Brugada syndrome is a rare syndrome, with an estimated prevalence in Europe of 1–5/10000 population, whose initial clinical presentation can be sudden death. Although it has a characteristic electrocardiographic pattern, this can be intermittent. The authors present the case of a 32-year-old man, with no family history of syncope or sudden death, who went to the emergency department for syncope without prodromes. The initial electrocardiogram (ECG) in sinus rhythm documented an isolated and non-specific ST-segment elevation in V2. During further diagnostic studies, a repeat ECG revealed type 1 Brugada pattern. This pattern was later seen in a more marked form during a respiratory infection. The patient subsequently underwent electrophysiological study, followed by implantation of an implantable cardioverter-defibrillator (ICD), with an episode of ventricular fibrillation converted via ICD shock two months after implantation.
A síndrome de Brugada é uma síndrome rara, com uma prevalência aproximada na Europa de 1-5/10 000 habitantes, mas cuja apresentação clínica inicial pode ser morte súbita. Embora com um padrão eletrocardiográfico típico, este é por vezes intermitente. Os autores apresentam o caso clínico de um doente de sexo masculino, de 32 anos, sem fatores de risco pessoais conhecidos e história familiar de morte súbita, que recorre ao Serviço de Urgência por síncope sem pródromos. O primeiro eletrocardiograma (ECG) em ritmo sinusal documenta a presença de uma elevação isolada e inespecífica do segmento ST em V2. Da restante investigação diagnóstica realizada, salienta-se a repetição do ECG, que revelou a presença de padrão de Brugada tipo 1. Este mesmo padrão é exacerbado posteriormente numa situação de infeção respiratória. O doente foi submetido a estudo eletrofisiológico, seguido de implantação de cardiodesfibrilhador (CDI), tendo tido um episódio de fibrilhação ventricular convertido com choque via CDI 2 meses após a implantação.
Brugada syndrome, first described in 1992, is a rare syndrome with an estimated prevalence in Europe of 1–5/10 000 population, but which has a strong social and media impact since the first clinical manifestation can be sudden death. It is a hereditary arrhythmogenic disease, characterized by right bundle branch block and downsloping ST-segment elevation in the right precordial leads V1–V3 on the electrocardiogram (ECG).1 However, this ECG pattern is dynamic and may be revealed or mimicked by various clinical and pharmacological situations such as fever syndrome, hypo- or hyperkalemia, or the use of sodium channel blockers.2
Case reportA 32-year-old man, with no relevant personal or family cardiovascular history, went to the emergency department (ED) for syncope at rest, without prodromes or previous symptoms, lasting two minutes and with spontaneous recovery. Physical examination revealed no relevant alterations; blood pressure was 104/58 mmHg and heart rate 76 bpm.
Standard 12-lead ECG at admission showed sinus rhythm, heart rate 60 bpm, 1-mm J-point elevation with downsloping ST in V1 and 1-mm horizontal ST elevation in V2, with no other alterations (Figure 1). The patient was monitored in the ED for clarification of the syncopal episode, but no extrasystoles or other arrhythmia were documented.
Repeat ECG 24 hours later showed sinus rhythm with heart rate of 60 bpm, and incomplete right bundle branch block with downsloping ST-segment elevation in V1 and V2, compatible with type 1 Brugada pattern (Figure 2).
Echocardiography showed no left ventricular dilatation or wall thickening, good global systolic function and regional wall motion, no left atrial or right chamber dilatation, and no valve abnormalities or other relevant alterations.
Given the presence of Brugada syndrome and syncope, the patient was referred to the arrhythmology clinic. The ECG performed at that time was similar to that shown in Figure 1, but the patient had brought another ECG performed in the context of fever accompanied by cough and expectoration, which showed a more marked type 1 Brugada pattern (Figure 3).
He subsequently underwent electrophysiological study (EPS) for risk stratification, which showed the following intervals: AH 96 ms; HH 31 ms; and HV 51 ms. No ventricular arrhythmia was induced following right ventricular apical stimulation up to S4 extrastimuli (200 ms).
Despite the fact that no ventricular arrhythmia was induced during EPS, current guidelines recommend an implantable cardioverter-defibrillator (ICD) in cases of syncope and spontaneous type 1 Brugada ECG pattern.1 The patient accordingly underwent implantation of a Biotronik® Lumax 340 VR-T XI ICD for primary prevention.
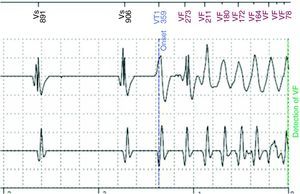
Around two months after ICD implantation, an episode of ventricular fibrillation (VF) (Figure 4) was converted via a 40-J ICD shock.
DiscussionBrugada syndrome is a primary electrical disturbance in patients with structurally normal hearts and is often associated with sudden cardiac death. It is a hereditary disease of autosomal dominant transmission,3 and mutations in the SCN5A gene (which encodes cardiac sodium channels) are identified in around a quarter of patients. The phenotypic expression of these alterations is characterized by an ECG pattern of right bundle branch block accompanied by downsloping ST-segment elevation in the right precordial leads.1,3 However, the pattern is intermittent and can be triggered by various clinical or pharmacological factors, particularly those that affect cardiac sodium channels.2
This intermittent pattern was observed in our patient, in whom the initial ECG in the ED showed 1-mm J-point elevation with downsloping ST in V1 and 1-mm horizontal ST elevation in V2 (without classic Brugada criteria), and only on the second ECG was a typical type 1 Brugada pattern observed. A more marked form of this pattern was seen during a respiratory infection. There have been reports of the Brugada pattern being precipitated by fever syndrome and hypo- or hyperkalemia.2,4
According to the guidelines on management of the Brugada syndrome, the occurrence of syncope in a patient with type 1 Brugada ECG pattern should prompt implantation of an ICD, as in our patient.
The patient underwent EPS prior to ICD implantation, during which no ventricular arrhythmia was induced. EPS in patients with Brugada syndrome is still the subject of debate as there is no consensus on indications for the exam or on the prognostic value of the results. This is partly due to the lack of a standard electrical stimulation protocol for EPS in Brugada syndrome.5 According to Brugada et al.,6 induction of ventricular tachycardia (VT) and/or VF in Brugada patients is a strong predictor of VT/VF and sudden death. The predictive value of EPS in stratifying these patients was also demonstrated by Giustetto et al., who prospectively studied the incidence of arrhythmic events in 166 patients with type 1 Brugada ECG pattern and found that the only predictors were syncope, aborted sudden death and positive EPS.7 However, according to Priori et al., VT or VF inducibility on EPS did not predict malignant arrhythmias or sudden death,8 and along the same lines, Gehi et al. concluded that EPS did not add relevant information for the management of patients with Brugada syndrome.9 Furthermore, multivariate analysis of the largest registry of Brugada patients, the FINGER Brugada Syndrome Registry, showed that EPS results were not predictive of time to first arrhythmic event.10
These conflicting results are illustrated by the case presented, in which an ICD was implanted despite no VT or VF being induced during EPS, two months after which the patient had an episode of VF converted via a 40-J ICD shock.
The present case highlights the fact that the Brugada ECG pattern is often intermittent and can be triggered by various situations, including fever syndrome. In addition, the fact that the patient had an episode of VF when previous EPS had failed to trigger any arrhythmia is a practical demonstration of the controversy surrounding the prognostic value of this exam in risk stratification of Brugada patients, and highlights the need for standardization of patient selection for EPS and of the stimulation protocols employed.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Cordeiro Piçarra B, et al. Síncope e padrão de Brugada intermitente. Rev Port Cardiol 2013. http://dx.doi.org/10.1016/j.repc.2013.02.002.