The demonstrated benefits of cardiac resynchronization therapy (CRT) in reducing mortality and hospitalizations for heart failure, improving NYHA functional class and inducing reverse remodeling have led to its increasing use in clinical practice. However, its potential contribution to complex ventricular arrhythmias is controversial.
We present the case of a female patient with valvular heart failure and severe systolic dysfunction, in NYHA class III and under optimal medical therapy, without previous documented ventricular arrhythmias. After implantation of a CRT defibrillator, she suffered an arrhythmic storm with multiple episodes of monomorphic ventricular tachycardia (VT), requiring 12 shocks. Subsequently, a pattern of ventricular bigeminy was observed, as well as reproducible VT runs induced by biventricular pacing.
Since no other vein of the coronary sinus system was accessible, it was decided to implant an epicardial lead to stimulate the left ventricle, positioned in the left ventricular mid-lateral wall. No arrhythmias were detected in the following six months.
This case highlights the possible proarrhythmic effect of biventricular pacing with a left ventricular lead positioned in the coronary sinus venous system.
Os benefícios demonstrados com a terapêutica de ressincronização cardíaca (TRC) na redução da mortalidade e hospitalização por ICC, melhoria da classe funcional e obtenção de remodelagem inversa em doentes selecionados com insuficiência cardíaca (ICC), têm contribuído para a crescente utilização destes dispositivos na prática clínica.
No entanto, permanece controverso o impacto da TRC como fator causador de arritmias ventriculares complexas. Apresentamos o caso duma doente com cardiopatia valvular operada, disfunção sistólica grave e ICC classe III da NYHA, com terapêutica médica otimizada, sem documentação prévia de arritmias ventriculares significativas. Após implantação do sistema de TRC com cardioversor-desfibrilhador, desenvolveu quadro de tempestade arrítmica com múltiplos episódios de taquicardia ventricular monomórfica (TV) e necessidade de 12 choques, mantendo padrão de bigeminismo ventricular reprodutível e indução de salvas de TV pelo pacing biventricular. Dada a inacessibilidade a outra veia tributária do seio coronário foi decidido implantar elétrodo epicárdico em localização diferente (de veia póstero-lateral para posição lateral-mediana), sem registo de recorrência de arritmias num follow-up de seis meses. Este caso sugere que a TRC pode contribuir para um efeito pró-arrítmico com consequências clínicas potencialmente graves.
The benefits of cardiac resynchronization therapy (CRT) in reducing mortality and hospitalizations for heart failure (HF), improving NYHA functional class and inducing reverse remodeling have been amply demonstrated in various multicenter trials in the last 10 years, leading to a considerable expansion of indications for biventricular (BiV) pacing.1–8
CRT can have adverse effects, most of which are related to procedural complications, infection and system malfunction. In recent years there has also been debate concerning the possible contribution of BiV pacing to the occurrence of complex ventricular arrhythmias.
Case reportA 58-year-old female patient with controlled mild hypertension, type 2 diabetes and dyslipidemia was being followed in the cardiology outpatient clinic for valvular HF and permanent atrial fibrillation (AF). She had previously undergone mitral valve replacement with a mechanical valve due to severe mitral stenosis.
During follow-up, progressive clinical deterioration was seen to NYHA class III under optimal medical therapy (OMT). The ECG showed QRS interval of 150 ms and complete left bundle branch block. She had no history of ventricular arrhythmias during follow-up. Serial echocardiograms showed steadily worsening global systolic function, ejection fraction (EF) falling from 24% to 13%. Six years after valve replacement surgery, she had severely impaired global systolic function, with left ventricular (LV) end-diastolic diameter of 82 mm, EF estimated at 13% by the modified Simpson's rule, and echocardiographic criteria of intraventricular dyssynchrony, with tissue synchronization imaging showing septal-lateral delay of 100 ms, two-dimensional strain imaging showing radial strain of 448 ms with inferior-anteroseptal delay but no ventricular dyssynchrony (pulmonary and aortic pre-ejection times of 78 ms and 105 ms, respectively). Right ventricular (RV) function was also impaired, with tricuspid annular plane systolic excursion of 5 mm.
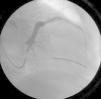
A VVIR mode CRT defibrillator (CRT-D) was implanted with the LV lead positioned in a posterolateral vein (Figure 1) with a different ostium from that of the coronary sinus, the venous system of which was sparse, consisting of small and markedly angulated vessels (Figure 2). In our center, the posterolateral vein is often used when the branches of the coronary sinus are technically difficult to access, although it is generally difficult to characterize. However, this vein is only used as an alternative, since the distance between it and the RV apex gives insufficient time for myocardial activation. Furthermore, the fact that both leads activating the ventricular mass are relatively close could trigger new dyssynchrony by the late activation of more distant areas of the myocardium.
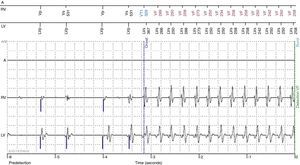
One month after implantation, the patient returned to our department after suffering 12 shocks in 24 hours. Device interrogation revealed these to have been appropriate shocks in response to an arrhythmic storm of multiple episodes of rapid ventricular tachycardia (VT) with a mean cycle length of 250 ms (Figure 3). At the same time reproducible ventricular bigeminy and VT runs induced by BiV pacing were seen. Various programming modes were tested with different pulse polarities, amplitudes and widths, as well as left ventricular pacing alone, none of which eliminated the ventricular extrasystoles. In view of the failure of these attempts, pacing via the left ventricular lead was switched off and the patient regained natural rhythm without ventricular extrasystoles, with RV pacing set to a minimum of 40 bpm. The CRT-D was programmed with three zones: VT-1, from 171 bpm with two bursts of antitachycardia pacing; VT-2, from 182 bpm, with two ramps followed if necessary by a 40-J shock; and VF, from 200 bpm, with up to six 40-J shocks.
Holter 24-hour monitoring performed two months later showed natural rhythm (AF) in 99% of the record, with only 195 isolated dimorphic ventricular extrasystoles, one pair and one 4-complex run. The patient was under medication with amiodarone 200 mg/day and carvedilol 6.25 mg twice daily.
Echocardiography five months after switching off LV pacing showed continuing very low EF (13%) with evidence of intra- and interventricular dyssynchrony; the patient remained in NYHA class III.
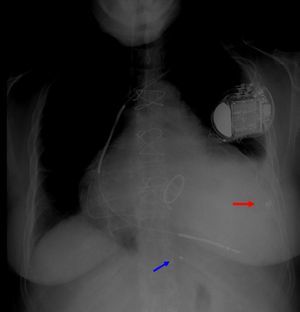
It was decided to make another attempt to implement CRT. Since no other branch of the coronary sinus could be catheterized, an epicardial lead was implanted in the lateral LV wall (Figure 4). The alternative of repositioning the RV lead to a septal position was not chosen because, before CRT implantation, the segments with the latest activation were those of the lateral wall, the distance between the leads would not be significantly increased by this change, and in order to begin pacing via the LV lead it would have to be implanted in a less arrhythmogenic position.
An epicardial lead was implanted between the second and third obtuse marginals by submammary thoracotomy.
One month later, the patient was still in NYHA class III, with poor global systolic function. The LV pacing percentage was 89% and the RV pacing percentage was 13%. The low percentage of BiV pacing is explained by the rapid intrinsic rates resulting from the patient's AF. However, no ventricular arrhythmias were recorded by the device.
Digoxin was added to the patient's therapeutic regime to control her intrinsic ventricular rate, the minimum pacing rate was raised to 80 bpm, and she was enrolled in a cardiac rehabilitation program. We opted for a conservative approach to maximize BiV pacing rate through optimizing medical therapy and reprogramming the device, given the theoretically greater risk of loss of capture by the epicardial lead than if the lead had been positioned in the coronary sinus venous system. If this strategy failed, the next step would be ablation of the atrioventricular node. If the LV lead had been in the coronary venous system, then nodal ablation would have been the first option.
At six months after implantation of the epicardial LV lead and after an increase in the percentage of BiV pacing, the patient was still in NYHA class III, but reported slight symptomatic improvement in her day-to-day activities, and her EF had risen to 19%. No new episodes of decompensated HF occurred and no ventricular arrhythmias were detected by remote monitoring during this period.
DiscussionInitial reports of the impact of CRT on the incidence of ventricular arrhythmias show an antiarrhythmic effect,9,10 which could be due to reduction of wall stress caused by the inverse remodeling induced by BiV pacing, decreased dispersion of ventricular repolarization resulting from dual depolarization wave fronts,11,12 and reduced sympathetic nervous system activation.13
Other studies suggested that this antiarrhythmic effect is due to reductions in the number of ventricular extrasystoles,14 the incidence of tachyarrhythmic events15 and the inducibility of sustained VT.16 More recent research has indicated that this effect is mainly seen in patients who respond to CRT, as a consequence of the hemodynamic improvement induced by BiV pacing,17,18 but not in non-responders.
Indications for CRT have widened in the last 10 years and research into its consequences has intensified, but its electrophysiological effects on the incidence of sudden death and ventricular arrhythmias are still poorly understood.
Cases have been reported of increased arrhythmic events in some patients when treated with BiV pacing.19–21 In 2005, Shukla et al.19 described a series of 145 consecutive patients, five of whom developed arrhythmic storm after implantation of a CRT-D, which was permanently resolved by discontinuing LV pacing. Similarly, Medina-Ravell et al.20 assessed 29 patients who received a CRT-D, four of whom developed ventricular extrasystoles with BiV pacing, eliminated when LV pacing was ended. The same phenomenon is seen in the case presented here.
Further evidence is found in the two largest randomized clinical trials to assess the effects of CRT in patients with and without an implantable defibrillator, which showed a reduction in all-cause mortality compared to OMT (COMPANION4 and CARE-HF5), the percentage of sudden death as a cause of death was slightly higher in those without a defibrillator.22
In the COMPANION trial, there was a statistically significant reduction of 36% in all-cause death (p=0.003) in patients under OMT and CRT compared to OMT only. However, the incidence of sudden death was higher in those under CRT with pacing only plus OMT than in those with OMT only (7.8% vs. 5.8%), while in those with CRT-D and OMT it was only 2.9%. Analysis of causes of death in the three groups shows that sudden death was responsible in 36.6% of patients with CRT with pacing only plus OMT, 23.4% of those with OMT only, and only 16.2% of those with CRT-D and OMT.22
In the CARE-HF trial, although mortality was lower in patients undergoing CRT than in those receiving OMT only, the percentage of the former suffering sudden death was higher (35.4% vs. 31.7%).
However, evidence to the contrary recently came from the REVERSE study, which assessed the incidence of VT/ventricular fibrillation and sustained VT in patients with CRT-D devices, one group with BiV pacing on and the other with pacing off. After two years of follow-up, the incidence of arrhythmic events was similar in the two groups (18.7% vs. 21.9%, p=0.84).23
In the normal sequence of myocardial activation, the endocardium is depolarized before the more epicardial layers, while repolarization travels in the opposite direction (from epicardium to endocardium). BiV pacing is normally effected via an endocardial lead placed in the RV and a lead placed inside the coronary sinus or one of its branches, and so the LV myocardium is stimulated via the epicardium. Epicardial pacing involves a non-physiological activation sequence in which the vector of the transmural propagation is reversed, resulting in delayed endocardial depolarization and earlier epicardial depolarization.24 Experimental studies have shown that epicardial-endocardial conduction time is significantly longer than endocardial-epicardial conduction time, due to a zone of myocardial wall between the deep subendocardium and mid-myocardial layers.25,26 The resulting increased dispersion of repolarization prolongs QT and JT intervals and the interval between the peak and the end of the T wave.25,27
Furthermore, a small number of predisposed patients may be more likely to suffer reentrant phenomena. The presence of cardiomyopathy, use of QT-prolonging drugs, and autonomic dysregulation can also promote these phenomena.28,29
Identification of factors that predispose to ventricular arrhythmias caused by BiV pacing is thus of considerable clinical importance in the assessment of candidates for this therapy and in the decision whether to implant a CRT-D system.
The predictors of arrhythmias in these patients have not been fully identified. In a study of 75 patients undergoing CRT, variation in QT dispersion before and after implantation was an independent predictor of major arrhythmic events; in a follow-up of 807 days, in the group with increased QT dispersion the incidence of events was 29%, while in those in whom it decreased, the incidence was 3% (p=0.0017).30
The same study30 assessed the interval between the peak and the end of the T wave (Tpeak-end), another marker of dispersion of repolarization. Patients who suffered arrhythmic events during follow-up had a significantly smaller reduction in Tpeak-end than those who were event-free (−1.5±12.8 ms vs. −20.0±5.4 ms, p=0.047).
The mechanisms involved in this differing QT dispersion response to CRT have not been investigated. It is thought that factors such as severe systolic dysfunction,29 perfusion disturbances31 and stimulation of LV myocardium in areas close to fibrotic tissue32 could in theory be related to changes in QT dispersion.
Dilated cardiomyopathy is associated with ventricular fibrosis, changes in muscle tissue architecture and abnormalities of cellular ultrastructure, particularly in cell membranes.33,34 The electrophysiological properties of cardiomyopathic myocardium are also altered by lines of conduction block resulting from fibrosis and areas of abnormal conductibility and refractoriness.35 The zones with altered electrophysiological properties are not homogenous throughout the dysfunctional myocardium,36 and the patterns of their distribution appear to differ between ischemic and non-ischemic dilated cardiomyopathy,36 with more diffuse involvement, mainly in the basal segments, in the latter compared to the former, in which these zones tend to be restricted to particular arterial territories and typically affect the endocardium more extensively.37,38 In the case presented, the patient had severe valvular disease and had undergone mitral valve replacement, which may have altered the tissue architecture and hence the distribution of zones with altered electrophysiological properties.
When a pro-arrhythmic effect of BiV pacing is suspected, an alternative site for LV stimulation can reduce arrhythmogenicity. In our patient, the lack of options led us to adopt a surgical approach, and during thoracotomy threshold tests were performed in different parts of the epicardium and the induction of ventricular extrasystoles by BiV pacing was assessed.
Various strategies have been tried to overcome the potential arrhythmic risk of LV stimulation via branches of the coronary sinus, including endocardial LV pacing with the lead positioned via transseptal puncture. Initial results of this procedure, still in the early stages of evaluation, are promising.39,40
Assessment of heterogeneity of repolarization during implantation is considered of little value, since no correlation has been established between changes in these parameters and adverse events, and any pro-arrhythmic effect may only be manifested hours or days after implantation.41
ConclusionCRT is not without adverse effects. Although its benefits clearly outweigh the risks in patients with indication for this therapy, in rare cases BiV pacing may induce arrhythmias. Reversal of the physiological depolarization sequence increases dispersion of repolarization, promoting reentry phenomena and increasing the incidence of ventricular arrhythmias in some patients.
Although the paradoxical increase in arrhythmogenicity with CRT is uncommon, it can have serious clinical consequences that reprogramming alone cannot prevent. In the case presented, only removal of the pacing lead from the coronary sinus eliminated the ventricular arrhythmia. Since ventricular resynchronization was necessary, an alternative site for the LV pacing lead had to be found, and an epicardial approach was the one chosen.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Cabanelas N, Oliveira M, Nogueira da Silva M, et al. Terapêutica de ressincronização cardíaca e efeito pró-arrítmico: um problema que deve ser lembrado. Rev Port Cardiol. 2014;33:309.e1–309.e7.