Takayasu arteritis is a large vessel vasculitis with various clinical presentations depending on the territories affected. We report the case of a 47-year-old woman who was diagnosed with Takayasu arteritis following rapid progression of coronary disease. The condition evolved rapidly under corticosteroid therapy, with formation of new arterial stenoses within the carotid and splanchnic circulations. Disease remission was achieved with cyclophosphamide pulses and percutaneous angioplasty of the affected vessels was performed.
A arterite de Takayasu é uma vasculite de grandes vasos que cursa com apresentações clínicas diversas consoante os territórios afetados. Apresenta-se o caso clínico de uma mulher de 47 anos a quem foi feito o diagnóstico de arterite de Takayasu na sequência de doença coronária rapidamente progressiva. O quadro evoluiu rapidamente, sob corticoterapia, com formação de estenoses a nível da circulação carotídea e esplâncnica, tendo-se conseguido estabilização da doença com pulsos de ciclofosfamida e angioplastia percutânea das lesões.
Takayasu arteritis is a rare vasculitis that mainly affects females before the age of 50.1 Clinical presentation varies according to the territories affected; the left subclavian artery is most often involved, followed by the aorta and the carotid, renal and vertebral arteries.2 Coronary artery involvement is well documented, but revascularization of coronary lesions is a challenge if the underlying disease is not controlled. Since there are no markers specific to the disease, in most cases diagnosis is based on identification of vascular lesions in imaging studies of patients with suggestive symptoms. Age of onset under 40, limb claudication, differences in pulses and systolic blood pressure between the arms, murmur over the subclavian arteries and stenosis of the great vessels on angiography are the diagnostic criteria used to distinguish Takayasu arteritis from the other vasculitides.1
Case reportWe report the case of a 47-year-old woman, white, with a history of hypertension and chronic iron deficiency anemia but no other known medical history. Three weeks before admission she began to suffer chest pain radiating to the jaw, relieved by rest. Following assessment at another institution she was prescribed aspirin, transdermal nitroglycerin and nebivolol and was referred for urgent cardiological consultation. Worsening symptoms in the previous 48 hours prompted her to go to the emergency department of our hospital, where on admission she was eupneic and hypertensive, with pain triggered by minimal exertion and a II/VI apical systolic murmur; there were no other alterations on physical examination. Laboratory tests showed normocytic normochromic anemia with hemoglobin 10.4 g/dl and elevated troponin (rising from 0.21 to 0.32 ng/dl). Serial ECGs revealed dynamic repolarization changes without ST-T segment elevation, while echocardiography showed mild concentric ventricular hypertrophy but no wall motion abnormalities, and ejection fraction was normal.
She was provisionally diagnosed with non-ST-elevation acute coronary syndrome and underwent urgent coronary angiography, which revealed stenosis in the ostium of the left main but no other lesions. During double bypass surgery (left internal mammary-anterior descending and saphenous vein-obtuse marginal), findings suggestive of aortitis were observed, and so a biopsy was performed, and anatomopathological study showed a nonspecific lymphoplasmacytic inflammatory infiltrate. Syphilis serology was negative. Postoperative recovery was uneventful and no further investigation was carried out.
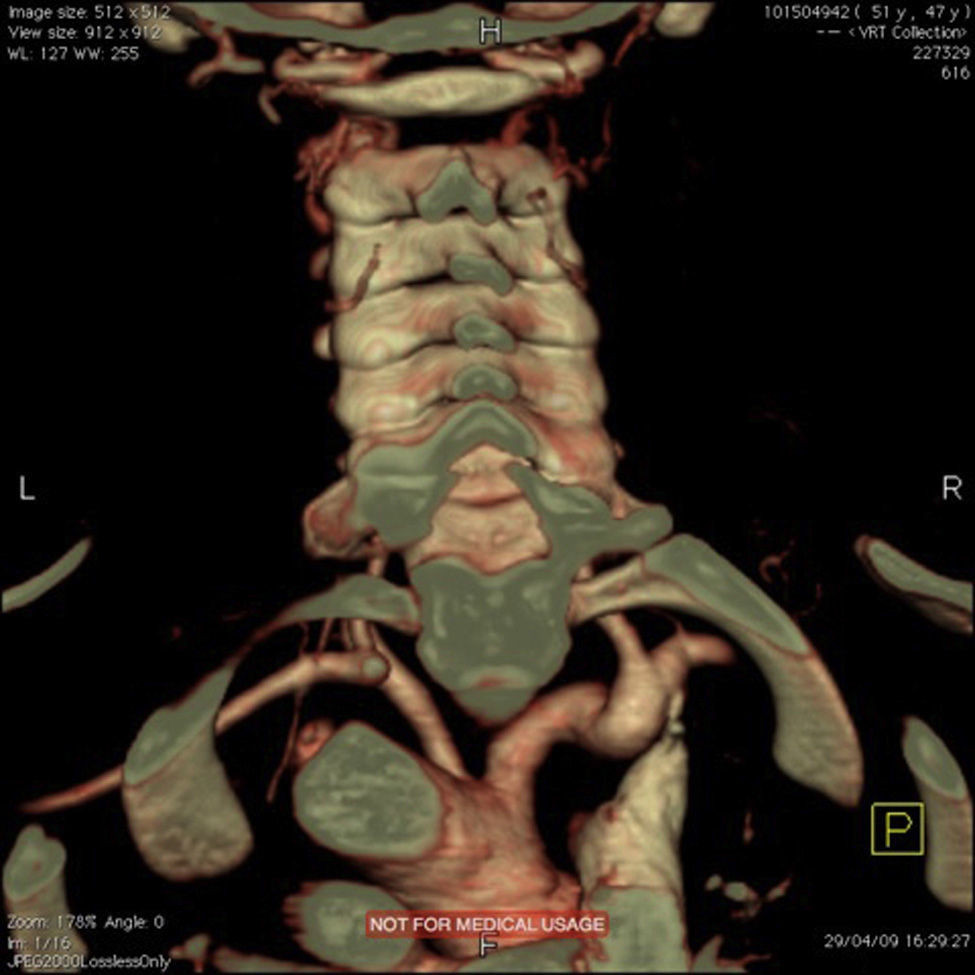
Around four months later, there was recurrence of exertional angina. At this time a difference in blood pressure between the arms was noted (20 mmHg less in the left arm), with a very weak pulse on the left and evident skin pallor immediately after exertion or when raising the left arm. Laboratory testing showed slight thrombocytosis and a rise in erythrocyte sedimentation rate to 100 mm/h. Echocardiography revealed new-onset hypokinesia of the left ventricular inferior wall, and coronary angiography was repeated, which showed preocclusive lesions of the right coronary artery and ostial saphenous graft. She underwent percutaneous coronary intervention with placement of two drug-eluting stents; during the procedure occlusion of the left subclavian artery was observed with retrograde filling from the ipsilateral vertebral artery (Figure 1), which raised the suspicion of Takayasu arteritis. Cranial computed tomography (CT) angiography confirmed proximal occlusion of the left subclavian artery upstream of the origin of the left vertebral artery (Figure 2), an atheromatous plaque in the distal segment of the right common carotid causing preocclusive stenosis of the external carotid, and tortuosity and kinking of the cervical course of the internal right carotid artery. Carotid Doppler ultrasound showed coiling of the right internal carotid and 70% stenosis, preocclusive stenosis of the right external carotid and reversal of flow in the left vertebral artery caused by left subclavian steal. Abdominal Doppler ultrasound detected no abnormalities in the renal arteries and the patient did not present nitrogen retention. In view of these findings and fulfillment of the diagnostic criteria, a diagnosis of Takayasu arteritis was made and therapy was begun with oral prednisolone 1 mg/kg/day.
She remained asymptomatic until around a month later, when she was readmitted twice in 15 days for acute hypertensive pulmonary edema. Laboratory tests revealed deterioration of renal function but inflammatory parameters were still normal. Stress echocardiography showed no wall motion abnormalities; given the suspicion of renal involvement of the vasculitis in view of persistent severe renal dysfunction despite optimization of blood volume and suspension of nephrotoxic medication, abdominal Doppler ultrasound was repeated. This showed the abdominal aorta with irregularly thickened walls but normal flow and stenotic lesions with marked hemodynamic repercussions at the origin of the superior mesenteric artery and left renal artery. Abdominal CT angiography confirmed the presence of a thin sheath of tissue surrounding the abdominal aorta, causing significant preocclusive stenosis of both renal arteries and the superior mesenteric aorta (Figure 3). Stenoses of around 50% were also detected in the inferior mesenteric artery and the celiac trunk.
Given the obvious progression of the disease under corticoid therapy, treatment with cyclophosphamide pulses was begun and angioplasty of the renal arteries and celiac trunk was performed, with a good angiographic result and complete recovery of renal function. The patient has remained under corticoid therapy, without further complications or evidence of disease progression in other arterial territories.
Discussion and ConclusionThe case described is a classic example of the severity of Takayasu arteritis and of the complexity of its diagnosis and treatment.
The disease typically presents in women aged under 50, although several recent series have reported a high prevalence in older age-groups.3
Its clinical presentation is varied; patients can be asymptomatic for several years and can present with nonspecific systemic symptoms such as fever, asthenia, arthralgia, myalgia and night sweats, and more rarely with acute vascular events.4 Depending on the arterial territory affected, there may be visual disturbances, headache, syncope, Raynaud phenomenon, limb claudication or differences in pulses and blood pressure between the arms.2,4
The clinical presentation in this case was coronary disease, which is seen in up to a third of Takayasu patients5 and is usually due to occlusion of the coronary ostia caused by aortitis, although several cases of coronary arteritis have been reported without ostial involvement.6,7 Its etiopathogenesis is unclear but some authors have suggested that as well as formation of stenoses, the inflammation itself accelerates coronary atherosclerosis.8
Hypertension is a common comorbidity, found in 33–83% of cases,4 linked to renal artery stenosis (observed in 20–38% of patients).6 Although there is disagreement concerning the treatment of these lesions, percutaneous angioplasty has shown good long-term results in terms of treating hypertension and improving renal function.2,6
The restenosis rate varies according to the location and degree of control of the disease. Interventions should preferably be performed outside periods of acute disease activity.9
Another important aspect of this case was disease progression under corticoid therapy, despite normalization of inflammatory parameters. Several authors have reported low sensitivity of laboratory monitoring in Takayasu arteritis and have suggested serial imaging studies to monitor disease progression.10,11 In around 50% of cases corticoid therapy alone is insufficient to halt progression of the vasculitis and additional immunosuppressive therapy is needed.2 In the case reported here, prolonged remission was achieved with cyclophosphamide pulses. There is no consensus concerning the best drug for corticoid-resistant disease; experience with cyclophosphamide in Takayasu arteritis is limited, unlike in other forms of vasculitis.6,12
This case report illustrates how Takayasu arteritis remains a diagnostic and therapeutic challenge.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Duque Neves B, Raimundo A, Appleton Figueira T, et al. Arterite de Takayasu: a propósito de um caso clínico. Rev Port Cardiol. 2015;34:215.e1–215.e4.