Coronary artery rupture is a rare but potentially fatal complication of percutaneous coronary intervention (PCI) that can result in life-threatening cardiac tamponade.
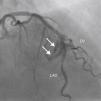
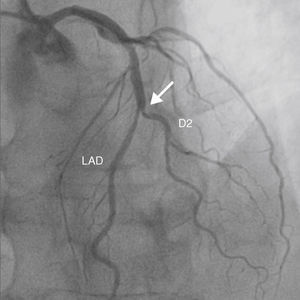
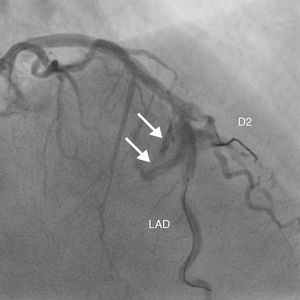
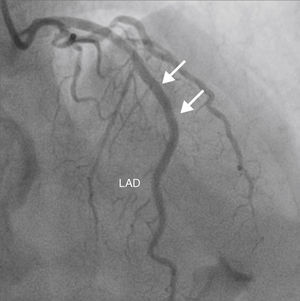
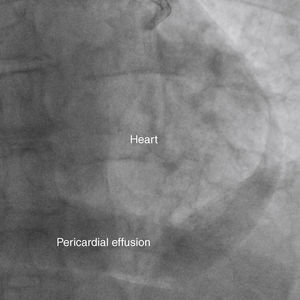
A 69-year-old man was referred for PCI of a 90% calcified lesion in the mid left anterior descending artery (LAD) involving the second diagonal branch (D2; Figure 1, arrow). After the left coronary ostium was cannulated and crossed with two BMW® wires, one to the LAD and other to the D2, predilation with a 2.5 mm×15mm Trek® balloon was performed and an unsuccessful attempt was made to cross the stenosis with a 2.75 mm×22mm Resolute Integrity® drug-eluting stent. Predilation was repeated with a 2.75 mm×15mm Trek® non-compliant balloon at high pressure. Suddenly, balloon rupture was detected and the angiogram showed LAD rupture with extensive contrast extravasation into the pericardium (Figure 2, arrows; Video 1). Protamine sulfate was used to reverse the effect of heparin and the drug-eluting stent was deployed with balloon inflation for 10minutes to seal the type III perforation but, as dye extrava- sation persisted, a 3.0 mm×19mm GraftMaster® covered stent was superimposed, followed by rapid cessation of contrast leakage (Video 2). The D2 branch was lost (Figure 3, arrows), and periprocedural myocardial infarction occurred. The final image showed pericardial effusion (Figure 4; Video 3). The echocardiogram excluded tamponade. Forty-eight hours later, atrial fibrillation occurred with hemodynamic deterioration. Pericardiocentesis was performed and 50ml of serosanguineous fluid was drained. Sinus rhythm was restored, with favorable evolution thereafter.
Treating calcified bifurcated lesions with balloons at high pressure must be performed with caution. If grade III per- foration occurs, a standard stent can be used to save the side branch, although this is only successful in a minority of patients.
Ethical disclosuresProtection of human and animal subjects. The authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publica- tion of patient data.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.repc. 2014.11.006.