The classic transvenous implantation of a permanent pacemaker in a pectoral location may be precluded by obstruction of venous access through the superior vena cava or recent infection at the implant site. When these barriers to the procedure are bilateral and there are also contraindications or technical difficulties to performing a thoracotomy for an epicardial approach, the femoral vein, although rarely used, can be a viable alternative.
We describe the case of a patient with occlusion of both subclavian veins and a high risk for mini-thoracotomy or videothoracoscopy, who underwent implantation of a permanent single-chamber pacemaker via the right femoral vein.
A implantação clássica de pacemaker definitivo (PMD) em posição antepeitoral e por via transvenosa pode ser impossibilitada por obstrução dos acessos venosos à veia cava superior ou pela presença de infeção recente no mesmo local. Quando estas barreiras são bilaterais e, concomitantemente, há contraindicação ou dificuldade técnica para uma abordagem por toracotomia para implantação de um eletrocateter epicárdico, a via femoral venosa, embora raramente utilizada, pode constituir uma alternativa viável.
Descrevemos o caso de uma doente submetida a implantação de pacemaker definitivo monocamaral por via femoral direita por apresentar obstrução de ambos os acessos subclávios e limitações importantes à realização de minitoracotomia ou videotoracoescopia para posicionamento de um elétrodo epicárdico.
A 52-year old woman was transferred from her local hospital for implantation of a permanent pacemaker (PPM) in the context of symptomatic, intermittent 2:1 atrioventricular block (AVB).
She had a history of hypothyroidism, controlled by hormone replacement therapy, and surgery for Hodgkin's lymphoma in 1986, followed by chemotherapy and radiotherapy, and is now in remission with regular assessment in hematology consultations.
The patient reported worsening fatigue with dyspnea on minimal exertion and episodes of dizziness for three days, which had led her to visit the emergency department of her local hospital. On admission she presented an irregular pulse at 53 bpm and the ECG showed 2:1 AVB (Figure 1). Laboratory tests showed no ionic changes or thyroid dysfunction and the patient was taking no drugs that would affect atrioventricular conduction. Physical examination revealed extensive superficial venous circulation over the abdomen and chest.
An attempt at PPM implantation using conventional venous access failed due to extensive occlusion of both subclavian veins with widespread superficial and deep vein collateral circulation (Figure 2).
Further cardiological assessment was undertaken with a view to performing the procedure using a different approach. Transthoracic echocardiography showed signs of constrictive physiology, notably early diastolic septal “bounce” with a notch toward the left ventricle and tricuspid inflow respiratory variation of over 25%.
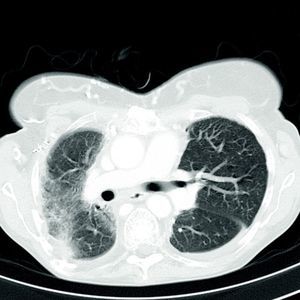
High-resolution thoracic contrast computed tomography (CT) (Figure 3) revealed extensive venous collateral circulation due to obstruction of the superior vena cava, together with marked right pulmonary apical fibrosis and mediastinal deviation to the right. There was minimal space between the posterior face of the sternum and vascular structures (particularly the origin of the supra-aortic trunks at no more than 3 mm) which were in contact with the aortopulmonary window and the right ventricular free wall. The subxiphoid region was in contact with the anterior face of the left hepatic lobe.
Cardiac magnetic resonance imaging confirmed constrictive physiology and excluded pericardial thickening.
In view of the abnormalities detected, particularly diffuse fibrosis of the thoracic cavity, implantation of an epicardial lead was excluded on medical and surgical evaluation.
Following confirmation by CT of the patency of vascular access via the inferior vena cava, it was decided to perform PPM implantation via the right femoral vein.
Given the intermittent nature of the patient's AVB, the embolic risk associated with two intravascular catheters covering a large territory (from the femoral vein to the inferior vena cava and right chambers) in a patient with potential predisposition for venous thromboembolism, and the risk of atrial lead dislodgment, it was decided to implant a single-chamber PPM.
The procedure was performed under general anesthesia. A longitudinal incision was made in the right groin, a few cm below the inguinal ligament, enabling visualization of the femoral vein (Figure 4). The vein was punctured using the Seldinger technique, and a guide wire was inserted into the vessel, followed by a 7F introducer (Medtronic Inc., Minneapolis, MN). A 5.7F, 85-cm bipolar active-fixation lead (CapSureFix® Novus 4076-85, Medtronic Inc., Minneapolis, MN) was inserted through the introducer previously positioned in apical-septal position.
Correct positioning of the lead in apical position was confirmed by detection of a current of injury of >4 mV on the right ventricular electrogram.
Satisfactory sensing and stimulation thresholds were obtained (sensing 6.6 mV; impedance 630 Ω; threshold 0.5 mV at 0.4 ms), and the introducer was withdrawn, leaving a sufficiently large loop in the lead to avoid dislodgement by stretching. The lead was fixed with non-absorbable sutures to the underlying muscle using the suture anchors. A PPM pocket was constructed in the subcutaneous tissue of the lower abdominis muscle on the same side, through a second incision sufficiently above the inguinal ligament to avoid local discomfort (Figure 5). The lead was then tunneled subcutaneously over the femoral ligament from the infrainguinal incision to the pocket, and connected to the pacemaker battery (Adapta, Medtronic Inc.).
The procedure was uneventful and the patient was mobile within 48 hours. The PPM was programmed in VVIR mode with a base rate of 50 bpm, resulting in 35% ventricular pacing, and the system was found to be functioning well in cardiology and cardiac pacing consultations after two years of follow-up, with no recurrence of the previous symptoms of heart failure. She reported no discomfort or complications at the implant site.
DiscussionUnilateral occlusion of the subclavian or innominate vein after pacemaker or defibrillator implantation is relatively common, occurring in approximately 10% of uncomplicated implants. Bilateral occlusion sometimes occurs when both subclavian access sites have been used for previous implantations.1 An epicardial approach is the standard alternative for cardiac pacing in cases of subclavian occlusion.
Epicardial ventricular pacing can be instituted through a small subxiphoid or left lateral incision when thoracic anatomy is favorable. Minimally invasive procedures for epicardial implantation are possible guided by videothoracoscopy. However, thoracotomy is necessary when placing an atrial lead to maintain atrioventricular synchrony to minimize the risk of triggering pacemaker syndrome.
The average operating life of an epicardial lead tends to be shorter than that of an endocardial lead.2,3
As an alternative to epicardial pacing, the subclavian vein in patients with previously implanted leads can be recanalized during extraction of the leads by mechanical or laser dilatation, using the dysfunctional lead as a guide, thus retaining the classical venous route.4,5 However, the risk of perforation or dislodgment can be high when the occlusion is in a territory that has been subjected to radiotherapy.
Almost 33 years ago, El Gamal and Van Gelder6 first described transvenous femoral access for atrial pacing with a Helifix lead.
In the case presented, we accessed the femoral vein directly and inserted the lead well below the inguinal fold to prevent discomfort from the scar. A pocket was created in the abdominal wall, away from the insertion site, to prevent the battery causing any discomfort with thigh movements.
Ellestad et al. also used abdominal wall pockets and reported no major complications in 95 implants.7 Mathur et al. made an incision in the groin skin crease to introduce the lead via the femoral vein, and then fashioned the pocket cranial to the incision; however, they reported skin erosion in two out of 27 patients.8
An increased incidence of lead fractures might be expected given the need to U-turn the leads from the venous entry site to the generator pocket, but this is not an issue mentioned in the literature. The groin is probably a much less mobile region than the subpectoral area, especially in elderly patients, and does not have an equivalent to the clavicle that can inflict crush injuries.
Dislodgment of atrial leads is a real concern, one of the reasons we opted for a single-chamber PPM in our patient. Ellestad et al. and Mathur et al. reported a dislodgment rate of 21% and 20%, respectively, even with the use of active-fixation leads.6,7 Gravity plays an important role, exerting a force on the whole length of the lead, which is suspended from its anchor point in the myocardium, in contrast to leads inserted from the pectoral area. Correct positioning of the lead is therefore of the utmost importance. Active-fixation leads should not be considered securely attached without a proper current of injury.9
The main aim of positioning the electrocatheter in apical-septal position in our patient was to increase the amount of the lead housed in the ventricular cavity in order to attach it more firmly and maximize the area of subsequent adhesions, further increasing lead stability in the long term and reducing the risk of dislodgement.
In conclusion, pacemaker implantation via the femoral vein is a good alternative when subclavian vascular access is unavailable. It is associated with low morbidity and is easy to implement compared with other alternative implant techniques.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Tereno Valente B, Conceição JM, Nogueira da Silva M, et al. Acesso femoral venoso: uma alternativa excecional para a implantação de pacemaker definitivo. Rev Port Cardiol. 2014;33:311.e1–311.e5.