A 49-year-old man was admitted to the emergency department suffering from a large anterior myocardial infarction that was treated by rescue PCI. The patient also had a moderate but complex lesion in the proximal segment of the right coronary artery. Optical coherence tomography showed striking images of a ruptured and ulcerated plaque with significant thrombus content. Although the lumen was not compromised, these unique findings prompted us to treat this non-culprit lesion. We selected a bioresorbable vascular scaffold with the aim of sealing and passivating this complicated and high-risk plaque.
Homem de 49 anos, admitido no serviço de urgência, que padecia de enfarte do miocárdio anterior extenso e que tinha sido tratado com intervenção coronária percutânea (ICP) de recurso. O doente também apresentou lesão moderada mas complexa no segmento mais próximo da coronária direita. A tomografia de coerência óptica revelou imagens impressionantes de uma placa com rotura e ulcerada com trombos significativos. Embora o lúmen não tenha sido comprometido, estas constatações únicas levaram-nos a tratar rapidamente esta lesão não culpada. Selecionámos um suporte vascular bioabsorbível com o objetivo de selar e de solucionar o caso desta placa complicada e de alto risco.
A 49-year-old man, a smoker and with hypertension and dyslipidemia, was admitted to the emergency department for rescue primary angioplasty. Marked anterior ST-segment elevation (5 mm in leads V2-V4) was seen on the ECG. Coronary angiography showed a critical coronary lesion in the mid segment of the left anterior descending coronary artery in which a 2.75 mm×13 mm bare-metal stent was successfully implanted. The right coronary artery showed a complex but moderate lesion in its proximal segment.
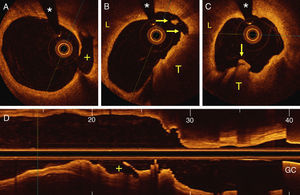
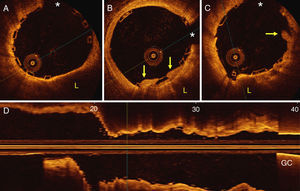
Two days later, a new coronary angiogram was performed to further assess the proximal right coronary lesion. Optical coherence tomography (OCT) disclosed a large thin-cap fibroatheroma with a clear fibrous-cap rupture and a large cavity along the direction of coronary flow (Figure 1). Several coronary thrombi were also detected. Although the lumen area was relatively preserved, these unique OCT findings of active plaque complication were instrumental in the decision to treat this lesion. A bioresorbable vascular scaffold (BVS) was successfully implanted (Figure 2).
Optical coherence tomography. (A) A ruptured cap and a large posterior cavity (+) are visualized; (B and C) images showing a lipid plaque (L) and a large red thrombus (T) protruding into the coronary lumen (arrows); (D) longitudinal reconstruction highlighting the ruptured plaque cavity (+) in the flow direction. GC: guiding catheter; *: wire artefact.
Optical coherence tomography images after intervention. (A) A large residual thin-cap fibroatheroma is partially visualized behind the scaffold; (B and C) a residual thrombus (arrows) protruding slightly into the lumen and a lipid plaque (L) are also visualized; (D) longitudinal image showing a fully expanded scaffold. GC: guiding catheter; *: wire artefact.
Multivessel coronary artery disease is present in nearly half of patients with acute myocardial infarction undergoing primary angioplasty.1 The optimal timing for the treatment of non-culprit lesions in these patients remains controversial, although a staged procedure is frequently selected following current recommendations.2 Only severe coronary lesions are treated during these repeat procedures. However, intracoronary imaging techniques have demonstrated that many patients with acute myocardial infarction also have complicated plaques in non-culprit lesions. Notably, some of these complicated plaques are not identified by angiography. OCT provides novel insights in this regard as its unique resolution enables the presence of plaque rupture with associated intracoronary thrombus to be readily identified.3 In our patient, angiography showed a complex but moderate lesion in the proximal right coronary artery, but OCT disclosed the presence of a large complicated thin-cap fibroatheroma with a large rupture associated with intracoronary thrombi. We used a BVS to treat this complicated plaque, in spite of a relatively large residual minimal lumen area, with excellent results. BVS are especially attractive to seal and passivate vulnerable coronary plaques, as these devices may lead to complete vessel wall restoration at late follow-up.4 Although there is little evidence to support this strategy, further studies are warranted to answer this important clinical question. Whether the additional information provided by OCT can help guide interventions in non-culprit lesions in patients presenting with an acute myocardial infarction deserves a prospective evaluation.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.