Hypertension is an important cardiovascular risk factor and although there have been many improvements in pharmacological treatment, a significant percentage of patients are still considered resistant. The authors describe two cases of radiofrequency renal sympathetic denervation that illustrate the feasibility of this new technique for the treatment of resistant hypertension. The procedure consists of the application of radiofrequency energy inside the renal arteries to ablate afferent and efferent sympathetic renal activity, which has been implicated in the pathophysiology of hypertension.
A hipertensão arterial é um importante fator de risco cardiovascular e apesar dos inúmeros avanços na terapêutica farmacológica, existe ainda uma percentagem importante de doentes que são resistentes. Os autores descrevem 2 casos clínicos de ablação da atividade simpática renal por radiofrequência, que ilustram a exequibilidade de uma nova técnica para o tratamento da hipertensão arterial resistente. O procedimento consiste na aplicação de energia de radiofrequência nas artérias renais, para ablação da atividade simpática renal aferente e eferente, implicada na fisiopatologia da hipertensão arterial.
Hypertension is an important cardiovascular risk factor that is implicated in myocardial infarction and stroke, which are major causes of mortality and morbidity in developed countries.1 Despite its high prevalence, hypertension is far from being controlled, as shown by the PAP study on the prevalence, awareness, treatment and control of hypertension in Portugal.2 This study, performed in 2003, found an overall hypertension prevalence of 42.1%, and only 46.1% of these patients knew they were hypertensive, 39.0% were taking antihypertensive medication and only 11.2% were controlled.
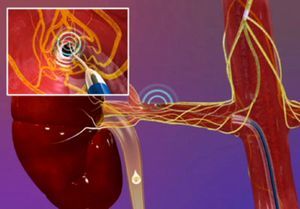
A technique has recently been developed to treat resistant hypertension by modulating renal sympathetic nerve activity using radiofrequency ablation.3–5 The aim of the procedure is to reduce afferent and efferent nerve activity of the renal sympathetic plexus (Figure 1), whose role and importance in the pathophysiology of hypertension has been recognized for several decades.6,7 The efficacy and safety of the technique was first documented in the Symplicity HTN-1 trial,4 and a recently published 24-month follow-up study reported a fall of 32mmHg in systolic blood pressure (BP) and 14mmHg in diastolic BP.8 The Symplicity HTN-2 randomized trial documented a reduction of 32mmHg in systolic BP and 12mmHg in diastolic BP at six months, with no significant changes in the control group, in a population of patients with mean baseline BP of 178/98mmHg, medicated with an average of five antihypertensive drugs.5
This article presents two case reports of treatment of resistant hypertension by radiofrequency ablation of renal sympathetic activity. The procedures were approved by the hospital's ethics committee and performed with the patients’ informed consent.
Case report 1A 50-year-old black man, a smoker, with no previous cardiovascular events, was being treated in the hypertension clinic. Secondary causes of hypertension had been ruled out. He was medicated with clonidine (0.45mg/day), irbesartan (300mg/day), amlodipine (10mg/day), indapamide (1.5mg/day) and bisoprolol (5mg/day). Renal function was normal, with estimated glomerular filtration rate (eGFR) of 115ml/min/1.73m2.
His BP at the last consultation prior to the procedure was 173/118mmHg, and 189/143mmHg at the time of admission, despite his usual therapy. In a previous exercise test under medication, his BP had risen from 160/100mmHg at rest to 200/120mmHg at peak exercise. Echocardiography documented concentric left ventricular hypertrophy, with normal global systolic function and no significant valve abnormalities. Ambulatory BP monitoring (ABPM) showed severe systolic and diastolic hypertension and a nondipper pattern (daytime: 145/104/118/41mmHg; nighttime: 136/96/111/40mmHg; mean systolic and diastolic BP, mean BP and pulse pressure, respectively).
Previous abdominal CT angiography showed favorable renal artery anatomy for the procedure.
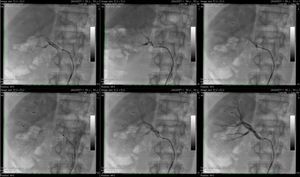
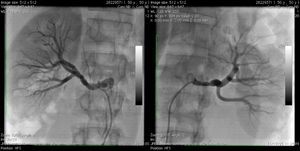
The procedure was performed with anesthesia support (propofol and remifentanil) for pain control, and anticoagulation with heparin for a target activated clotting time of >250s. After gaining vascular access via the right femoral artery, abdominal aortography and selective renal artery angiography were performed. Following catheterization, a Symplicity® catheter (Medtronic, USA) was inserted into each renal artery, connected to a radiofrequency generator that is programmed and controlled automatically, independent of the operator (Figure 2). Six applications of radiofrequency energy (8W) lasting 120s each were performed in the right and left renal arteries (Figures 3 and 4). Fluoroscopy time was 13min, the quantity of contrast was 70ml, and total procedure time was 53min. There were no complications related to the intervention. Renal angiography at the end of the procedure showed normal flow and no signs of dissection; some irregularities in the luminal contour were observed due to edema at the ablation sites, as is common in such procedures (Figure 5).
At the end of the procedure, the access site was closed using an Angio-Seal® device. There were no post-procedural complications and the patient was discharged the following day; he continues to be monitored in the hypertension clinic, beta-blocker therapy having been discontinued. His BP was 150/86mmHg one month after the procedure, a reduction of 23mmHg in systolic BP and 32mmHg in diastolic BP compared to before the intervention and with one less drug class. Renal function showed no significant changes following the procedure, with eGFR of 123ml/min/1.73m2.
The patient is scheduled to undergo ABPM at three and six months, and renal CT angiography at six months.
Case report 2A 59-year-old white woman, obese (body mass index 32), with type 2 diabetes, was being treated in the hypertension clinic. Secondary causes of hypertension had been ruled out. She was medicated with aliskiren (300mg/day), lercanidipine (10mg/day), enalapril (10mg/day), furosemide (40mg/day), spironolactone (50mg/day) and carvedilol (50mg/day). The patient had known atherosclerotic disease, with coronary involvement (angioplasty of the anterior descending artery for stable coronary disease) and cerebrovascular disease (previous ischemic stroke). Renal function was normal for her age (eGFR of 85ml/min/1.73m2).
Her BP at the last consultation prior to the procedure was 194/84mmHg, and 203/89mmHg at the time of admission. Echocardiography documented concentric left ventricular hypertrophy, with normal global systolic function and no significant valve abnormalities. ABPM showed systolic and diastolic hypertension, with marked elevation of systolic load and a nondipper pattern (daytime: 174/84/113/90mmHg; nighttime: 157/79/107/78mmHg; mean systolic and diastolic BP, mean BP and pulse pressure, respectively).
Selective catheterization of the renal arteries excluded stenosis and confirmed favorable anatomy for the procedure.
The procedure was similar to that described for the previous patient, with vascular access via the right femoral artery and six radiofrequency ablations in each renal artery. Fluoroscopy time was 9min, the quantity of contrast (low-osmolarity – Visipaque 320mgI/ml) was 60ml, and total procedure time was 46min. At the end of the procedure, the access site was closed using an Angio-Seal® device. There were no complications and the patient was discharged the following day. On assessment one month after the procedure, having discontinued beta-blocker therapy, her BP was 166/70mmHg, which compared to levels prior to the intervention represented a reduction of 28mmHg in systolic BP and 14mmHg in diastolic BP, and taking one less drug class. Renal function showed no significant changes following the procedure, with eGFR of 83ml/min/1.73m2.
The patient is scheduled to undergo ABPM at three and six months, and renal CT angiography at six months.
DiscussionThese two cases illustrate the feasibility of renal sympathetic nerve ablation to treat resistant hypertension and the importance of a multidisciplinary approach in this new percutaneous treatment. The patients were assessed by a nephrologist prior to the procedure, clinical and anatomical criteria being applied in selecting patients for the treatment.
The clinical criteria were a diagnosis of resistant hypertension, defined as systolic BP≥160mmHg in two or more measurements during a consultation, under therapy with four or more antihypertensive drugs (including a diuretic), and exclusion of secondary causes of hypertension. The anatomical criteria were renal artery diameter≥4mm and length≥20mm and absence of anatomical abnormalities (extreme tortuosity or stenosis) or previous intervention in the renal arteries. Renal anatomy should be assessed by angiography (CT, magnetic resonance or catheterization) prior to the procedure.
Various registries and clinical trials have demonstrated the efficacy and safety of this technique. A multicenter randomized trial (Symplicity HTN-2) involving 106 patients with resistant hypertension reported a fall of 32mmHg in systolic BP and 12mmHg in diastolic BP at six months in the group undergoing ablation.5 An inclusion criterion of this trial was that patients should be taking three or more antihypertensive drugs (including a diuretic) and the reported reduction in BP levels was obtained with patients maintaining previous treatment, as stipulated by the trial's protocol. However, the study population was medicated with 5.3 drugs on average, and so we decided to include patients medicated with four or more antihypertensive drugs. As this was our initial experience, in the two cases presented here, it was also decided to suspend beta-blocker therapy after the procedure as a precaution against the possible additive effect of both medication and ablation of sympathetic activity, the impact of which on afferent pathways could lead to a reduction in systemic sympathetic tone.
The technique's efficacy is due to the reduction in afferent and efferent sympathetic activity, which plays an important role in the pathophysiology of hypertension. Stimulation of the renal efferent nerves increases renin production, leading to activation of the renin–angiotensin–aldosterone system, sodium retention and diminished renal blood flow. At the same time, increased afferent nerve activity stimulates central sympathetic drive, which in turn is implicated in the pathophysiology of other clinical entities, notably insulin resistance,9 left ventricular hypertrophy, heart failure and sleep apnea.10 These conditions may also be improved by renal artery ablation, increasing the benefit of BP control and widening the range of potential applications of this technique.
ConclusionsThese two cases illustrate the feasibility of a new technique in interventional cardiology for the treatment of resistant hypertension, first used in Portugal in July 2011. It is based on radiofrequency ablation of renal sympathetic activity, which has proved extremely promising in recently published multicenter clinical trials.
Conflict of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Araújo Gonçalves, P; Ablação da actividade simpática renal para tratamento da hipertensão arterial resistente. Rev Port Cardiol 2012. doi:10.1016/j.repc.2012.02.016.