
Scientific evidence on waiting times for cardiac surgeryThe Working Group sought information and analyzed various publications for the purpose of establishing criteria for the timing of cardiac surgery, with a view to preventing or at least minimizing mortality, morbidity and clinical worsening during the waiting period. The available information is mainly from countries with Beveridge-type health systems, like Portugal, and is of two main types: studies on patterns of clinical referral, and analyses by health authorities on patterns of institutional referral. Establishing clinically acceptable maximum waiting times for different medical conditions is based on studies of the natural history of heart disease, clinical studies comparing medical treatment with intervention, retrospective and prospective analyses of patients on waiting lists, and the opinions of experts and working groups.
The first studies analyzing the consequences of excessively long waiting lists for cardiac surgery were published in the 1990s,2–5 and in 2000 the Spanish Society of Cardiology and the Spanish Society of Cardiovascular Surgery published guidelines defining maximum waiting times for cardiac surgery according to the main types of heart disease and degrees of severity.6 Between 2005 and 2006, the Canadian Cardiovascular Society (CCS) published a series of documents defining benchmarks for cardiovascular exams and procedures.7–9 Despite their limitations, these documents, which were based on various expert consensuses, reignited the debate on the harmful effects of long waiting times, particularly for coronary disease and aortic stenosis, in Canada and the UK. Some studies acknowledge that classifying patients in different priority levels, and changing the level during the waiting period, is not a reliable process.2–4,7,8,10 Such triage, using priority scoring, is difficult to perform and to validate, due to the many possible combinations of risk variables.4 Working groups analyzing the issue have therefore recommended shorter maximum waiting times, classifying patients in only three categories: emergent, urgent and elective.7,10,11 On the basis of longitudinal studies of prospective cohorts, Sobolev and other epidemiologists at the University of British Columbia analyzed the institutional benchmarks in force in Canada and the UK, 26 and 16 weeks, respectively, which are manifestly excessive. In more recent studies on coronary patients, those classified as elective presented a lower risk per unit of time (0.5 per 1000 patient-weeks in the semiurgent group vs. 0.9 per 1000 patient-weeks in the urgent group), and thus had longer wait times. However, if waiting times are too long, the overall risk approaches or exceeds that of urgent patients. The maximum acceptable time on the waiting list for elective patients should take into consideration both risk rate and accumulated risk.12–15 Besides the increased risk with longer waiting time, patients who wait more than the recommended 6 or 12 weeks are more likely to suffer operative mortality.13,14 The 2014 European Society of Cardiology and the European Association for Cardio-Thoracic Surgery guidelines on myocardial revascularization stressed, for the first time, the importance of timings and shorter waiting times.16
The life expectancy of a patient with aortic stenosis and dyspnea is less than two years, and in view of the risk of sudden death, valve replacement is recommended as early as possible.1 For valve disease, the available information is mainly on severe aortic stenosis. A prospective study in Canada on 29293 patients showed that mortality while waiting for valve surgery, isolated or in combination with coronary artery bypass grafting (CABG), was 0.65% and 0.98%, respectively, which was higher than for isolated CABG (0.4%).10 Another Canadian group, studying wait times for access to cardiac catheterization and surgery in stable angina and valvular heart disease, proposed a maximum of six weeks for coronary and valve surgery.11 A recent study on severe symptomatic aortic stenosis revealed mortality on the waiting list of 3.7% and 8.0% at one and six months, respectively,17 while another on severe aortic stenosis showed increased operative mortality in some subgroups, especially those with abrupt symptomatic deterioration from New York Heart Association (NYHA) class I to NYHA III-IV before surgery.18
There is thus some information on the impact of waiting times for ischemic heart disease (IHD) and aortic stenosis, but little for other conditions such as mitral and aortic regurgitation, for which clinical presentation and disease severity as assessed by echocardiography are the determining factors in prognosis. For valve disease, there is ample evidence that intervention at an earlier stage improves long-term prognosis and reduces complications such as atrial fibrillation, persistent ventricular dysfunction and pulmonary hypertension.19,20 Recent data show the harmful effects of changes in the referral system in Portugal, which have led to increased waiting times, hospitalizations, and mortality in patients referred for cardiac surgery.21
The above brief review of the literature demonstrates that in an efficient system, the number of patients placed on the waiting list should equal the number undergoing surgery, and waiting times should be short and adjusted to the patient's risk, and should enable the best allocation of patients and resources. Waiting times for two types of treatment for the same condition (such as CABG and coronary angioplasty) should be similar, to avoid favoring the treatment with the shorter waiting list. The present limit in Portugal of nine months for non-urgent patients is excessive, considering the risks demonstrated in the literature and current practice in other developed countries.
There is therefore a case to be made for positive discrimination in cases of heart disease by reducing maximum waiting times from those currently in force, as has occurred with certain other medical conditions.
Scope of the recommendationsScheduling of surgery in the NHS is managed with the use of software known as SIGLIC (Integrated System for Management of Waiting Lists for Surgery), which sets guaranteed waiting times22 and four priority levels: emergent, urgent, priority and elective. The system can deal with most patients referred for cardiac surgery, but does not distinguish cardiovascular patients from those referred to other specialties.
From the patient's standpoint, what counts is the total time from onset of disease to the date of the operation. However, not all patients are immediately referred for surgery, as there may be alternate forms of treatment or the need for preliminary studies. The current document therefore considers three phases for which there may be a waiting period: cardiology appointments; the diagnostic process; and invasive treatment.
It should be borne in mind that the recommendations presented here apply to all patients, irrespective of health system and care provider. Once priority levels have been defined, physicians can apply them in all situations, while taking into consideration the characteristics of individual patients, some of whom will have complex comorbidities or disease features that require a higher priority. It is essential to take into account the wishes of the patient, who may decide to postpone the procedure, even after the situation has been clearly explained without undue pressure being exerted.
SPCCTV/SPC recommendationsWaiting times for patients referred for surgical or percutaneous treatmentThe Organisation for Economic Co-operation and Development (OECD) recommends that waiting times should be calculated from the patient's standpoint as the total period between first medical contact and the treatment indicated being performed. This period, the “total patient journey”, is made up of the sum of the time taken for referral and diagnosis and time waiting for the procedure.23
Referral timeReferral time is defined as the period between first medical contact and appointment with a cardiologist. Order in Council no. 95/2013 sets out the maximum times to obtain an appointment with a specialist at different levels of priority, ranging between 30 and 150 days. These times are inappropriate for severe heart disease.
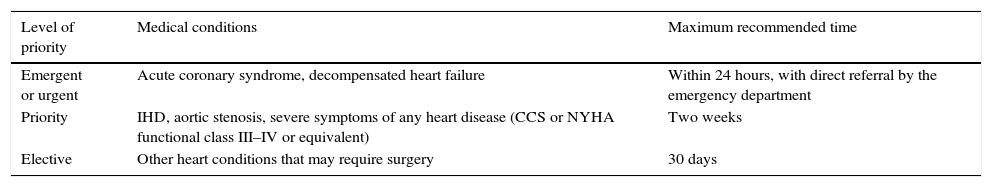
Table 1 shows the proposed recommendations for maximum referral times for cardiac patients who are possible candidates for invasive treatment.
Maximum referral times for appointment with a cardiologist.
| Level of priority | Medical conditions | Maximum recommended time |
|---|---|---|
| Emergent or urgent | Acute coronary syndrome, decompensated heart failure | Within 24 hours, with direct referral by the emergency department |
| Priority | IHD, aortic stenosis, severe symptoms of any heart disease (CCS or NYHA functional class III–IV or equivalent) | Two weeks |
| Elective | Other heart conditions that may require surgery | 30 days |
CCS: Canadian Cardiovascular Society; IHD: ischemic heart disease; NYHA: New York Heart Association.
Time to diagnosis is defined as the period between first appointment with a specialist and definitive diagnosis and referral for surgery. It includes the time taken for the main diagnostic exams required for therapeutic decision-making and for presurgical evaluation, such as echocardiography, computed tomography, magnetic resonance imaging, scintigraphy and catheterization, as well as those needed for characterization of comorbidities and risk. Although not all patients assessed by a cardiologist are indicated for surgery, the decision between surgery, percutaneous intervention or medical therapy is made at this stage.
The first cardiology appointment is the one considered for new patients. However, patients with known heart disease may be seen in follow-up consultations for months or years, only being indicated for possible invasive treatment after developments such as symptomatic worsening, a new result on a diagnostic exam, or an event. In such cases, the clinician or the cardiology department begins the referral process.
Once a definitive diagnosis is established, the next stage is referral for surgery, acceptance depending on the joint decision of the cardiologist and the surgeon. If an appointment with a surgeon or a joint medical and surgical evaluation is required, the time required should be included in the time to diagnosis and the surgical department should respond promptly. Once a patient is accepted for surgery, the priority level is recorded and the patient enters the waiting list at the appropriate point. We propose that the surgical department should respond within two weeks of presentation of the case by the cardiologist for elective patients and in two to four days in urgent cases.
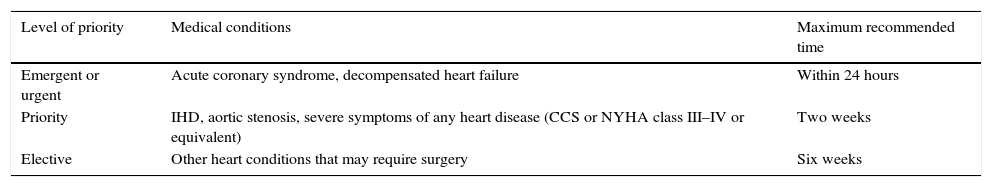
Table 2 presents the recommendations for maximum times to diagnosis.
Maximum times to diagnosis.
| Level of priority | Medical conditions | Maximum recommended time |
|---|---|---|
| Emergent or urgent | Acute coronary syndrome, decompensated heart failure | Within 24 hours |
| Priority | IHD, aortic stenosis, severe symptoms of any heart disease (CCS or NYHA class III–IV or equivalent) | Two weeks |
| Elective | Other heart conditions that may require surgery | Six weeks |
CCS: Canadian Cardiovascular Society; IHD: ischemic heart disease; NYHA: New York Heart Association.
The times include time for multidisciplinary consultations and joint medical and surgical evaluations, which should not exceed two weeks in elective patients.
The time on the waiting list is the period between acceptance for surgery and the operation itself. A patient accepted for surgery is immediately placed on the waiting list and this is communicated to the referring physician and the patient. If the surgeon requests further exams after acceptance, the time taken for these to be performed is counted as part of the waiting period for surgery.
The priority level set according to “functional class or equivalent” is based on clinical status and depends on medical assessment. It may be based on the patient's symptoms, results of functional tests such as myocardial perfusion scintigraphy, or the characteristics of lesions observed on echocardiography or other exams.
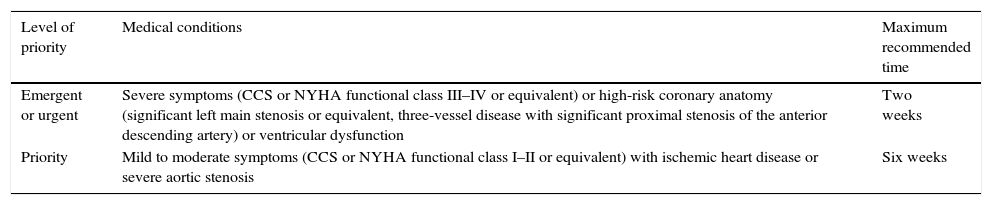
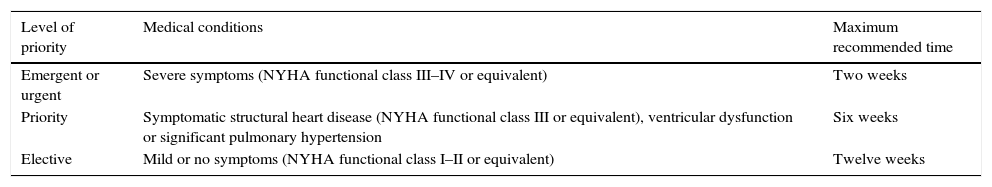
The recommendations for maximum waiting times for patients accepted for cardiac surgery are laid out in Table 3 for IHD and severe aortic stenosis and in Table 4 for other conditions.
Maximum waiting times for cardiac surgery in patients with ischemic heart disease or severe aortic stenosis.
| Level of priority | Medical conditions | Maximum recommended time |
|---|---|---|
| Emergent or urgent | Severe symptoms (CCS or NYHA functional class III–IV or equivalent) or high-risk coronary anatomy (significant left main stenosis or equivalent, three-vessel disease with significant proximal stenosis of the anterior descending artery) or ventricular dysfunction | Two weeks |
| Priority | Mild to moderate symptoms (CCS or NYHA functional class I–II or equivalent) with ischemic heart disease or severe aortic stenosis | Six weeks |
CCS: Canadian Cardiovascular Society; NYHA: New York Heart Association.
Maximum waiting times for cardiac surgery in patients with other conditions.
| Level of priority | Medical conditions | Maximum recommended time |
|---|---|---|
| Emergent or urgent | Severe symptoms (NYHA functional class III–IV or equivalent) | Two weeks |
| Priority | Symptomatic structural heart disease (NYHA functional class III or equivalent), ventricular dysfunction or significant pulmonary hypertension | Six weeks |
| Elective | Mild or no symptoms (NYHA functional class I–II or equivalent) | Twelve weeks |
NYHA: New York Heart Association.
Waiting times in acute coronary syndrome are controversial in view of the lack of evidence based on randomized clinical trials. Only around 10% of patients with acute coronary syndrome undergo surgery in the index hospitalization.23 Given the variability in coronary anatomy, persistence or recurrence of ischemia, hemodynamic status, left ventricular function, thrombotic vs. bleeding risk with antiplatelet therapy, and patient risk, the priority level is usually defined according to medical and surgical criteria.24 The recommendation proposed in this position statement is that these patients should be considered on an equal footing in terms of priority level to patients with IHD and severe aortic stenosis.
Patient monitoring and trackingSIGLIC has adequate information for patients and physicians, as well as compensatory and regulatory mechanisms. However, although in theory the system is capable of managing waiting lists, in practice there are failings in its management of cardiological patients and cardiac surgery. Among the improvements from which its operation would benefit are the following:
- (a)
greater transparency and visibility;
- (b)
better integration with non-surgical waiting lists such as those for specialist appointments and diagnostic exams;
- (c)
auditing of the practices of its users;
- (d)
better communication with patients and their physicians;
- (e)
assessment of the consequences of its use, including mortality while on the waiting list, changes in priority levels, and rehospitalizations.
The fact is that it provides little information, which has hampered recognition of the scarcity of the resources available to meet patients’ needs, particularly for cardiac surgery. In view of the above problems, we propose a system of monitoring waiting times for surgery or percutaneous intervention and the adverse events that occur during this period. The aim of this tracking system is to gather data prospectively that can be analyzed to determine real waiting times and their consequences. Ideally, this registry should also allow retrospective analysis of time spent waiting for consultations with cardiologists and time to diagnosis, since this would enable the total patient journey to be determined, as recommended by the OECD.
It should be mandatory to record the results of joint medical and surgical evaluations and for their decisions to be monitored by the referring cardiology department, overseen by an independent body (governmental or non-governmental). Such a system will provide valuable information on the decisions of the centers involved, as well as on the speed of their responses. Publication and comparison of each center's results will lead to more informed choices and to a better understanding, and correction, of any failings.
Final commentsDuring the preparation of this document, there was general agreement on a series of important points. Firstly, cardiac surgery has specific characteristics that are not comparable to other surgical specialties, and it is important to reduce maximum waiting times, especially for elective patients, and to define them for the three phases of care. Equally important is to recognize that although the system for management of waiting lists for surgery is basically sound, it is in need of significant improvement, and to this end, this Position Statement proposes a monitoring and tracking system.
The lack of consensus concerning patients with IHD or severe aortic stenosis who are asymptomatic and whose functional tests indicate low risk, and who could thus be considered elective, should not be seen as an impasse, but rather as indicating an area in transition that requires further evidence. It should be borne in mind that functional and other types of exam used to determine patient risk in this context have not been studied, and that some of these patients remain under surveillance for long periods without indication for surgery. This suggests that the present recommendations should be reviewed in the near future in the light of forthcoming clinical and scientific evidence, on the basis of data from a national registry of patients referred for cardiac surgery or percutaneous intervention such as we propose should be implemented.
Finally, there are two considerations that may have differing implications for a specific patient and should therefore be mentioned. The first is the time taken for the total patient journey, calculated as the sum of the times taken by the different phases of care. One of these phases may be subject to excessive delay, which has a knock-on effect on subsequent phases. The other consideration is that of who is responsible for managing each phase. Unless the phases and maximum waiting times are clearly defined, there will be considerable pressure on the subsequent phase and an excessive number of urgent operations. In the management of patients awaiting cardiac surgery, the obstacles are not insuperable, and ways can be found to overcome them.
Conflicts of interestThe authors have no conflicts of interest to declare.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that no patient data appears in this article.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
Please cite this article as: Neves J, Pereira H, Uva MS, et al. Recomendações da Sociedade Portuguesa de Cirurgia Cardio-Torácica e Vascular e da Sociedade Portuguesa de Cardiologia sobre tempos de espera para cirurgia cardíaca. Rev Port Cardiol. 2015;34:683–689.